Table of Contents
Introduction
In the body, the digestive system makes sure that the food that is being consumed is digested in the gastrointestinal (GI) tract and the nutrients, minerals, and vitamins are being transported all throughout the entire body. Once that is done, the excess unused food is excreted out to avoid any issues that the gut or the body has encountered. Most of the time, the food a person eats can cause gut issues in the stomach and if a person continues to consume the same food, it can cause inflammation in the gut. When this happens, the inflammatory cytokines will attach themselves to the gut intestinal permeability and the immune system will begin to attack the intestinal permeability causing the toxins and gut bacteria to leak out and progress the gut inflammation further turning into IBD (inflammatory bowel disease). In this 2 part series, we will be taking a look at the pathophysiology of IBD (inflammatory bowel disease) and how its symptoms affect the gut system. Part 2 will be taking a look at how IBD affects the other organs and what kind of therapeutic treatments can help dampen the symptoms of IBD. By referring patients to qualified and skilled providers who specialize in gastroenterology services. To that end, and when appropriate, we advise our patients to refer to our associated medical providers based on their examination. We find that education is the key to asking valuable questions to our providers. Dr. Alex Jimenez DC provides this information as an educational service only. Disclaimer
Can my insurance cover it? Yes, it may. If you are uncertain, here is the link to all the insurance providers we cover. If you have any questions, please call Dr. Jimenez at 915-850-0900.
What Is IBD?
IBD or inflammatory bowel disease is when the digestive tract has chronic inflammation all over the digestive tract. When inflammation is in the body, it can be beneficial and harmful, depending on how severe it is. When inflammation is in its acute form, the immune system will send out the inflammatory cytokines to the injured area of the body, where it will attack the pathogen, causing the affected area to be red and hot to the touch for a few minutes to hours, depending on how severe it is. In its chronic state, however, inflammation can be caused either by a food allergen or sensitivity that can upset the gut system, an acute inflammation that hasn’t been treated, a person who has been exposed to toxins, or even an autoimmune disorder that can affect the body. When these factors start to cause the immune system to attack the healthy tissues like the gut permeability, it can lead to IBD. Research studies have shown that the exact cause of IBD is unknown, but factors can cause IBD to progress and aggravate the gut to develop IBD. Some of the risk factors that can exacerbate IBD are:
