Introduction
In today’s podcast, Dr. Alex Jimenez and Dr. Mario Ruja discuss what sciatica does to the body and how it affects a person’s overall health and wellness.
What Causes Sciatica?
[00:00:06] Dr. Alex Jimenez DC*: Hey Mario, we’re on a new podcast today. Today we’re going to be talking about sciatica and the complications with that. I got Mario here, and we’ve decided to chat and discuss the issues of sciatica.
[00:00:29] Dr. Mario Ruja DC*: It sounds excruciating.
[00:00:31] Dr. Alex Jimenez DC*: You know, let me ask you this. In your practice, Mario, in terms of working with sciatica, what have you learned over the years in terms of sciatica?
[00:00:41] Dr. Mario Ruja DC*: Sciatica will put you down, Alex. It will make you feel like a baby and make you remember how vital chiropractic is and maintenance. It’s like having that car. For example, if you are driving Buggati and do not do the maintenance, you just put gas. It’s just like, rip it and run it. And then one day, it leaves you hanging in the middle of I-10, and everyone’s passing you, and you’re embarrassed.
[00:01:15] Dr. Alex Jimenez DC*: It is what sciatica is.
[00:01:18] Dr. Mario Ruja DC*: It isn’t very pleasant.
[00:01:20] Dr. Alex Jimenez DC*: You know, I believe it’s kind of funny that we’re laughing at it, but it is a scourge. I call it of the low back. It catches you off a surprise. It creeps up on you. It looms around, too. Yeah. And when they bite you, I mean it classically defined as pain going down the leg. There’s a lot of reasons why that happens. What do you get when your patients show up with that? What do they tell you? What kind of symptoms do they sort of present?
[00:01:45] Dr. Mario Ruja DC*: You got to be kidding me. First of all, their wife drives them in. Does that tell you what it is? Yeah, it’s like a knife stabbing them in the back, and it radiates down their leg, and then they’re usually leaning to one side or another. And then they have this story. Alex, there is this crazy story like, ” Well, I was only…” the only part is ridiculous. “I was only picking up my child,” or “I was only throwing the football, and all of a sudden, my back went out. And then I try to stretch it, and I have my wife rub it. And all of that didn’t work the following day. I couldn’t get out of bed and had to crawl to the bathroom.” Now that is when your attention is on.
[00:02:43] Dr. Alex Jimenez DC*: Yeah.
Dr. Alex Jimenez and Dr. Mario Ruja Explain What Sciatica Does To The Body.
[00:02:44] Dr. Mario Ruja DC*: Our attention is on sciatica. This is a big topic, Alex.
[00:02:48] Dr. Alex Jimenez DC*: This is a vast topic, and let me just kind of throw this out there where we are going to begin the process of breaking down sciatica by no means are we going to be able even to know the breadth and width as this is like saying you can take down a sequoia with one bite. It’s not going to happen, and we’re going to have to chisel away from it. And as we go in there, we’re going to go deep. Are we going to get nasty with the science, Mario?
[00:03:14] Dr. Mario Ruja DC*: This is getting deep and nasty. Folks will have to strap on their seatbelts for this ride.
[00:03:21] Dr. Alex Jimenez DC*: Absolutely. As we do that, we’re going to be able to kind of go deep into it. We’re going to touch on some subject matters, but follow us on this process because we’re going to be discussing real essential issues about sciatica that affects so many millions of people at any given point. I’d venture to say that one in every four people is suffering from chronic back pain, and half of those people are suffering from sciatica in some form or the other or some pain down the leg. So in that sense, we’re dealing with a huge issue that affects millions of patients and millions of people across the country with all different doctors and different types of protocols. And these protocols can be from really esoteric to invasive. And we all want to do it quickly, and we all want to do it a simple way. So I think modern medicine Mario has determined that we have to go basic and try everything before any surgical interventions.
[00:04:16] Dr. Mario Ruja DC*: I mean, it’s common sense, and I always used the car model as an example. Before you get a rebuilt transmission, why don’t you maintain it before you drop a new engine? Why don’t you change the oil and get a tune-up? Unfortunately, again, you mentioned the unbelievable impact of low back pain in our society. I believe I don’t know if I may be in the ballpark. It is the number two or three reasons for work injuries and is one of the biggest reasons for the military to get med boarded out of the military. I mean, this is a big issue that impacts people’s lives, and then you would get into chronic pain management, things like that. But again, if we look at the most critical solution in our life, how can we prevent it? Prevention is the natural utilization of therapeutic arts that decrease the misalignment in the spine. Again, that misalignment is that torque where your back is out of alignment and calibration, right? Which causes uneven wear and tear on the disc. Then the other one is constant compression of sitting down and repetitive motion. The other one is just the injuries from everyday sports activities. More and more young kids are getting injured in sports football, basketball, more intense pain, more torque, and you can see pro basketball players and football players, all of them suffer from sciatica.
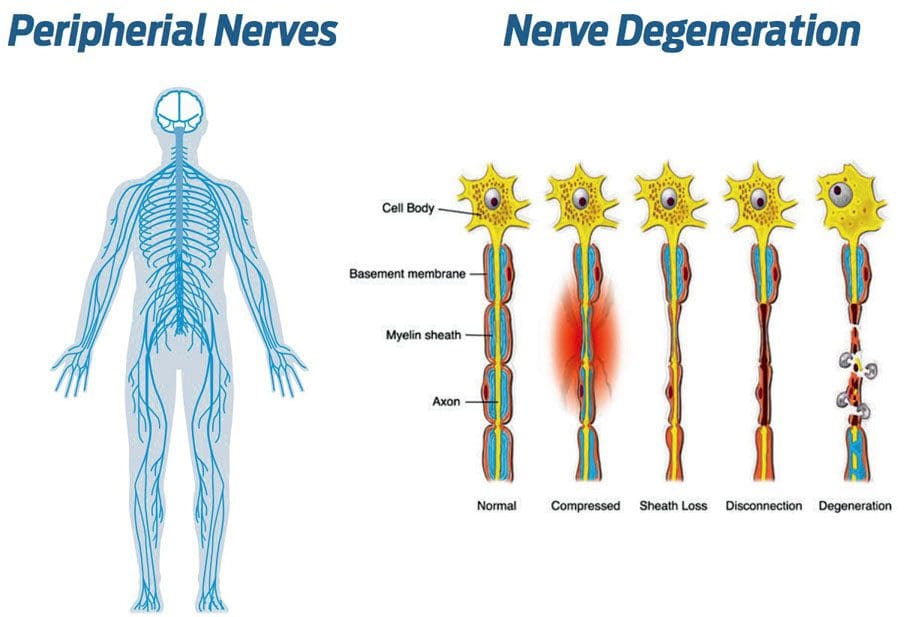
[00:06:19] Dr. Alex Jimenez DC*: Yeah. Here’s the cascade. The cascade starts with a decalibration of the pelvis or the hips, or some injury trauma, some space-occupying lesion, or something on this path. I’m going to go ahead and demonstrate here on our pathway, and we’re going to show a little bit of what is in the nerves.
