Table of Contents
Introduction
When the body has an underlying condition that can change how a person looks, this is due to unwanted factors are in the body and starting to cause chaos in the body that can develop into chronic conditions. When these conditions start to affect the gut, the brain, the musculoskeletal systems, this can lead to a cluster of conditions known as chronic metabolic syndrome. In this 2 part series, we will be taking a look at what different kinds of treatments can not only dampen the effects of chronic metabolic syndrome but also improve brain health. Part 1 took a look at what chronic metabolic syndrome is and how its symptoms can affect the brain. By referring patients to qualified and skilled providers who specialized in neurological services. To that end, and when appropriate, we advise our patients to refer to our associated medical providers based on their examination. We find that education is the key to asking valuable questions to our providers. Dr. Alex Jimenez DC provides this information as an educational service only. Disclaimer
Can my insurance cover it? Yes, in case you are uncertain here is the link to all the insurance providers we cover. If you have any questions, please call Dr. Jimenez at 915-850-0900.
Metabolic Syndrome
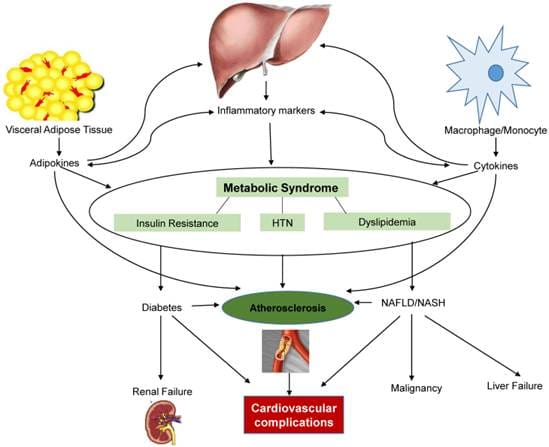
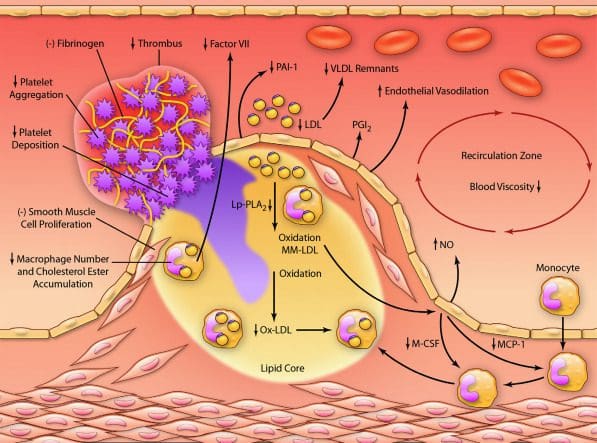
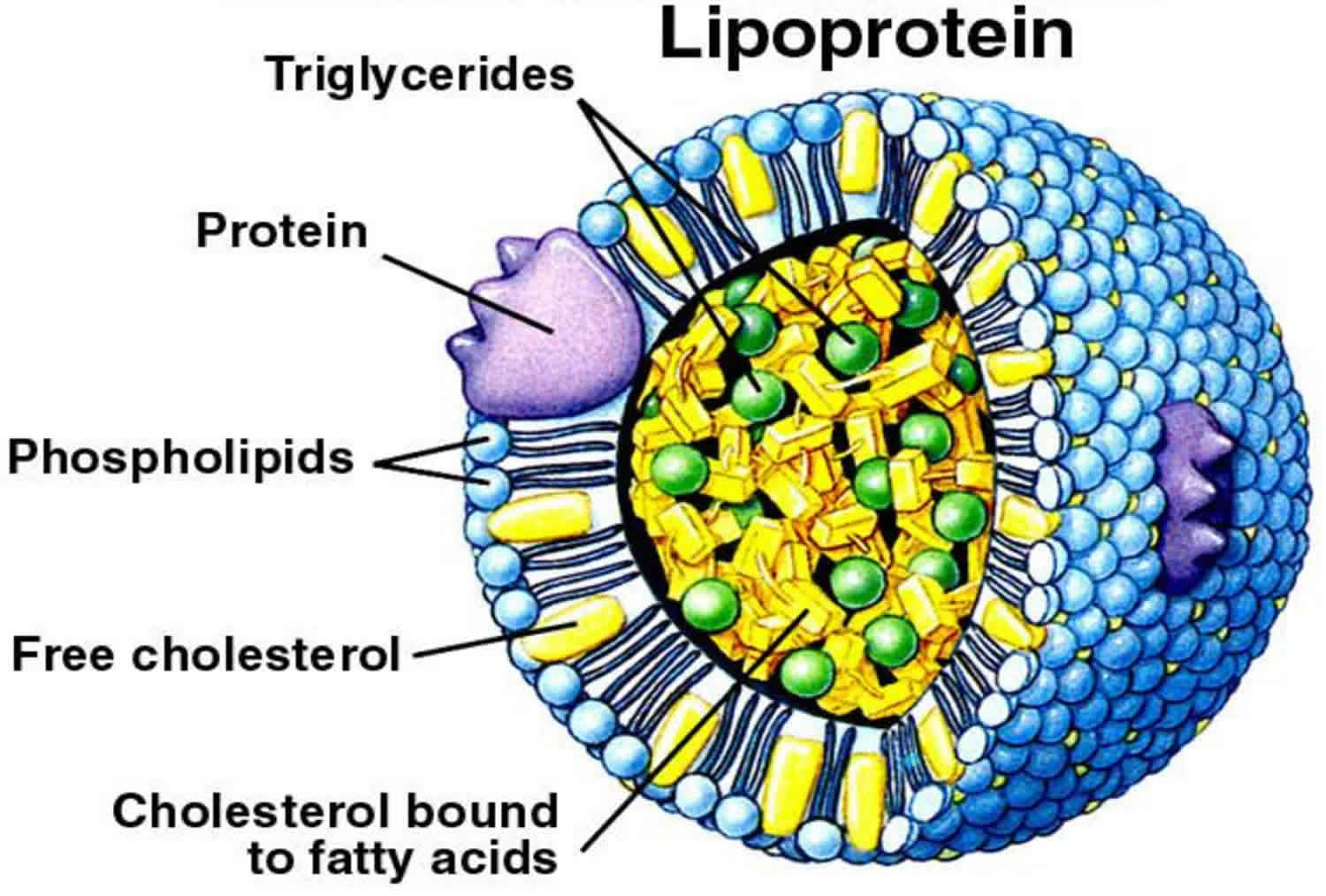
