Trail mix is a favorite snack for many individuals. A typical mix combines granola, dried fruits, nuts, seeds, cereals, and pretzels. The mix was originally developed as a portable snack/meal for hikers that was lightweight, could be stored in a backpack, and provided plenty of protein and energy. Prepackaged trail mix is available at many grocery stores and online retailers. It’s an excellent choice for traveling or going on a road trip because of its energy and nutritional content. However, not all types are considered equal in terms of nutrition. Some can consist of ingredients loaded with sugar and salt. Added consumption could cause weight gain and contribute to conditions like heart disease, type 2 diabetes, and liver problems. Here we look at choosing healthy mixes.
Table of Contents
Trail Mix
The nutritional power comes from the high amounts of fiber and antioxidants.
Benefits
Protein and Healthy Fats
Protein is essential for tissue repair, immune health, and muscle development.
- Nuts and seeds make up the largest portion.
- A healthy source of protein, allowing individuals to snack on the go and not become hungry.
- One of the greatest benefits of eating these is that they are full of heart-healthy fats.
- These healthy fats help decrease unhealthy LDL cholesterol levels and reduce inflammation.
Fiber
- The fiber in the seeds and granola helps keep the gut healthy and regular.
- It also helps control appetite, aids in digestion, and keeps the body fuller longer.
Energy
- Dried fruits and granola consist of healthy sugars.
- Healthy sugars help stabilize blood sugar levels, providing the body with a consistent energy source.
Antioxidants, Vitamins, and Minerals
- Dried fruit maintains a majority of its nutritional value.
- The nuts and seeds are also packed with nutrients and antioxidants.
Choosing Healthy
Check the nutrition label and avoid varieties high in added sugar or sodium.
- Look for products containing nutrient-dense ingredients like nuts, seeds, dried fruits, and limited amounts of candy or chocolate chips, if any.
- Healthy ingredients include almonds, pumpkin seeds, cashews, sunflower seeds, dried fruit, popcorn, and dark chocolate.
- Making trail mix at home allows control of its contents and maximizes its potential health benefits.
- It is important to keep an eye on portion control.
- A recommended serving is about a fourth of a cup.
Nutritionist
Nutritional consultation can improve an individual’s quality of life, health, and well-being. A nutritionist can help individuals with precision or personalized nutrition that focuses on the individual. Nutritionists can create meal plans for their clients and provide education and knowledge on appropriate food choices.