[00:06:43] Dr. Mario Ruja DC*: I love this 3-D model you are showing here.
[00:06:43] Dr. Alex Jimenez DC*: Thank you.
[00:06:44] Dr. Mario Ruja DC*: This is good stuff.
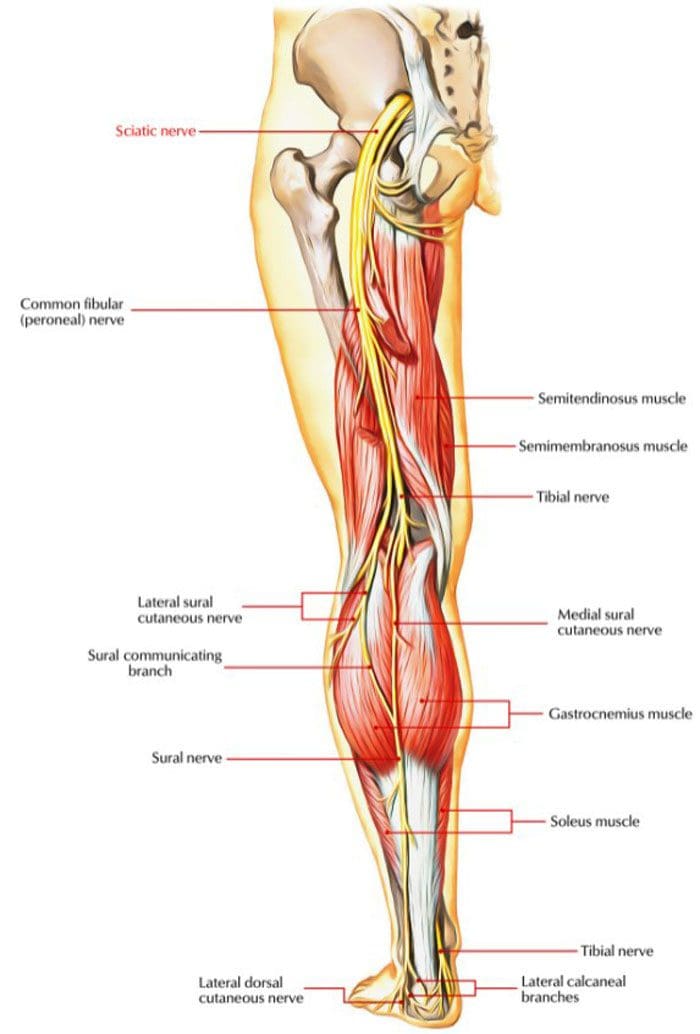
The Sciatic Nerve
[00:06:46] Dr. Alex Jimenez DC*: This is the complete anatomy provided for us and what we can see is a three-dimensional aspect of how and why someone has sciatica. Now when you look at this, Mario, what’s your first take? Because for me, it says it’s a complicated structure when we’re looking at this. When you look at the back, where it comes out, you see this big old cable called the sciatic nerve, but you see so many proximal areas and so many regions that are getting weird.
[00:07:11] Dr. Mario Ruja DC*: That is a lot of moving parts, Alex.
[00:07:15] Dr. Alex Jimenez DC*: Yes, it is. And you know what? One of the crazy things that I’m looking at here is the sacrum.
[00:07:20] Dr. Mario Ruja DC*: And that is the base.
[00:07:21] Dr. Alex Jimenez DC*: That’s the foundation. The way the creator created us was that this is where energy transmits this bone right here. The sacrum, right? But little to the front of it. You have the sacral nerve roots that come out as they form out. You can see on this particular area; you can see the nerve roots coming out as they come in posterior aspect, you can kind of turn this around and we kind of get this little area here and as we rotate this thing, we can see the sciatic nerve as it comes out of what we call the sacral notch. That sacral notches right there is enormous.
[00:08:03] Dr. Mario Ruja DC*: That is crazy.
[00:08:04] Dr. Alex Jimenez DC*: I know, right? So what happens is when you see it here, you can understand that this big ol’ nerve influences the entire creature. You take this thing out, and you have limited the creature’s ability to move. Please look at it as it comes out; you can look from the inferior border to the superior border. You can see why a woman is pregnant; you can determine why this baby could sit in this pelvic cavity here can cause a lot of damage to the sacral nerve.
[00:08:31] Dr. Mario Ruja DC*: Many of them suffer from back pain and sciatica.
[00:08:34] Dr. Alex Jimenez DC*: This is one of the reasons why right here that baby sits and dances in this whole area here. So when we look at this kind of stuff, we can make sense of all the presentations. As you hurt a nerve in one area, you can see that you would hurt as you would do something like this. And the nerve will hurt a distal or pull towards away from it. Once you hurt that region, our goal is to determine the nerve roots going down on that particular area. If this affects all the way down the leg, it will cause pain. Now, you can see in this specific region what goes on.
[00:09:18] Dr. Mario Ruja DC*: This is it now. Now you see that this is what I like, and this is a creation. If you believe in miracles, you stop believing and just realize that you’re one walking. Here’s the sacral sacrum right here, the sacred bone, and that’s why it’s called sacrum because it’s sacred.
[00:09:42] Dr. Alex Jimenez DC*: I didn’t know that. I learned about the scared bone, and it is the base of the spine.
[00:09:48] Dr. Mario Ruja DC*: This is where, as you mentioned, this is where the birth comes out. This is where the next legacy is created. So here is the ilium. OK, so that’s your hip bone. You have two of them. There is symmetry in our bodies, and that’s how God created us in symmetrical synergy. Then right here are pubic surfaces, and then you’ve got the operators right there, and then here is that L5 disc, and this is the one where I would say probably about 80 percent of disc herniations happened right there. So if you want to take a wild guess, this is it right here.
Intervertebral Foramen
[00:10:32] Dr. Alex Jimenez DC*: Let me hone in on that right there so I can bring that in a little bit better.
[00:10:42] Dr. Mario Ruja DC*: This thing is dancing.
[00:10:43] Dr. Alex Jimenez DC*: As Dr. Ruja was explaining, he’s talking about in the disk space of the spine right here.
[00:10:51] Dr. Mario Ruja: Right, so see, that is where you have the IVF.
[00:11:00] Dr. Alex Jimenez DC*: Intervertebral foramen.
[00:11:01] Dr. Mario Ruja DC*: IVF. Interverebral foramen. There it is, and all that is like a fancy word for it. There’s a hole where the right everything comes out.
