Can cervical retraction be a good addition to a home exercise program for individuals with neck pain, spinal arthritis, or needing to strengthen their neck muscles?
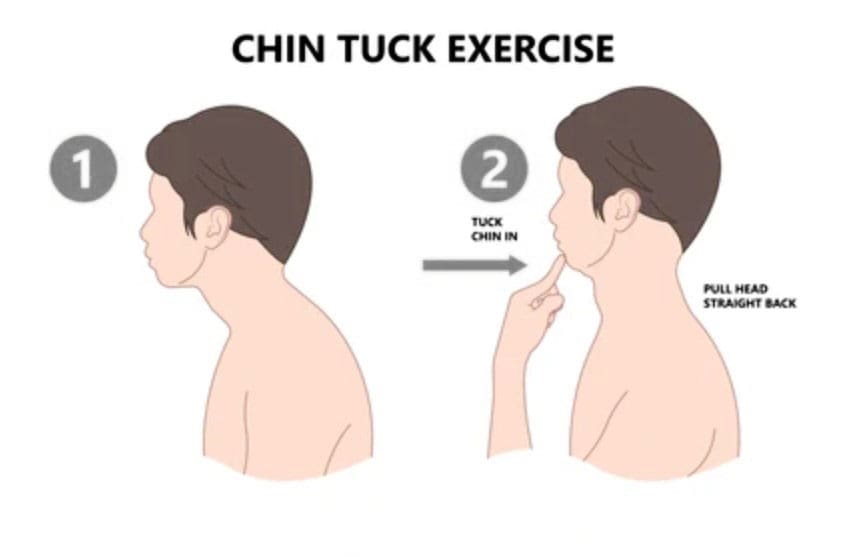
Table of Contents
Cervical Retraction
Cervical retraction is a neck exercise that involves gently sliding the head backward while keeping the chin tucked. It can help with:
- Neck pain
- Stretching and loosening the muscles at the back of the neck.
- Headaches
- Tightness
- Improve posture
- Improve flexibility and mobility
Preparation
Basic steps for performing a cervical retraction exercise:
- Sit upright with good posture.
- Tuck your chin as far as you can comfortably.
- Look up while keeping your chin tucked.
- Rotate the neck 1-2 inches to each side.
- Return to the starting position.
- Stop the exercise if you experience pain.
You want to get good at this without loading the joints while learning the movement. Gently and accurately moving your head in alignment with the neck will help you find the correct head action as it moves. Then, it can be performed as a full exercise. Performing the movement correctly requires focus. This is why cervical retraction is done while sitting in a chair with proper posture. Individuals can also stand, but it is more complicated for the body to coordinate than sitting, but it can be done once the individual has practiced.
Sitting or Standing
- Gently tuck your chin down toward your neck.
- The focus is alignment.
- Keeping your chin where it is, press your head back.
- Feel the stretch at the back of your neck.
- Relax and repeat.
- Try doing 8-10 reps, with 3-4 daily sessions. (North American Spine Society, 2012)
Pain Management
- There will be soreness, especially for those with pain symptoms, but the neck should feel better.
- Be mindful of any intense or severe pain resulting from cervical retraction.
- Individuals with cervical spondylosis (neck arthritis) stop if pain presents. (Cleveland Clinic, 2023)
Other Neck Exercises