- Age
- Family history
- Environmental triggers
- Compromised immune system
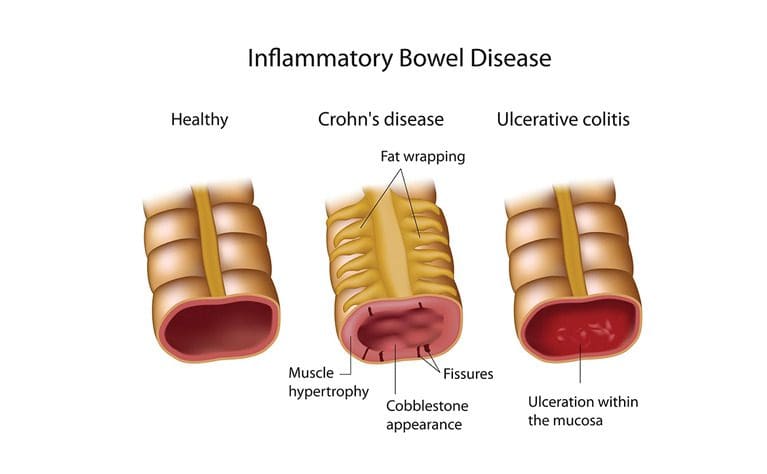
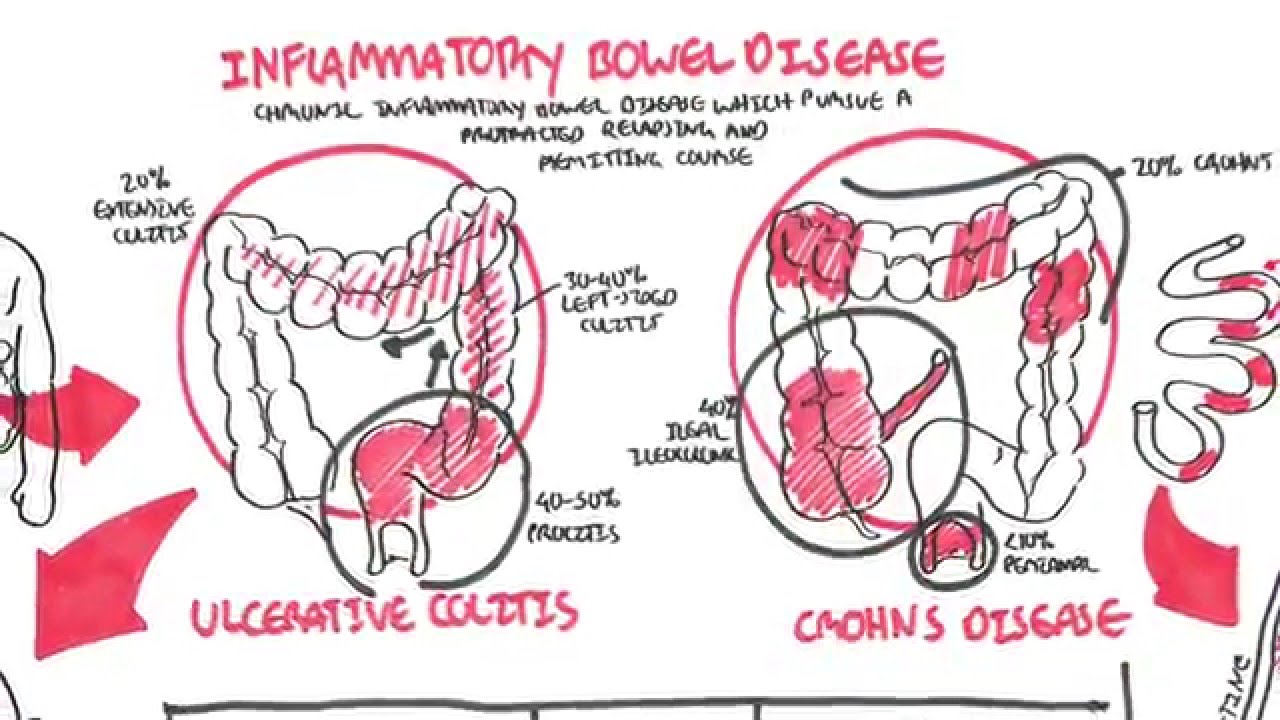
Other research studies have found that IBD is defined as chronic intestinal inflammation of the small and large intestines causing the body’s immune system to attack the digestive system, thus encompassing two primary inflammatory forms known as Crohn’s disease and ulcerative colitis. When chronic inflammation in the gut, the epithelial cells are secreted out of the intestinal wall lining, causing the immune system to attack the intestines. This will lead to the development of Crohn’s disease and ulcerative colitis.
Crohn’s Disease
Research studies have shown that Crohn’s disease is a type of IBD that causes inflammation in different areas of the digestive tract in other individuals. This chronic inflammation can often spread into deeper layers of the intestinal bowels. It can be painful, leading to life-threatening situations for some individuals with Crohn’s disease. The pathophysiology of Crohn’s disease is due to how it is multifactorial as studies have found that Crohn’s disease has the characteristics of transmural inflammation that affects the entire GI tract causing granuloma formation. What this does is that granuloma formation from Crohn’s disease causes ongoing inflammation in the GI tract and scarring to the bowel structure. Other studies have shown that the factors for Crohn’s disease can include a person’s age, family history, environmental factors, and other chronic disorders that can cause Crohn’s disease to progress further in the body, causing the individual to be in constant pain.
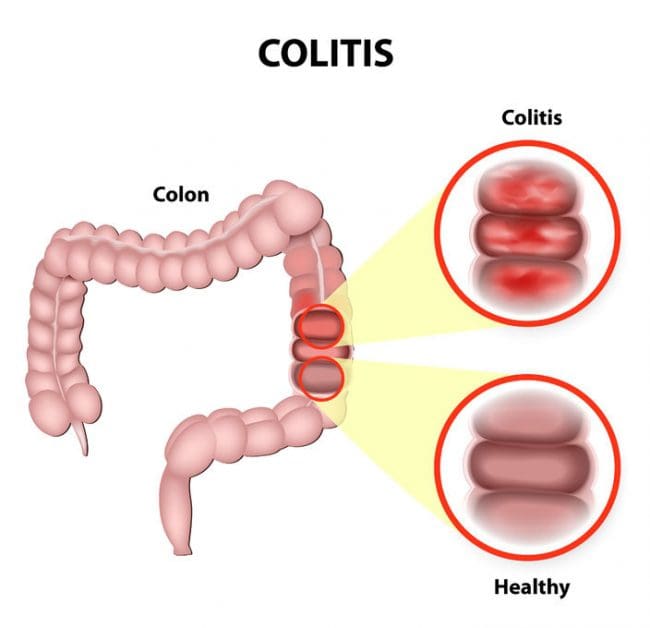
Ulcerative Colitis
Ulcerative colitis is another form of IBD that is an idiopathic inflammatory condition that causes diffuse friability and superficial erosion of the colonic walls and can cause the colon to bleed, as studies show. What ulcerative colitis does to the gut system is that it affects the large intestines or the colon by causing irritation and ulcers around the colon, making it very uncomfortable for individuals. Research studies show that ulcerative colitis causes inflammation of the rectum and can spread all over the colon, causing another form of ulcerative colitis known as ulcerative proctitis. The other conditions of ulcerative colitis are chronic as they affect the colon and can be severe depending on the location and the amount of inflammation is affecting the colon. Since the many forms of IBD can affect different people, the factors and symptoms can vary for each individual going from mild to severe if it is not treated.