[00:11:06] Dr. Alex Jimenez DC*: So here we start looking at the hole on the side, and as we look at it right there. You can see where the nerve roots come out right there.
[00:11:29] Dr. Mario Ruja DC*: So at that point, you see it here.
[00:11:35] Dr. Alex Jimenez DC*: Exactly, and as you turn the model.
[00:11:38] Dr. Mario Ruja DC*: OK, right there.
[00:11:41] Dr. Alex Jimenez DC*: That is the nerve right there.
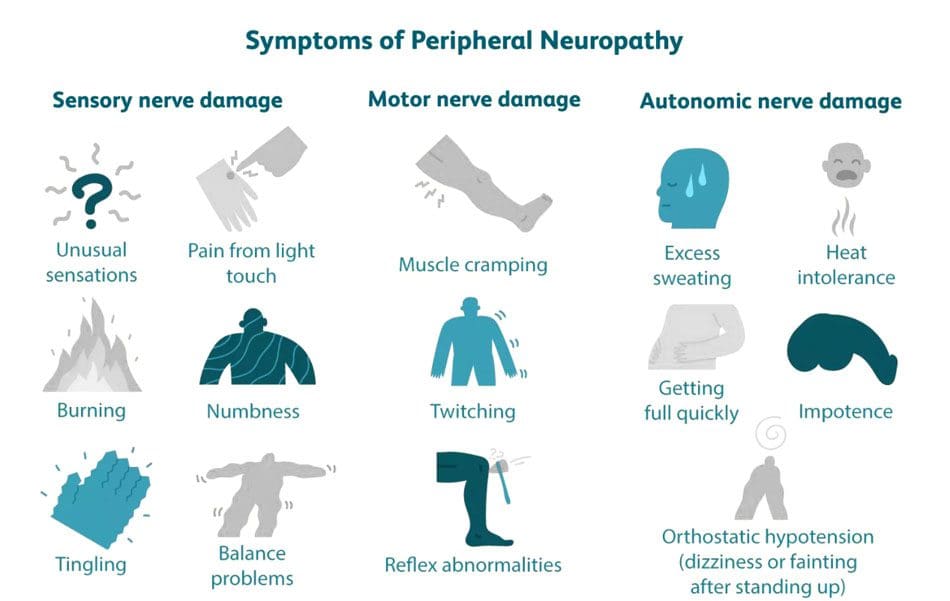
[00:11:43] Dr. Mario Ruja DC*: So this is where how they sit on top of each other right there. Then you can see it from underneath right in there. Now at this point, these nerves, like the fiber optics, are traveling down through these canals and openings and everything. So there are so many places, Alex, that they can be entrapped, compressed, and they can be twisted again. Remember, the big word for us and in our talks is inflammation.
Does Inflammation Causes Problems In The Body?
[00:12:23] Dr. Alex Jimenez DC*: Inflammation yes.
[00:12:26] Dr. Mario Ruja DC*: Deep inflammation, yes. Now, these are all again if you’re looking like an electrician because I love how electricians work. You look at the fiber optics, and you have to trace it and find out where the issue is? Is it up here? Right here? Is it in the middle? Is it here in the canal? It is right there in that notch is the muscle compress.
[00:13:01] Dr. Alex Jimenez DC*: Oh yeah, you can see it in the muscle compress.
[00:13:12] Dr. Mario Ruja DC*: See where it’s pinched right there. That peraforma muscle is now critical. Again, that’s where you see a lot of times you need to release that muscle. Once it compresses, it just goes haywire right there.
[00:13:30] Dr. Alex Jimenez DC*: Yeah, why do they call the peraforma muscle Mario?
[00:13:35] Dr. Mario Ruja DC*: Tell me, Alex.
[00:13:37] Dr. Alex Jimenez DC*: Because it looks like a pear. When you take it, it’s a fat muscle when you look kind of flat here.
[00:13:43] Dr. Mario Ruja DC*: And I visualize in the pear, Alex.
[00:13:44] Dr. Alex Jimenez DC*: Yeah. Here is the top of the pear, and that’s the wide part of the pear.
[00:13:49] Dr. Mario Ruja DC*: That’s cute, Alex. I don’t know what kind of pear that is.
[00:13:52] Dr. Alex Jimenez DC*: Exactly.
[00:13:52] Dr. Mario Ruja DC*: But yeah, you’re right, it’s pear-shaped. Now I can see it.
[00:13:56] Dr. Alex Jimenez DC*: This is a crazy part. There’s a superior Escamilla right here in that area so that it can be trapped anywhere. As we look at this from the base point of view, you can see why people start having these symptoms.
[00:14:08] Dr. Mario Ruja DC*: Yeah, if we look at this pattern, we can also see an increased sedentary lifestyle, Alex. Can you see how all of these muscles are here? The glutes, gluteus minimus, Maximus, the hamstrings. Major squat muscles and the hips. Can you see all of these being deconditioned and compressing on a nerve?
The Lymphatic System
[00:14:40] Dr. Alex Jimenez DC*: Yeah, let me show you this, Mario because I wanted to show you this. When I first started seeing this, I thought this as you begin noticing that you have the venous system, but here’s what people don’t know about the venous system. Next to it is the lymphatic system. Now let me remove these muscles here, and you’re going to see the intricacies of the green lines. These green lines are in the circulatory system.
[00:15:02] Dr. Mario Ruja DC*: Wow, the green lines are the lymphatic system.
[00:15:05] Dr. Alex Jimenez DC*: The green is the lymphatic, and the red is arterial. When you start seeing red now, you can see that they have problems with their circulation when someone sits down a lot. And as you can see here, imagine sitting down all day on top of this thing? Can you see how the inflammation would happen in that region?
[00:15:25] Dr. Mario Ruja DC*: Alex, look at how much is happening in that pelvic area. I mean, this is like fiber optics just strapped, and this is like compress. Already, there is not that much space going on here, Alex. I mean, you’ve got nerves, arteries, veins, and lymph, all of those going through the same canal. So there is not a lot of what I call, you know, space and forgiveness. That’s why this radiating pain down the leg compresses that area that the flow down the leg is activated. That’s why your leg goes numb and your muscles to a large extent after a long time of having this problem. What happens, Alex, with a lot of my patients is they get muscle atrophy. You know, they gain muscle weakness, and that’s where your muscles shrink.
[00:16:40] Dr. Alex Jimenez DC*: Let me show you the additional muscles here. You see, that’s why we train because all these muscles here are surrounding and covering up this area, and the muscle decalibrates.
[00:17:00] Dr. Mario Ruja DC*: Decalibrates.Is that like a fancy word for saying it just…
[00:17:05] Dr. Alex Jimenez DC*: De-conditions?