Another good neck-strengthening exercise is the isometric neck press. In this exercise, you move your head forward, backward, and to each side while your hand provides resistance. This develops flexibility and is recommended for those with arthritis in this area. (Sadeghi, A. et al., 2022) Other exercises include: (Pain Consultants of West Florida, 2019)
- Neck extensions: Backward bending can help relieve nerve compression and ease the strain on the cervical spine.
- Side rotation: This exercise can improve neck mobility.
- Shoulder rolls: This exercise can help keep the neck and shoulder joints fluid.
Injury Medical Chiropractic and Functional Medicine Clinic
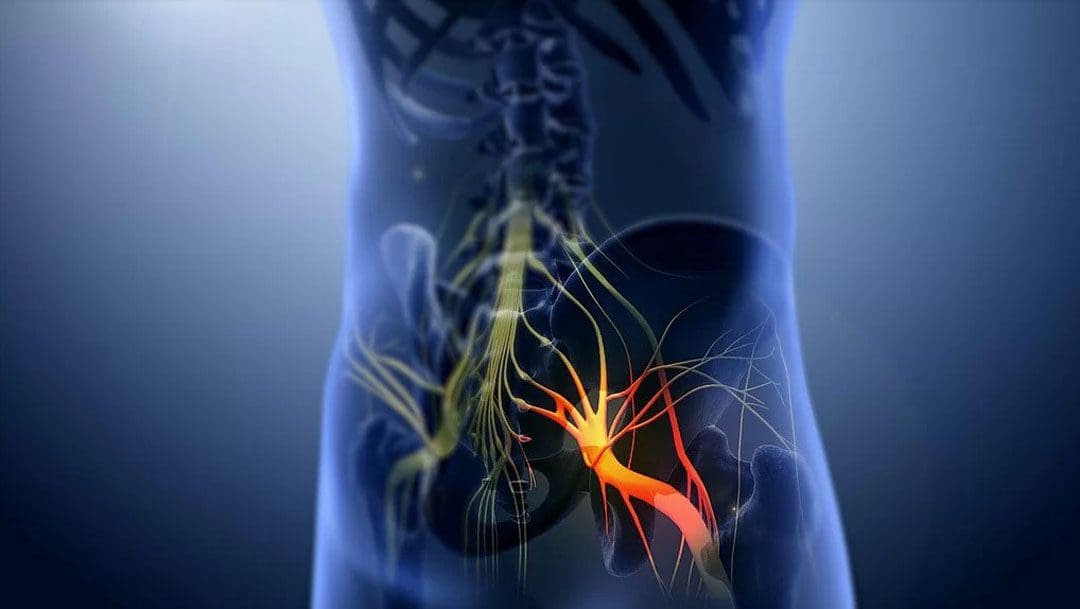
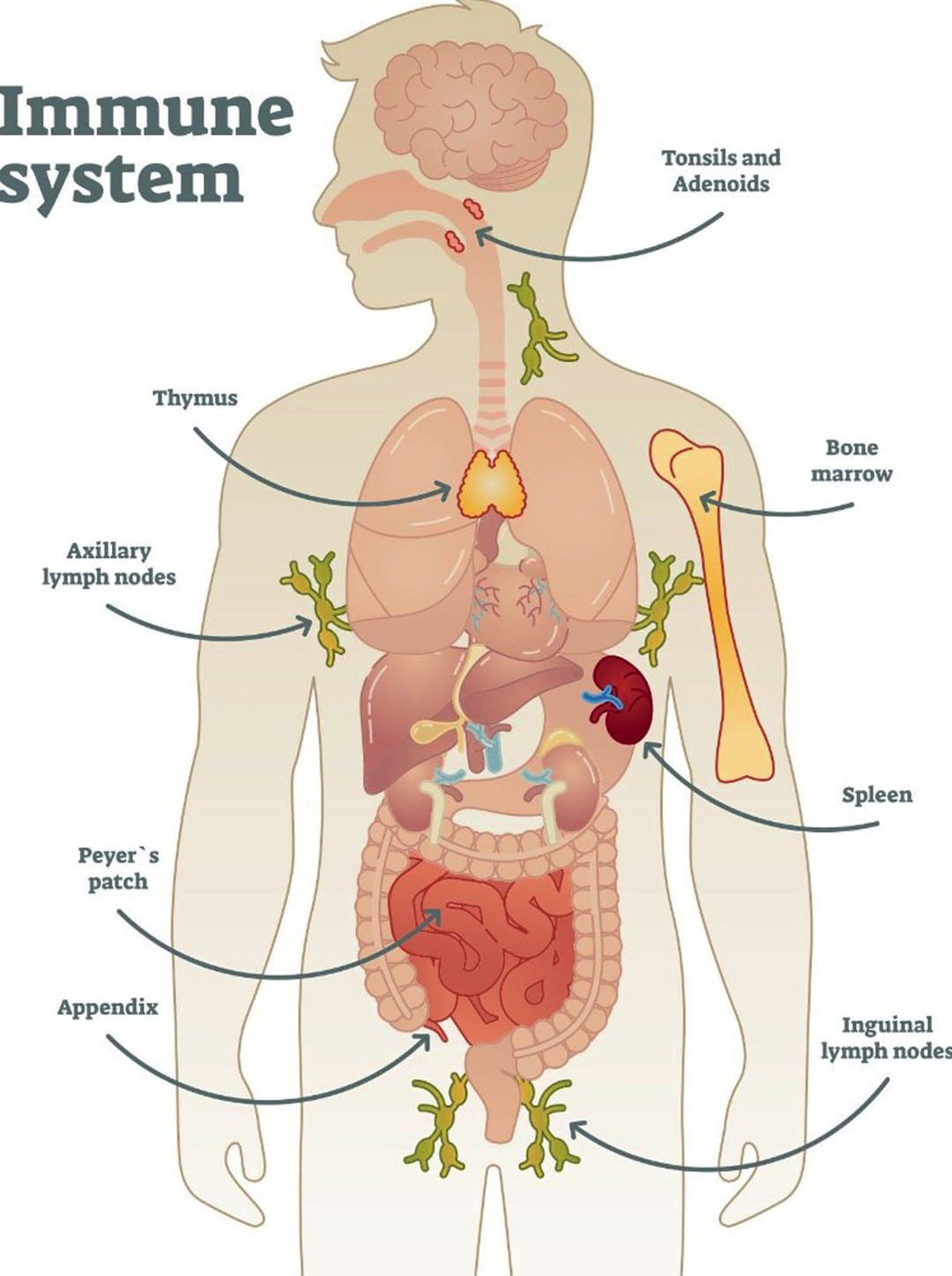
If you have a neck condition or radiculopathy that causes pain or other symptoms going down the arm or are unsure how to do it, check with a healthcare provider or physical therapist before trying the exercise. Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to develop an optimal health and wellness solution. We focus on what works for you to relieve pain, restore function, and prevent injury. Regarding musculoskeletal pain, specialists like chiropractors, acupuncturists, and massage therapists can help mitigate the pain through spinal adjustments that help the body realign itself. They can also work with other medical professionals to integrate a treatment plan to resolve musculoskeletal issues.
Neck Injuries
References
North American Spine Society. (2012). Cervical exercise: The Backbone of Spine Treatment. https://www.spine.org/KnowYourBack/Prevention/Exercise/Cervical-Exercise
Cleveland Clinic. (2023). Could your neck pain actually be neck arthritis? https://my.clevelandclinic.org/health/diseases/17685-cervical-spondylosis
Pain Consultants of West Florida. (2019). Chronic Neck Pain: How Core Exercises Can Help. Our Blog. https://pcwfl.com/chronic-neck-pain-how-core-exercises-can-help/
Sadeghi, A., Rostami, M., Ameri, S., Karimi Moghaddam, A., Karimi Moghaddam, Z., & Zeraatchi, A. (2022). Effectiveness of isometric exercises on disability and pain of cervical spondylosis: a randomized controlled trial. BMC sports science, medicine & rehabilitation, 14(1), 108. https://doi.org/10.1186/s13102-022-00500-7