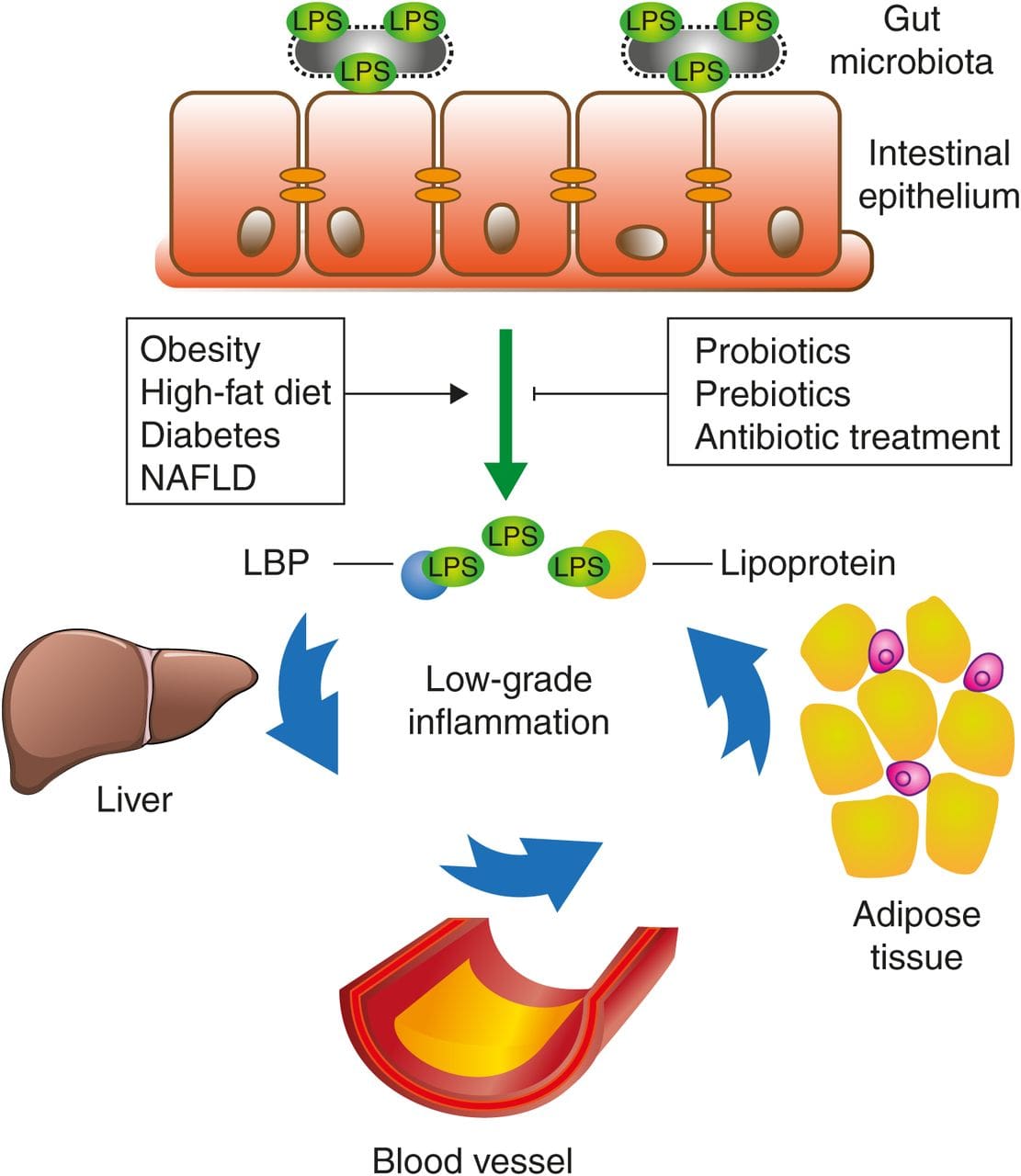
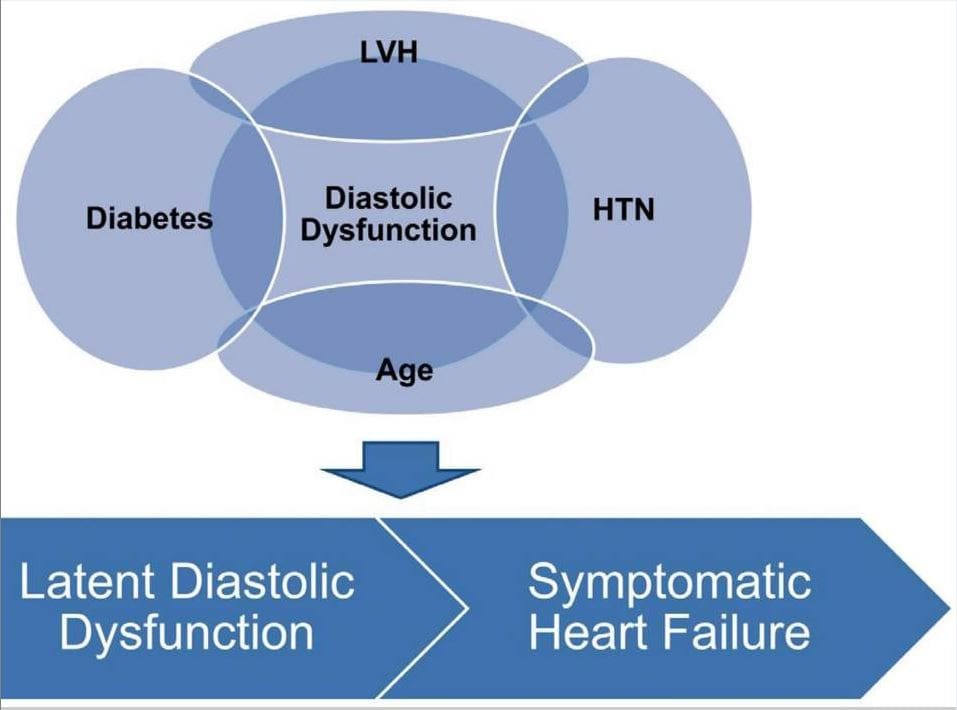
So metabolic syndrome, as research shows, is a cluster of conditions that can develop over time in the body. Some of the conditions that can cause the development of metabolic syndrome can include high blood pressure, increased blood glucose levels, excess body fat around the waist, and abnormal triglycerides. Other factors that metabolic syndrome can cause the body to develop apple and pear-shaped bodies for both males and females over time. Other research studies show that people with metabolic syndrome can have it increased with age and can cause neurodegenerative disorders in the brain.