[00:17:06] Dr. Mario Ruja DC*: That flops down?
[00:17:08] Dr. Alex Jimenez DC*: For me, I like the word calibration because it is a fine-tuned structure. Philosophically speaking, they got a bump at this ball that follows them everywhere when you look at humans. This power unit, right? This throttling system, it’s the glutes. Some have it more significant than others, right? But here’s where we propel from; it is the source of power. It is the way the creature creates its anchor. If the hips are gone, the beast doesn’t survive. So when we look at this, and we look at someone who was an athletic person when they were young and all of a sudden they get this job where they sit in front of a computer, they don’t go out. What happens to them? They decalibrated like a car. It doesn’t get used, and before you know it, it starts sinking and becoming flattered, and eventually, the inner workings that we just came from really start grinding. So when there’s congestion, the lymphatic system is responsible for the circulation. But the lymphatic system, unlike the arterial and venous system, which works primarily with the heart pumping, is functional by motion. So when you sit down, you are not moving.
[00:18:16] Dr. Mario Ruja DC*: You know what, Alex? It is the sacral occipital pump; when you’re talking about the CSF cerebral spinal fluid, I can tell you right now when that sacrum is not pumping back and forth when you’re walking, you know what happens? It’s stagnating to flow to your brain.
[00:18:36] Dr. Alex Jimenez DC*: It does.
[00:18:37] Dr. Mario Ruja DC*: Yeah, all the way to your brain. Then the area that you talked about that I think is critical. You’ve got to keep the body moving. We are created as bipeds. We do not walk like gorillas who walk on all fours. I know sometimes you feel like one, but we’re not apes. That’s right; we’re not silverback apes. The thing is, we’re bipeds. So that means the whole body has to align and stand up. Alex, in every sport, I tell people I’m impressed with your biceps, but your core sucks. You know what? Your core determines your overall function. That is where you keep your body upright, and you create that calibration of your spine. Once that that lordosis, that curve into your back. Once that is lost, you’re degenerating; you’re aging. There it is, right there.
[00:19:41] Dr. Alex Jimenez DC*: Let’s go ahead and take a look at that right there. Yeah, that’s the lordosis you’re talking about in the spine.
The Lordosis
[00:19:56] Dr. Mario Ruja DC*: Can you draw the lordosis out?
[00:19:59] Dr. Alex Jimenez DC*: Of course.
[00:20:01] Dr. Mario Ruja DC*: Wow, that is crazy, Alex.
[00:20:06] Dr. Alex Jimenez DC*: That is crazy.
[00:20:10] Dr. Mario Ruja DC*: OK, so let’s do the pink pen for pain on the lordosis.
[00:20:17] Dr. Alex Jimenez DC*: That curve along with this curve makes a big difference. So what happens is you end up understanding that this sacrum or this glute area influences a vast area. What I’ve learned in my practice is that when you have a person with a sciatic issue, there are upper back issues, and there are shoulder issues now if the lower back has problems…
[00:20:53] Dr. Mario Ruja DC*: It throws everything off, and it’s like a domino effect.
[00:20:56] Dr. Alex Jimenez DC*: Yeah. What do you think about when they tell you, Hey, the person only hurt their lower back, and this is a work-related job? And similarly, they say it’s only related to the back. Yet they come in with leg pain, arm pain, and it makes sense to us, but nobody wants to understand that.
[00:21:11] Dr. Mario Ruja DC*: Yeah, that’s because they don’t want to, Alex. That’s where they want to lie, and it’s a lie. Remember when your mama told you it is not OK to lie?
[00:21:34] Dr. Alex Jimenez DC*: You know what? Why don’t we just say for what it is? They’re lying. They understood why they don’t understand that the body is a biomechanical chain, and if it affects the hips, it starts affecting the lower back, which then affects the upper back. And everybody knows if you have a back that’s giving up, your shoulders will have issues. If you got shoulder problems, it is equally on the opposite side of the room; you’re going to have knee issues. So what happens is as we look at this dynamic model, we see that we can’t be telling a fib here.
The Trapezius
[00:22:06] Dr. Mario Ruja DC*: The spine is one unit composed of many segments. OK, it’s not separate. So there is no way that you can have an injury to one part of the spine, and you can tell me 100 percent that it does not affect any other one. It’s impossible. I’m sorry, God didn’t create it. If you want to see it here, look at this ischium muscle as it goes all the way across. Look at this one. This one is amazing. I’m just going to do this. Here is here’s the muscle right here, trapezius. Now watch as it goes from here to where the shoulders are down, then go to the neck in the back of the neck.
[00:23:32] Dr. Alex Jimenez DC*: Let me clear up the pen marks, OK?
[00:23:35] Dr. Mario Ruja DC*: Can you move the body down?
[00:23:38] Dr. Alex Jimenez DC*: Yes, I can, and there you go.
[00:23:44] Dr. Mario Ruja DC*: So I want to show one example so you can see all the way to the base of the head.
[00:23:49] Dr. Alex Jimenez DC*: OK, I got you.
[00:23:52] Dr. Mario Ruja DC*: Alright.
[00:23:57] Dr. Alex Jimenez DC*: Well, here’s what you want to show. I think what you’re trying to show is that you’re trying to show the negative muscles and see all the good stuff in there.
[00:24:06] Dr. Mario Ruja DC*: Yeah, but I want to show you just that top layer, the trapezius.
[00:24:10] Dr. Alex Jimenez DC*: Oh, let’s go to the muscular portion.
[00:24:11] Dr. Mario Ruja DC*: So it goes all the way from the base. Can you zoom out so we can see the whole thing?
[00:24:16] Dr. Alex Jimenez DC*: Sure can.
[00:24:18] Dr. Mario Ruja DC*: OK, lift the model.
[00:24:20] Dr. Alex Jimenez DC*: I wish I could.
[00:24:23] Dr. Mario Ruja DC*: Now here it is, and this is how dynamic this is. When people say, Oh, you only hurt your neck, but not your mid-back. Here it is. Trapezius right here goes from the base of the skull down the shoulders, right there, all the way down to the mid-back. OK, and this is probably like T10 T11, right? Somewhere around there, right by the middle and all the way across. So this whole area right there, that’s one muscle, and if you have an injury here in this area, this will affect all the way here then if you go in deeper into the second and third layer of the muscle.
[00:25:50] Dr. Alex Jimenez DC*: Let me click here for you to see it.
[00:25:53] Dr. Mario Ruja DC*: Now it gets crazy.
[00:25:55] Dr. Alex Jimenez DC*: When we start removing muscular layers or increasing muscle layers, you start looking at all the functions.
[00:26:02] Dr. Mario Ruja DC*: Oh, look at that, the super spinadeus, And look at this right here. Vader scapula and from the shoulder all the way to the head is scalenus calculus.