Potassium
References
Devitt, A A et al. “Appetitive and Dietary Effects of Consuming an Energy-Dense Food (Peanuts) with or between Meals by Snackers and Nonsnackers.” Journal of nutrition and metabolism vol. 2011 (2011): 928352. doi:10.1155/2011/928352
Grillo, Andrea et al. “Sodium Intake and Hypertension.” Nutrients vol. 11,9 1970. 21 Aug. 2019, doi:10.3390/nu11091970
Mehlhose, Clara, et al. “PACE Labels on Healthy and Unhealthy Snack Products in a Laboratory Shopping Setting: Perception, Visual Attention, and Product Choice.” Foods (Basel, Switzerland) vol. 10,4 904. 20 Apr. 2021, doi:10.3390/foods10040904
Vreman, Rick A et al. “Health and economic benefits of reducing sugar intake in the USA, including effects via non-alcoholic fatty liver disease: a microsimulation model.” BMJ open vol. 7,8 e013543. 3 Aug. 2017, doi:10.1136/bmjopen-2016-013543















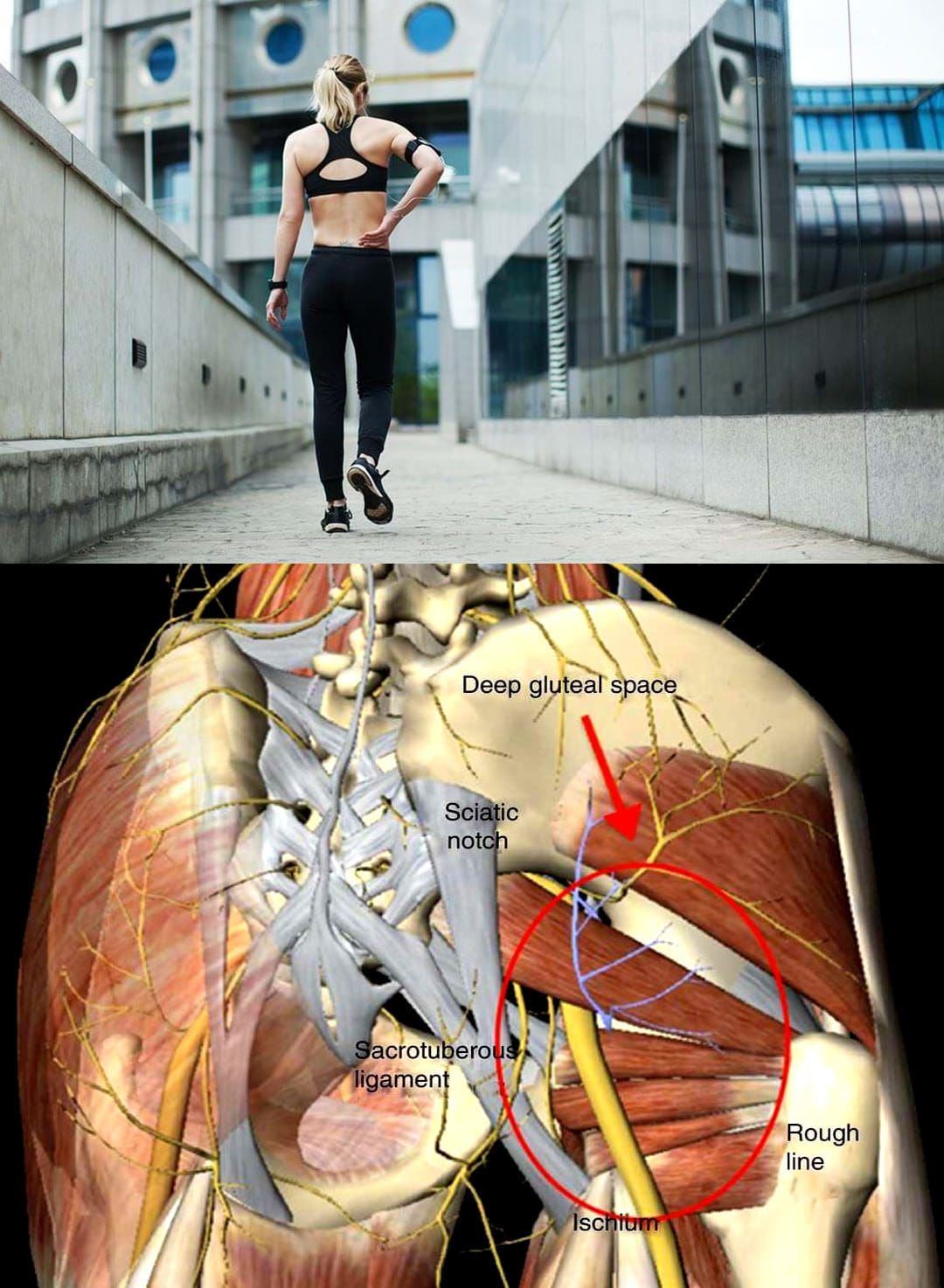
 Whiplash Nerve Injury
Whiplash Nerve Injury
















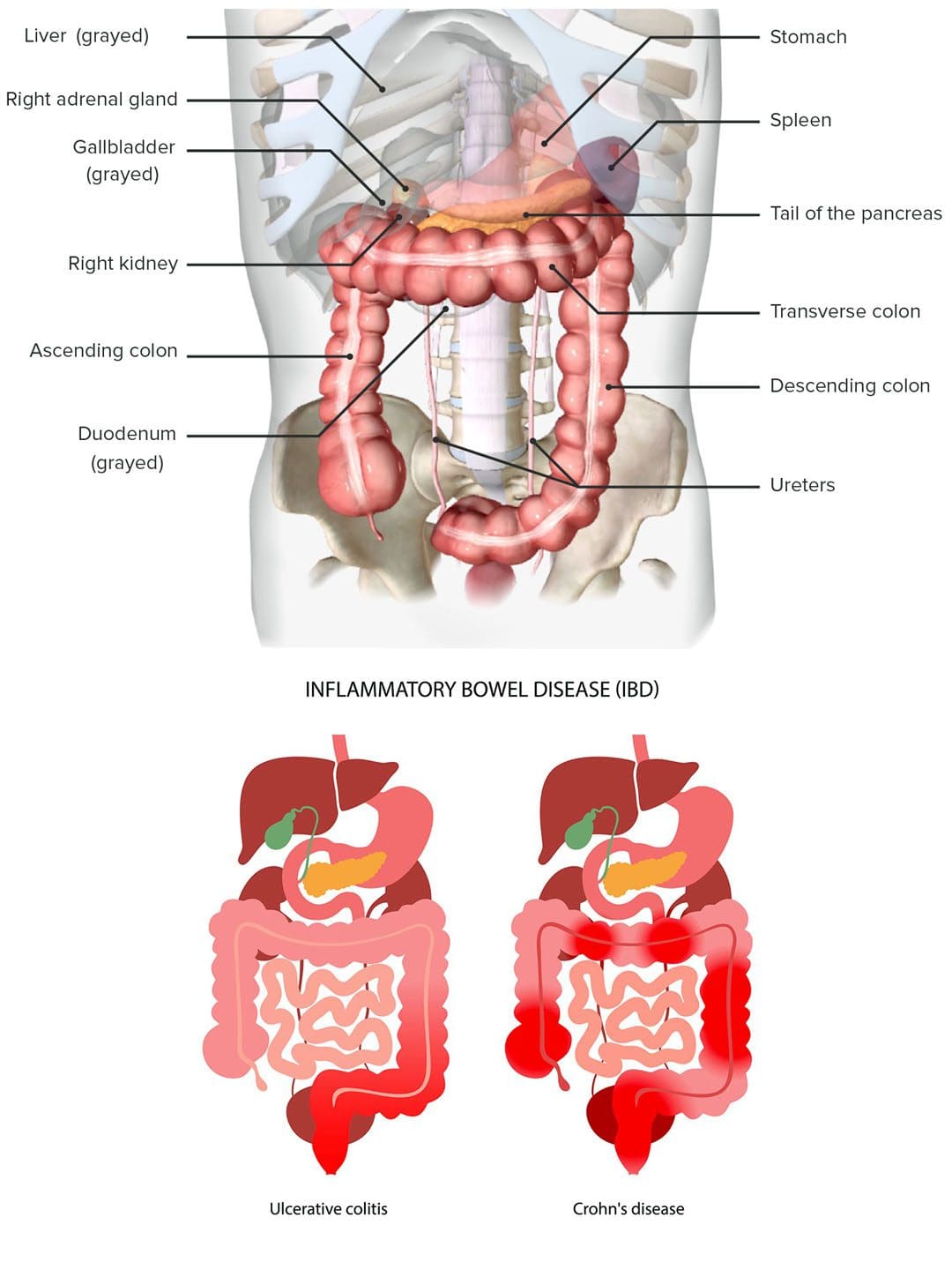 IBD Back Pain
IBD Back Pain
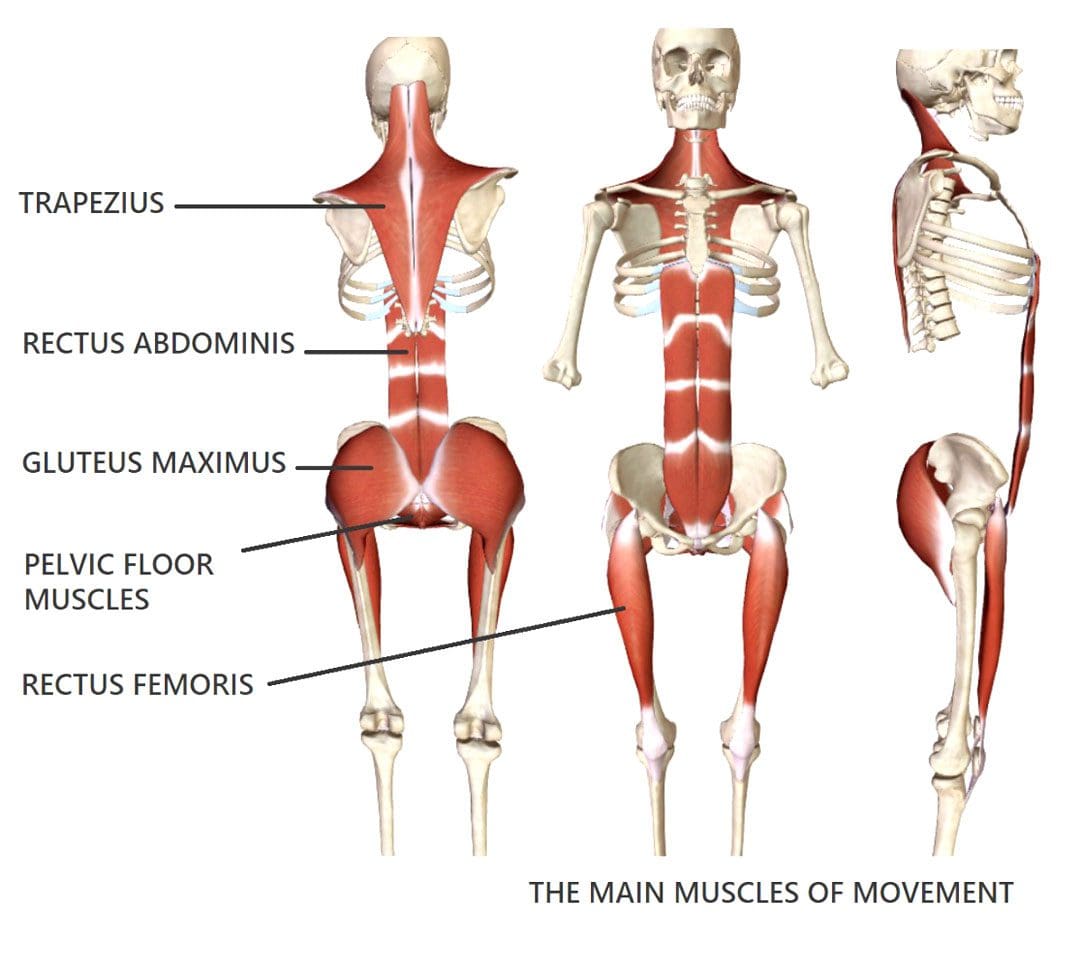 Posture Adjustments
Posture Adjustments