Triathlon training involves running, biking, and swimming. This much fitness training takes a toll on the body. Pulled hamstrings, twisted ankles, and sore heels are common, but triathlon training can also cause or worsen back pain. Because the back muscles are connected to many other muscles, certain types of movement after a tough training session can present with back pain. There was an Ironman triathlete study that found that 90% of the athletes suffered some form of soft-tissue injury during training, with 70% reporting low back pain and/or sciatica. A 2020 study in BMC Musculoskeletal Disorders found that 14% of recreational half-marathon runners presented with low-back pain.

Table of Contents
Triathlon Training Hard on the Back
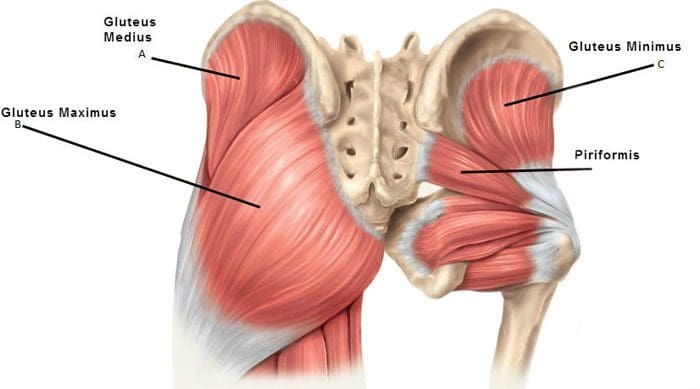
High-impact activities/exercises, constant repetitive motion, places a heavy pounding on the body that impacts the joints and spine. Using improper techniques will aggravate any issues. The stresses applied from repetitive motions, and poor form can lead to the joints breaking down. If new to intense training the muscles might not be strong enough yet, which could also cause back pain and injury. The back stabilizer muscles tend to get neglected in the training, but these muscles support the structures in the midline, spine, and joints. Strengthening the:
- Base muscles
- Glutes
- Back muscles
- Core
- Ensures stability of the spine and joints from all the wear and tear.
Training and Overtraining Errors
Even veteran athletes can make mistakes during their training that can lead to sore backs. The biggest mistake individuals make during triathlon training is that they only swim, bike, and run. Training for the specific sport/s is important; but weight lifting, core strengthening, and flexibility training are just as important. Proper rest can become neglected as the individual wants to get in as much training as possible that often gets overlooked, leading to overuse injuries. However, rest is a vital part of training to allow the body to fully recover and operate at full and optimal potential.
Preventing and Avoiding Back Pain When Training
How to sidestep back pain altogether during training includes:
Sleep
A healthy lifestyle includes proper sleep cycles and is even more important during training. The mental aspects a triathlon competition can create require proper rest. Fatigue can also lead to poor technique/form, placing excess stress on the joints and the spine, leading to injury.
Flexibility
Muscles need to maintain flexibility to preserve function and recovery ability. After a training session stretching and working on flexibility will help with overall performance. Stretching should be done after activity when the muscles are warm, and the fibers can be stretched/elongated for optimal recovery.
Proper nutrition
The body needs high-performance fuel to support high-calorie deficits that are associated with intense training and competition.
Strengthening the body
Having a solid body foundation is the objective. Everything is balanced with strong muscles supporting healthy bones. Specific exercises that target the multifidus muscles. These are the body’s back brace. Strengthening these muscles will help prevent spinal injury/s. Back-strengthening exercises include:
- Cat-cow stretch
- Glute bridges
- Bird dog
- Planks
- Mobility stretches
Rest days no matter what
Plan rest days no matter what. Pushing through will not make the body stronger or able to perform better, and could cause performance to decrease leading to injury. This does not mean sleeping all day, but engaging in active recovery where the body gets the rest it needs while still maintaining fitness. Active recovery includes:
- Moving
- Stretching
- Foam rolling
- Sports chiropractic massage
- Body rejuvenation
- Body and mind exercises
- Allows for a thorough recovery and enhances training.
Technique Improvement
Proper form and technique can really make the difference between staying injury-free and injury/s. Using the right form promotes healthy function. It could help to have gait, swim stroke, and bike techniques evaluated by a professional to ensure that proper form is being utilized.
Body awareness
Stop if the body signals one to stop. This is why the body feels pain. It is the internal mechanism that tells the individual something is wrong. It is not recommended to follow the phrases train through the pain, and no pain, no gain. Individuals are recommended to:
- Always pay attention if pain presents and does not go away after exercising or warming up.
- Pain that limits function.
- Pain that interferes with daily activities.
- These could significantly exacerbate a spinal injury and should be checked by a doctor.
Body Composition
Rest and Recovery
During rest and recovery, the body goes back to normal or homeostasis. This is the body’s resting rate or normal phase. The body is always trying to go back to homeostasis. This is done by:
- Maintaining core temperature
- Blood pressure stable
- Muscles refreshed
When exercising/training, the homeostasis phase is disturbed, meaning the body needs a period of rest to return to normal. The process of homeostasis uses a lot of energy, which results in an abundant amount of calories burned. After exercise, there is an increase in excess post-exercise oxygen consumption or EPOC. The body uses up more oxygen during recovery than it does before or during exercise. This increase results in burned calories and strong muscles. The most important part of recovery is the rebuilding of muscle. When working out, especially resistance training, tiny tears are made in the muscle fibers. For the tiny tears to turn into growing muscles, they need to repair themselves. This happens during rest. Apart from the physiological benefits, rest helps prevent injury caused by overuse and assists in healing when injuries do occur. Time off helps with mental health as well to refocus, reassess, and apply what has been learned. What rest and recovery can do for the body includes:
- Burn massive calories
- Build muscle
- Refuels the muscles
- Prevents injury
- Improves mental health and motivation
References
American journal of physical medicine & rehabilitation/Association of Academic Physiatrists. (October 2014) “Efficacy of Aerobic Exercise for Treatment of Chronic Low Back Pain: A Meta-Analysis” https://www.researchgate.net/publication/266682158_Efficacy_of_Aerobic_Exercise_for_Treatment_of_Chronic_Low_Back_Pain_A_Meta-Analysis
Scientific Reports. (April 2017) “Running exercise strengthens the intervertebral disc” https://www.researchgate.net/publication/316262547_Running_exercise_strengthens_the_intervertebral_disc
Stretch Before and After Journal of Chiropractic Medicine. (Winter 2003) “Changes in low back pain in a long-distance runner after stretching the iliotibial band” https://www.sciencedirect.com/science/article/pii/S0899346707600718