[00:26:24] Dr. Alex Jimenez DC*: OK, so what we’re looking at here, we’re looking at the unbelievable body, but let’s go back to the area of concern.
[00:26:33] Dr. Mario Ruja DC*: All right, you see how connected it is, Alex.
What Are The Causes of Sciatica?
[00:26:36] Dr. Alex Jimenez DC*: Here’s the deal, OK? You and I know that the whole darn thing is connected, right? We can determine what is going on after dealing with the many patients we’ve seen over the years. And we’re like violin instructors. We touch the violin, and we make this body move. Our job is to understand when someone comes in and physically to see where this problem is. Find out where the issues are; there are tons of issues, and we haven’t even begun. We’re just having a general conversation about sciatica and where the issues are. What we don’t want is we don’t wish to surgical intervention at any early state unless it’s really necessary. Now what we’re looking at is when we see this, nobody wants that. So how do we fix this? So there are tons of ways to do that.
[00:27:26] Dr. Mario Ruja DC*: Can we go back to the slides of the causation for sciatica?
[00:27:34] Dr. Alex Jimenez DC*: Absolutely. I’m going to take you back to the causation when you get over there in a second. The causation is right here, and we are looking at it.
[00:27:51] Dr. Mario Ruja DC*: The first one is compression.
[00:27:52] Dr. Alex Jimenez DC*: Compression of the disc.
[00:27:54] Dr. Mario Ruja DC*: Compression due to the lack of calibration balance within the system. So you have uneven compression and then a lot of sitting down; we talked about that, right? And then inflammation again, inflammatory process. We spoke last week about metabolic syndrome, inflammation. Inflammation affects the whole body and the disc bulging. Number two right there is disc bulging. That one again is due to what? The spine is out of calibration, out of alignment, putting uneven pressure, and it’s just like squeezing a balloon or a donut. That’s a classic example. You put pressure on a donut on one side, and it will crack, then you go from this bulge to worse herniation. Herniation and then fractures. Of course, if you have trauma DDD, that’s a funny thing. Degenerative disc disease.
Degenerative Disc Disease
[00:28:58] Dr. Alex Jimenez DC*: Yes, early degenerative issues.
[00:29:00] Dr. Mario Ruja DC*: Right? And I love it because most people come into my clinic go, “Oh, I have degenerative disc diseases like I’m getting old,” and I say, “No. You had no maintenance on your back, and you’re not old. ” If you would have taken better care of your body, you wouldn’t have degeneration. They act as though this is normal; however, it is not normal; this is just a sign of the breakdown.
[00:29:23] Dr. Alex Jimenez DC*: You know, the magnitude of either of us uncovering or discovering where a person has an issue. All of these things have ways that we can help it. What’s crazy about it is that we have to go against the grain in our methods because you would not think exercise would be a helpful tool right for this. However, exercise is one of the best things for we have to calibrate that pelvis if it’s appropriate. It’s a herniated disc, and it’s a bad one. We have to go ahead and surgically remove that; if not, we do anti-inflammatories, do we do natural methods, and get that body working and calibrating. Sometimes what happens is these people come in. These individuals are patients who come in and suddenly have a pain that just crept up on them over the last couple of weeks. Sometimes they have a slipped injury, a slipped disc, or even a vertebra that’s been fractured for years and now presents with the issues. Sometimes it’s a neurological presentation. Sometimes it’s a metabolic disorder like metabolic syndrome, and they have an inflammatory condition. What I’ve noticed, and I’m sure you’ve seen it too, is that these people who have sciatica live with this looming monster. It’s almost like a snake that lives in their pants, and when it bites them, it gets their whole leg. It disrupts people’s lives. Figuring out where the cause is is very important. So as we go over these things, I mean, it’s essential to go over the regions. I’ve even seen patients where they come in thinking it was sciatica. And sure enough, it’s sad, but it’s a tumor. And in that situation, we move on too quickly. I got to tell you, in the situations where we’ve had it, we’ve had great teamwork and resolved many issues for a lot of patients.
[00:31:06] Dr. Mario Ruja DC*: That’s the beauty of how we think, Alex. We think in terms of integration. So, just because you have a hammer, everything doesn’t look like a nail. We are chiropractors, but at the same time, we are physicians. And what that means is that we know about physiology, anatomy, neurology, all of that. So we can understand that the pain sensor is not the problem. The pain sciatica is not the problem. We look for the causation of the problem, Alex. And that is in many ways, the misalignment, the compression, the inflammation, the disc bulging again, bone spurs, and many times people will say, Well, I have bone spurs because I’m getting old. No, bone spurs are created because there is a misalignment and lack of calibration in your spine where the body is attempting to self-regulate, self align, and it’s called the wolf’s law. You know, its law is the same principle that deals with the fracture healing fracture where you have pressure, that’s where you have increased calcification. Alex, is that correct?
[00:32:22] Dr. Alex Jimenez DC*: It’s the same thing when you work out; when you work out, you get calluses right because the body responds to stress by increasing and protecting the tissue. The same thing happens with the spine. Suppose it starts unloading improperly, then before you know it, the wolf’s law kicks in, the osteoclast start losing, which are the ones that take away bone, and the osteoblasts start winning. Then you have an increase of bone growth in a direction, usually in the direction of the force. So, in essence, the body tries to protect it, so you can imagine if someone’s going like in the leaning tower. Well, it’s on this side that the body protects it to prevent it from falling over. So, in essence, as we look at these degenerative diseases, we try to get them early on, and we try to mobilize. In most scenarios, we can help the individual by different methods and different techniques. And we use a lot of other methods and techniques to help individuals through this process.
Spinal Stenosis
[00:33:18] Dr. Mario Ruja DC*: I want to go through a couple of points. You know, we’re talking about spinal stenosis. Again, the start of spinal stenosis is the misalignment of your spine, which chiropractic has the beautiful art. This is the art and science of correcting that. So the more alignment, the more clarity, the more balance you have in your spine. The more maintenance you receive to your spine, the less spinal stenosis you will have later on in your life. Or again, spinal stenosis. You know, the other one that we’re looking at is degenerative disc disease or disc herniation. I believe that I look at the body in the 25+ years of my practice; the better maintenance you give your body, the fewer issues, and the less breakdown wear and tear you will have later on in your life. So I look at is that we are anti-aging doctors in terms of biomechanics, so we help the body maintain its optimal function for a more extended period. So that way, when you’re in your 60s and 70s, and 80s, you can walk by yourself without a cane, and you can function. You can do a squat. I love fitness calibration every time, you know. Danny is awesome. With PUSH, Danny is tremendous in terms of a fitness core. And this is where the synergy comes in. The more miles, the more wear and tear, the more pounding you put on your body. The more maintenance you need, the more recovery work. And too many people, Alex, have this idea like, Oh, my back hurts, I just need to squat more. I just need to do more weights. I just need to be in a gym, no. It’s like me telling you I don’t need count maintenance and tune-ups on my car. I just need to drive it more now. So the more miles you put on your bag, the more you squat, the more calibration you need. Why? Because eventually, your body is going to go out of alignment.