How Does It Affect The Brain?
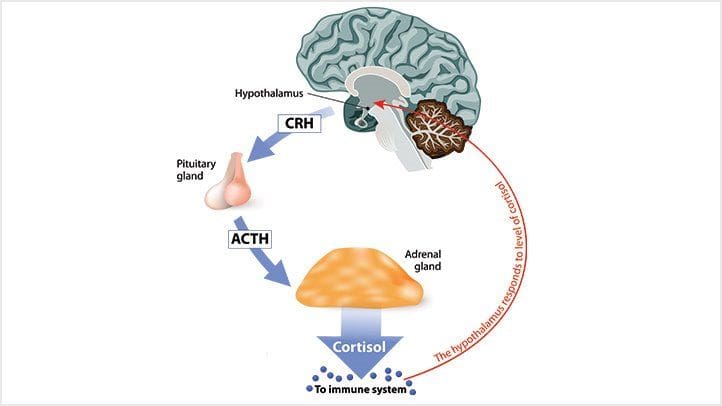
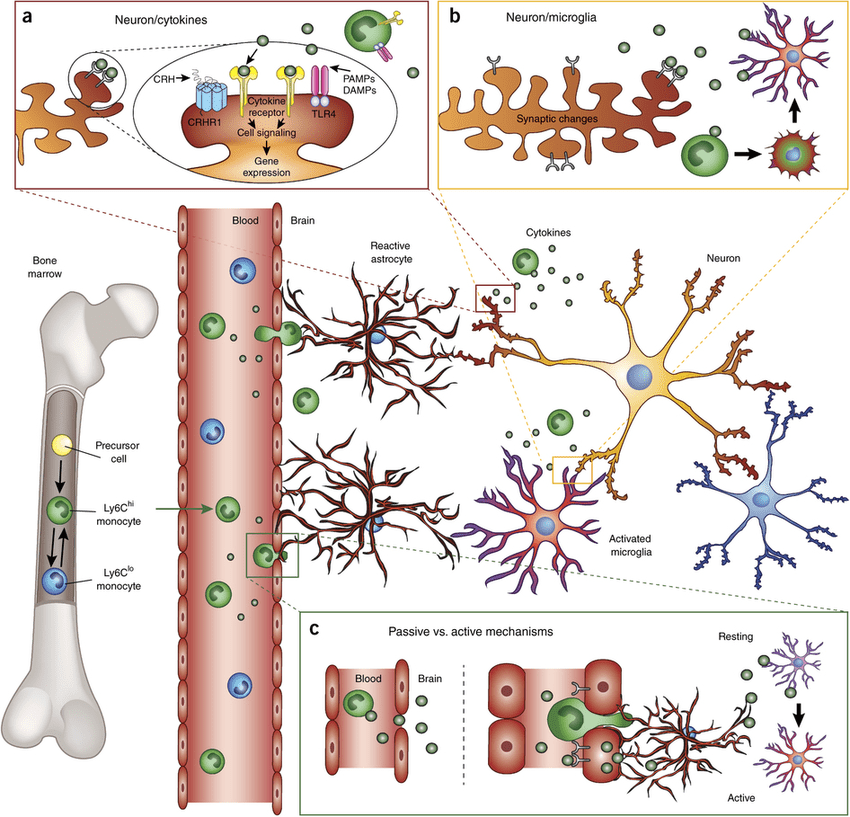
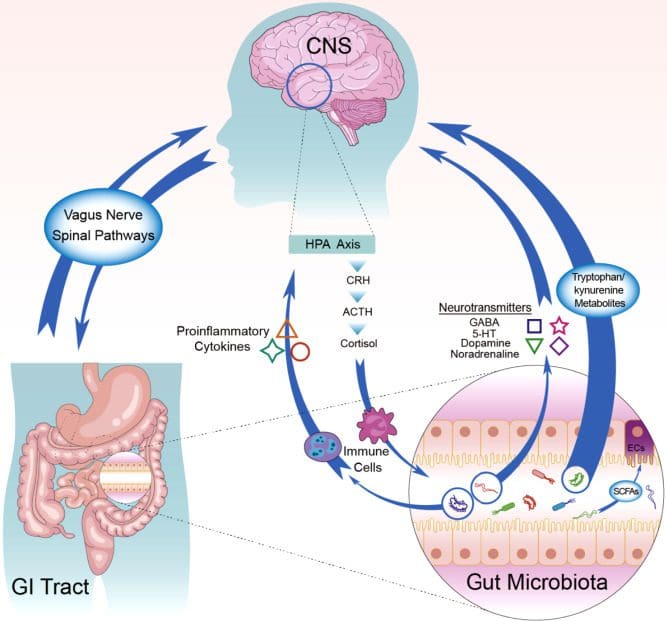
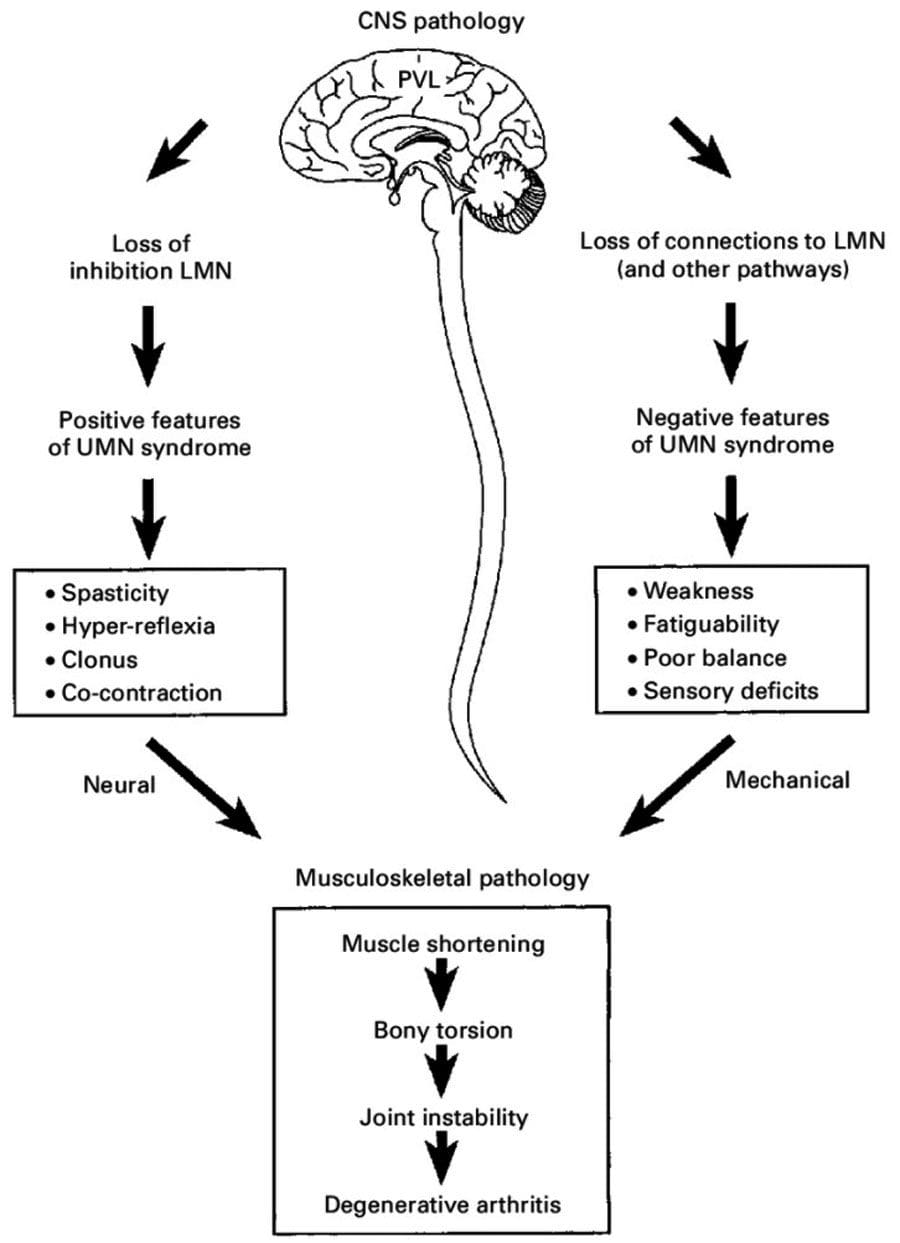
Since metabolic syndrome is a cluster of conditions that can cause the body to develop chronic illnesses over time, it is important to know that it can affect the brain as well. The brain is part of the central nervous system and it sends out signals all throughout the body and vice versa. These neuron signals help send out information from the brain to the entire body by making sure that it stays functional. When chronic conditions like metabolic syndrome start to disrupt and affect the signals from the brain. Studies have found that metabolic syndrome can play a