The Pathophysiology Of IBD
The pathophysiology of IBD (inflammatory bowel disease) is where there is chronic inflammation around the gut, GI (gastrointestinal) tract, and both the large and small intestines. IBD also has two forms of inflammatory conditions known as Crohn’s disease and ulcerative colitis that can affect the intestines and the colon. The symptoms that these chronic inflammatory diseases also cause include abdominal pain, ulcers, diarrhea, and severe cramping, which can cause a person to be in constant pain. Since IBD, Crohn’s disease, and ulcerative colitis causes chronic inflammation of the digestive system, the factors that can cause these chronic diseases to progress can be due to genetics, compromised immune system, and environmental triggers.
The Symptoms Of IBD
Some of the symptoms that individuals with IBD (inflammatory bowel disease) can vary as they can come and go in the body. Research studies have found that individuals would experience mild or severe symptoms of IBD that can come gradually or suddenly at any time of day or night. Some of the symptoms that IBD causes include:
- Abdominal pain
- Bloating
- Loss of appetite
- Joint pain
- Fatigue
IBD can also cause other symptoms because it can cause flare-ups in the gut and is common in about 3 million individuals affecting all ages and genders. It is different from IBS (irritable bowel syndrome) since IBS affects bowel function while IBD damages the intestines and increases the risk of colon cancer in many individuals.
Crohn’s Disease Symptoms
Research studies show that Crohn’s disease can affect any part of the small or large intestines and can cause unwanted issues to a person as it can affect the body. The signs and symptoms that a person with Crohn’s disease can vary from being mild to severe as they develop gradually or suddenly without any warning. The symptoms that Crohn’s disease can cause to a person include:
- Abdominal pain
- Fever
- Weightloss
- Anemia
Other symptoms that Crohn’s disease can cause in the body are extraintestinal manifestations. They can vary from a recurrence of urinary tract infections, arthritis, ankylosing spondylitis to a person having gallstones in their system.
Ulcerative Colitis Symptoms
Since ulcerative colitis affects the colon and the rectum, the signs and symptoms of ulcerative colitis can range from being mild to severe, as research shows. Unlike IBD and Crohn’s disease, ulcerative colitis’s symptoms develop over time and, depending on how the inflammation has progressed in the colon, can vary. Some of the signs that are caused by ulcerative colitis include:
- Rectal pain
- The inability to go to the bathroom
- Nausea
- Liver disease
- Red, painful eyes
- Mouth sores
- Loss of fluids and nutrients
Conclusion
The gut system ensures that any food or liquid is being digested and excreted out of the body to ensure that everything is functioning correctly and that the nutrients are being transported throughout the entire body. Therefore, chronic inflammation in the gut system can cause IBD (inflammatory bowel disease) in the GI tract and cause many unwanted symptoms that can turn chronic over time if it is not treated right away. When chronic inflammatory diseases like IBD, Crohn’s disease, and ulcerative colitis affect the gut, many individuals will be in pain and try to find some relief to dampen the effects that it has caused in their gut system. The second part of this series will discuss how IBD affects the organs and how different treatments dampen the impact of IBD in the gut system.
References
Fakhoury, Marc, et al. “Inflammatory Bowel Disease: Clinical Aspects and Treatments.” Journal of Inflammation Research, Dove Medical Press, 23 June 2014, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4106026/.
Ha, Francis, and Hanan Khalil. “Crohn’s Disease: A Clinical Update.” Therapeutic Advances in Gastroenterology, SAGE Publications, Nov. 2015, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4622286/.
Lynch, Whitney D., and Ronald Hsu. “Ulcerative Colitis.” StatPearls [Internet]., U.S. National Library of Medicine, 18 June 2021, https://www.ncbi.nlm.nih.gov/books/NBK459282/.
Medical Professionals, Cleveland Clinic. “Inflammatory Bowel Disease: Symptoms, Treatment & Diagnosis.” Cleveland Clinic, 3 May 2021, https://my.clevelandclinic.org/health/diseases/15587-inflammatory-bowel-disease-overview.
Medical Professionals, Cleveland Clinic. “Ulcerative Colitis: Symptoms, Treatment, Living with It & Diagnosis.” Cleveland Clinic, 23 Apr. 2020, https://my.clevelandclinic.org/health/diseases/10351-ulcerative-colitis.
Ranasinghe, Indika R., and Ronald Hsu. “Crohn Disease.” StatPearls [Internet]., U.S. National Library of Medicine, 8 June 2021, https://www.ncbi.nlm.nih.gov/books/NBK436021/.
Staff, Mayo Clinic. “Crohn’s Disease.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 13 Oct. 2020, https://www.mayoclinic.org/diseases-conditions/crohns-disease/symptoms-causes/syc-20353304.
Staff, Mayo Clinic. “Inflammatory Bowel Disease (IBD).” Mayo Clinic, Mayo Foundation for Medical Education and Research, 7 Nov. 2020, https://www.mayoclinic.org/diseases-conditions/inflammatory-bowel-disease/symptoms-causes/syc-20353315.
Staff, Mayo Clinic. “Ulcerative Colitis.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 23 Feb. 2021, https://www.mayoclinic.org/diseases-conditions/ulcerative-colitis/symptoms-causes/syc-20353326.
Disclaimer
Professional Scope of Practice *
The information herein on "The Pathophysiology Of Inflammatory Bowel Disease | Part 1" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card