[00:35:32] Dr. Alex Jimenez DC*: You know, as we look at disorders, like you said, spinal stenosis. There are many reasons we can have spinal stenosis, from a disc to just arthritic issues. But when we have an individual who suddenly has issues, OK, this is not a sudden, you know, kind of thing that the spinal stenosis doesn’t happen unless it’s a massive disc herniation that occurs in one moment. Yeah, but these things and what we’re talking about spinal stenosis, there are different reasons. And in the treatments are many methods are just, you know, microanatomy. There’s also a laminectomy which is to remove the pressure. But the bottom line is very little wrong with the nerve. The issue is compressive forces. So what do we have to do in the situation where there is a biomechanical imbalance in the pelvic girdle most of the time.
[00:36:20] Dr. Mario Ruja DC*: So it is structure impedes on the nerve.
[00:36:23] Dr. Alex Jimenez DC*: Yes. And as we do that, we evaluate that there are certain things like age, obesity, or even less of a life of activity. What are other things, Mario?
What Are The Occupations That Cause Sciatica?
[00:36:33] Dr. Mario Ruja DC*: Sedentary lifestyle, repetitive occupational motion?
[00:36:36] Dr. Alex Jimenez DC*: What kind of occupations would have sciatica?
[00:36:40] Dr. Mario Ruja DC*: Truck drivers. Why? By sedentary vibration. Eight to ten hours by sitting down. Secretaries, I mean, you can go on and on, people working in banks and teachers even.
[00:36:57] Dr. Alex Jimenez DC*: We have patients that go to the Southern Union railroad, the engineers, the vibration, the bouncing over 30 years of vibrating. Eventually, the bone activates the spine clouds, or you have spinal stenosis, and they have back disc issues, and they have degenerative diseases.
[00:37:14] Dr. Mario Ruja DC*: Athletes have a repetitive toque like a golfer. How many golfers do you know that have no back pain? None. How about baseball players?
[00:37:25] Dr. Alex Jimenez DC*: How about our buddy, Tiger Woods?
[00:37:27] Dr. Mario Ruja DC*: Yeah, what happened to him?
[00:37:28] Dr. Alex Jimenez DC*: Yeah, what did people think? People thought he might have been having some issues with alcohol. Still, the reality is he’s taking medication after surgery, and suddenly, he’s driving, and he probably forgot to take medicine. You know, they took a pill and started to get addicted, and this is the issue. We got to figure out how to fix these issues calibrating. But I got to tell you; there are a lot of ways we can help people. The issue is that once we understand where the problem comes from, the plan of attack can take off. There are different issues and different types of diagnoses. We have here a little bit of a window where you can take a look at that. You can see that sciatica is a symptom. It’s a presentation of syndromes. It’s a pain down the leg, but there are tons of reasons.
[00:38:14] Dr. Mario Ruja DC*: Now the causation is right there, right?
[00:38:17] Dr. Alex Jimenez DC*: Well, look at all of these things, and it is ridiculous.
[00:38:21] Dr. Mario Ruja DC*: Wow.
[00:38:22] Dr. Alex Jimenez DC*: The one people think about a lot is peraforma syndrome, and that’s only one component. Then when that doesn’t work, your little stretches, you try to figure out what’s causing it could be tendinopathy, it could be bursitis. Look at all these issues when we go in here; when we look at these particular issues, we can look at other subsequent areas causing problems. You mentioned it before the four sets; this degeneration redevelops the quadrant is formoral area.
[00:38:48] Dr. Mario Ruja DC*: So let’s make this simple. Otherwise, you know, people will listen to us and go; it’s a lot. It’s a lot, and this is like a fire hydrant, and I just have my mouth over it. Alex, this is what we got. Number one, it all comes down to foundation and function, right? If we go back on each of these things from, you know, four-set syndrome, this degeneration, ridiculous hip, you know, formoral impingement, quadrennial femoral, you know, abnormalities all of these. The root of all of these is the misalignment and lack of calibration of the neuromuscular system. I mean, when you go down to it, the majority, I’m not saying 100 percent, let’s not do that. Let’s not be silly tonight. No. The point is the majority, if we can do a better job for our community, if we can do a better job in terms of our athletes, is to create a maintenance calibration system for them, we would decrease a lot of these degenerative disc diseases and diagnoses, we would stop them before they blow up in their face.
Different Methods To Treat Sciatica
[00:40:19] Dr. Alex Jimenez DC*: Let me ask you this. What kind of things in terms of our diagnostic abilities, what we use different methods to diagnose?
[00:40:26] Dr. Mario Ruja DC*: I love MRI.
[00:40:28] Dr. Alex Jimenez DC*: In terms of sciatica, X-rays are good, but MRIs can tell you what the problem is.
[00:40:34] Dr. Mario Ruja DC*: That’s it, and we’re talking about like a Tesla ten. I don’t know if they have it, and I think it’s sorry about it. I just got crazy tonight. Nah, they didn’t make it. We’re going to get some calls. Tesla, what?
[00:40:46] Dr. Alex Jimenez DC*: We got a great radiologist, and they help us hone in on particular areas.
[00:40:54] Dr. Mario Ruja DC*: They have a three-point-o or something?
A Relationship With Your Radiologist
[00:40:59] Dr. Alex Jimenez DC*: The whole idea is a relationship with our radiologists. Our radiologists are our eyes and ears on the deep tissues. I can tell you that we do have the best radiologists working with us. We do. I mean, the city has some top-end radiologists people, and when we send them to them, they communicate with us and tell us where the problem is that from there we go at it from once we know where it’s at. We use cat scans. We use ultrasound. We use bone scans.
[00:41:29] Dr. Mario Ruja DC*: Why is it a question? OK, this is going to get a little crazy and a little nasty tonight. Why is it that most doctors, Alex order X-rays first? Why is it? I can never understand for myself. You know what I tried to go straight to the issue was to go to MRI. Why is it?
[00:41:51] Dr. Alex Jimenez DC*: The standard of care is many insurance carriers will want an X-ray first to see if it’s a degenerative bone structure to be able to bleed on that. But we all understand that the best possible option for actually assessing it is to kind of rule out some things. If you want to look at bone, you do a cat scan to do the soft tissues. Well, this is soft tissue. So then you do an MRI with contrast, and you can see the deep tissues and the separation and the inflammation for any prolonged issues occurring.
[00:42:21] Dr. Mario Ruja DC*: That’s why, to me, Alex, that makes sense if we’re looking at diagnosing disk and nerve issues, right? Why is it that we use an instrument many times and I see this and agree with you. All of the insurances are going in and saying, Hey, you need to do an X-ray first. We won’t let you do the MRI, do they? I’m like, but X-rays don’t show any soft tissues.
[00:42:46] Dr. Alex Jimenez DC*: I think it’s a common thing. It’s almost like when you go to a dentist, you know, they scan all the teeth. It’s pretty easy to generalize. You know, there are times when the standard of care is into that today? For the low back, the standard of care is an X-ray as an initial entry point. So from there, I’ve learned, and I have gotten this lately, that most insurance carriers are very open to allowing the individual based on a presentation to do whatever it takes. They don’t stop. That’s a real beautiful change that’s happened since I’d say for the last five years; it’s a whole different game. So we get to see that we do nerve conduction and nerve testing to see the speed at which the nerve pulses. So we can find that AMG’s electromyography and see how the muscles are. But you don’t need to be doing that stuff for sciatica when you know the person is in severe pain. Now, if you want to prove it, that’s when you do the NCBI. Other than that, the person will not come in telling you that they have pain. Now sciatica because I call it the scourge because it just annoys you. It stops you from doing, you don’t sleep, you get to lay down, and the darn thing just activates. And there you got this electric current preventing you sleep. People come in with their eyes bloodshot and unable to enjoy their lives. This changes the quality, and we need to fix these things.
Does Sciatica Cause Inflammation?
[00:44:09] Dr. Mario Ruja DC*: It affects families. Alex, let’s get down to it. You know what? It affects your relationship with your spouse, with your children, at work. You know, you go to work, and you’re angry. Yes, you’re just mad at the world, and people are trying to figure out, like, what’s wrong, man? And it’s like, “You know what? I’m dealing with stuff.” And then that chronicity after a while, you’re like, “I don’t know what to do. I’m taking too many meds. I’m taking 800 milligrams every day for like five months.”
[00:44:39] Dr. Alex Jimenez DC*: Let’s give the people out there who may want some information a little bit of insight into the other options they have. Because what’s the name of the game here? What are sciatica and inflammation? It’s what it always has and always will be. So what we got to do is do what we can, and many people ask me, What are my options? Well, we have here a breakdown of certain things, and we’re going to discuss these things in real extensive detail over the next couple of months. And we’re going to hit this thing as we will be dealing with sciatica and vitamin C, D, calcium. We’re going deep all these things, you can take a screenshot of this, and you can say berberine. We got glucosamine, ACL, carnitine, alpha-lipoic acid, ashwagandha, soluble fiber, vitamin E, green tea, turmeric. A lot of these things have a lot to do with metabolic syndrome. But guess what? When you have metabolic syndrome, which is what?
[00:45:36] Dr. Mario Ruja DC*: Inflammation.
[00:45:37] Dr. Alex Jimenez DC*: So what we’ve noticed, Mario, and correct me if you see something different.
Ashwagandha
[00:45:44] Dr. Mario Ruja DC*: I love that word ashwagandha.
[00:45:47] Dr. Alex Jimenez DC*: Yeah, I love it too.
[00:45:55] Dr. Mario Ruja DC*: It’s like, we’re going to meditate pretty soon, Alex.
[00:46:01] Dr. Alex Jimenez DC*: So, as we kind of look at these options, we really can discuss deep levels of biomedical science here, OK. Because everyone wants to know what we can do, but since we’re dealing with, let’s say, just on the angle of metabolic syndrome, again, we got to tie in another beast insulin. Insulin inflammation susceptibility. And here, we correlate. It may seem far away, but if you take a hundred people with metabolic syndrome, these people are susceptible to sciatica and the stuff we hold on to.
[00:46:46] Dr. Mario Ruja DC*: Let’s make it simple. How many people do you know with metabolic syndrome that don’t have back pain or sciatica? OK, let’s make it. Let’s make it simple.
[00:46:58] Dr. Alex Jimenez DC*: We got to tie together, and this is where we do it. National in clinical practice, what we do is we make these connections. And the bottom line is we start changing people’s habits, you know, simple things like instead of having a pop or something else only option you should have as green tea. Green tea is an antioxidant anti-inflammatory. We start changing the metabolic processes, begin cutting the gut grease, and all that starts happening.
[00:47:27] Dr. Mario Ruja DC*: OK. We’re mixing ashwagandha with gut grease. You know what? People are going to remember this forever, Alex.
[00:47:34] Dr. Alex Jimenez DC*: If you kind of see what we’re got, we’re saying it is complex. We can go down one rabbit hole and say we got the moment of truth or the thing that’s important. But the reality is that the low back causes neck pain. A lot of people will look at it and say, Why does that happen? Well, as Mario said, you know, God didn’t name it as neck pain. God didn’t call it lumbar spine. We named it the vertebral column. It’s the whole darn thing that is connected. From the moment you heal, strike your head feels the shockwave, right? So when we look at that, when we assess that, we can see that the body has a massive implication when some large nerve, late-deciding nerve, gets offset. So what we can do is first figure out, mitigate the issues, control them and come up with a treatment plan that works appropriately for the patients. So as we do these things, we will go over all those beautiful ideas that we have going on here. And I just wanted to let you know that we’re going to be discussing many more subject matters.
Vitamin D3
[00:48:35] Dr. Mario Ruja DC*: There it is vitamin D3. That is why I love vitamin D3, and it’s everywhere.
[00:48:43] Dr. Alex Jimenez DC*: Four hundred disorders. A 400 percent decrease in all risk mortality or times decreases disease mortality with vitamin D. This is like the magical thing? I mean, common sense. I mean, what’s our biggest organ, right? It’s the skin. So when we live in the sun city, right, what happens?
[00:49:07] Dr. Mario Ruja DC*: We absorb the sun’s rays.
[00:49:09] Dr. Alex Jimenez DC*: And that should be the healthiest.
[00:49:11] Dr. Mario Ruja DC*: Hey, I want to get crazy tonight. All right. Sun City vitamin D. We should be the healthiest on the planet.
[00:49:22] Dr. Alex Jimenez DC*: That’s it. I mean, it’s essential. So what did we get called about a couple of decades ago? Mario, you remember that we were named the fattest sweaty town in the country?
[00:49:35] Dr. Mario Ruja DC*: That angers me, and that should motivate and pump people up. That right there should be the wake-up call and the battle cry of El Paso and the whole region. Never again will you ever open your mouth and say that because we are the best.
Treatment Protocols
[00:50:00] Dr. Alex Jimenez DC*: We are. We are very family-based and a location and a community, but we suffer from metabolic syndrome, which implicates issues. And one of them is sciatica. I got to tell you; there isn’t a day that half my patients coming in have sciatica, and you and I have been doing this between 25 and 30 years, right? So as we’ve been pounding and fixing these disorders. And you’ve got to tell you there are studies where we see that when doctors of all different sorts refer for a surgical consult, there’s a high tendency to have surgical, you know, focus when you go to a nonmusculoskeletal special like a physical therapist or chiropractor, we kind of filter out the situation when in our path or an available position to see the lower back pain. They throw it into the orthopedic surgeon, and only five to 10 percent of most studies show that those become surgical the ones we send. About 50 percent are surgical. That means we do a great job of filtering out before they have that issue. In other words, we fix the problem, and the ones we do refer to these.
[00:51:17] Dr. Mario Ruja DC*: Yes, that’s right.
[00:51:19] Dr. Alex Jimenez DC*: Game on. So we want to make sure you know that you know that we need that for your orthopedist out there. We require that option, that modality, but we don’t do that kind of procedure. But it’s necessary for terms of the common treatment protocol, you know, the mainstay of sciatica.
[00:51:38] Dr. Mario Ruja DC*: It’s gabapentin. Just adding on to that, we refer to real cases, you know? When someone comes in, they need it. It’s not like, Oh, you know what? We’re going to waste people’s time. They need it. Because again, the new model now for back problems and especially sciatica is noninvasive. OK, noninvasive care first for at least two to three months.
[00:52:10] Dr. Alex Jimenez DC*: Well, you know, I’m on my point of view on those guidelines. You know, every person is different.
[00:52:17] Dr. Mario Ruja DC*: Yeah. ODG guidelines, Alex.
[00:52:21] Dr. Alex Jimenez DC*: And what happens is that you can oversee the treatment protocols when we look at these dynamics.
[00:52:31] Dr. Mario Ruja DC*: Yeah, there it is. The treatment protocols. You know, I look at treatment. Chiropractic care, a lifestyle change. Metabolic syndrome, we’re looking at physical therapy; we need everyone on board. Acupuncture, drugs again. Medication for pain. Anti-inflammatory muscle relaxers. Nutraceuticals, herbals, steroid injections. Yeah, those are what we call lying like the second you, even with a lot of the patients, it’s after conservative care by the time they get to that phase. And then, of course, you have surgery, surgical procedures. So yeah, you must go with our patients. We go from noninvasive to invasive care.
[00:53:36] Dr. Alex Jimenez DC*: These procedures are the ones we do.
[00:53:47] Dr. Mario Ruja DC*: Now with those. And that’s a foam roller right at the storm rolling, that means releasing the goods, the pure performance right there. And again, a lot of our viewers will think, hold on. I can’t even walk, and I can’t do that. But again, this is the secondary phase, Alex. This is the second phase. Furthermore, we’re not getting people out, and all of a sudden, they can’t walk in there. They’re, you know, doing box jumps. No, this is the secondary self first care correct release the pressure brake and the pain pattern and then stabilize and correct the muscle imbalance. So those are things because I think a lot of times, you know, many people ask me like, “Oh, you know what? I want to go work out.” I’m going on like, Hey, slow down, superstar, let’s not workout. You know, let’s not work out. Let’s correct the problem. Calibrate your back. Then you work out, and then you do a process of what I call periodicity. That means you scale it. You got to crawl before you walk and walk before you run. So let’s not be superheroes, and a lot of people just aren’t patient.
[00:55:08] Dr. Alex Jimenez DC*: I agree with you.
[00:55:09] Dr. Mario Ruja DC*: They’re not patient. They want things now. You know this has been created. This sciatica and back problems have been created for years. No maintenance for like 10 20 years. And they expect to walk into the office and, in one visit, do jumping jacks. You know what? Sorry but it’s not going to happen. So that’s where people want again. We do our best, but we don’t look for quick fixes. If you wish for the symptoms to go away but are not corrected, then you’re going to deal with the problem. That’s going to be lingering for years and years, and it’s going to get worse, you know, and those pain sensors. This is what’s so important. God created a body such as such a miraculous system, and we can’t even duplicate this. The most potent technology developed to wear the sensors, the awareness, proprioception within our body, and pain is effective. I often tell people, don’t block the pain because it is healthy because it tells you to stop. That pain is that red light on your dash that says, don’t drive the car, don’t park it, and fix it. Please don’t unplug the light and keep driving it. And this is where our society and our, you know, immediate care. I want things now. I can’t wait. Just like fitness, you know, people want to get fit in like like a week.
[00:56:47] Dr. Alex Jimenez DC*: Like, come on, it’s not going to happen.
Conclusion
[00:56:50] Dr. Mario Ruja DC*: Same thing with your health. It takes time, and you have to get the proper diagnosis. You know, the intense lab work, the genomics, the inflammatory. I mean, this is like I tell people, you’ve got to invest in your health or your sickness. Either way, you’re going to spend the money, either way, but once, you’re going to enjoy the fruits of that investment. The other one, you’re just going to drag. So the process of diagnostics from MRI’s, the process of diagnostics to look at metabolic syndrome, to look at your inflammatory process, that’s an investment. And then with those tools with that information, you got to have created baselines, Alex. If you don’t know where you’re at, you don’t know where you’re going. Now that’s what I would say is I want to motivate and empower people to invest in that process because it’s not an overnight thing and people want it. I tell them that they have got to understand. Be disciplined, be relentless and see the results for life instead of patching up your health.
[00:58:15] Dr.Alex Jimenez DC*: This is very dear and near to all of us here because sciatica affects so many individuals. We’re going to be discussing all these issues one section at a time. We’re going to bring an explanation. We’re going to give you an answer. We’re going to provide you with options. We’re going to provide you with treatments. We’re going to come up with a way that we’re going to find the best possible treatment protocol for you. And if not, we’re going to give you at least a basis to ask your doctors exactly what the best approach is, and you’re going to at least know the different directions you can take because we must understand this disorder. It may be simple to many people, but it debilitates you. You integrate way when you have it. We’re going to bring this to you. If you ever want to ask us personal questions and call us personally, Mario makes himself available 24-7 via phone number (915)494-4468. Always has been, and you get called all the time as he is right now. My phone number is(915)850-0900. And here we have, Mario, and I want to thank you all for allowing us to go over these things. This is also Mario’s website at: rujahealth.com. It’s easy, and it’s a fantastic site. We got me over here. This is my address and my phone, and then there’s Daniel Alvarado, where he works from the PUSH Fitness center. So we welcome you guys to see what’s cooking here and seeing what’s happening, and we wish you the best of everything that’s happening. So as we go through that. Mario, it’s been a blessing, brother and I look forward to going over more details with you in the next couple of days, and we will start recording more and more as time goes on. God bless.
Disclaimer