significant role in the progression of Alzheimer’s disease and other neurodegenerative diseases that can affect the brain. This is due to neuroinflammation and it can cause the inflammatory cytokines to cause damage to certain parts of the brain.
HCTP Therapy

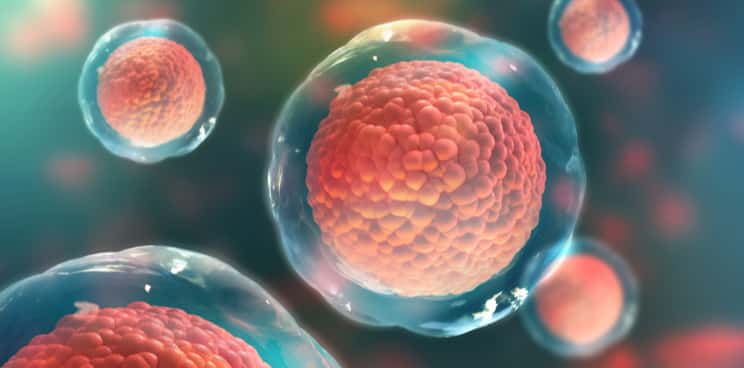
HCTP (human cellular tissue products) or stem cells* treatment has been used in both international and nationally affiliated clinics and distribution organizations for individuals that are dealing with chronic issues. HCTP therapy is part of regenerative medicine treatment since HCTP can help boost the body’s own natural healing process by regenerating damaged cells, diseased tissues, and organs back to their original state and helping the individual be pain-free. With more upcoming research on the beneficial properties of HCTP, individuals can start their wellness journey without chronic pain.
Treatments To Improve Brain Health
The brain’s main job is to make sure that the body is functioning properly and that it’s sending out neuron signals all throughout the body in a bidirectional connection. When there are unwanted pathogens that enter the body and start to disrupt those signals from reach to the brain, it can cause neurodegenerative disorders to develop. By making small changes in a certain lifestyle that a person is used to can actually help not only improve their body but also can improve their brain health. These changes can be a variety of things that can help improve the brain like:
- Eating nutritional foods
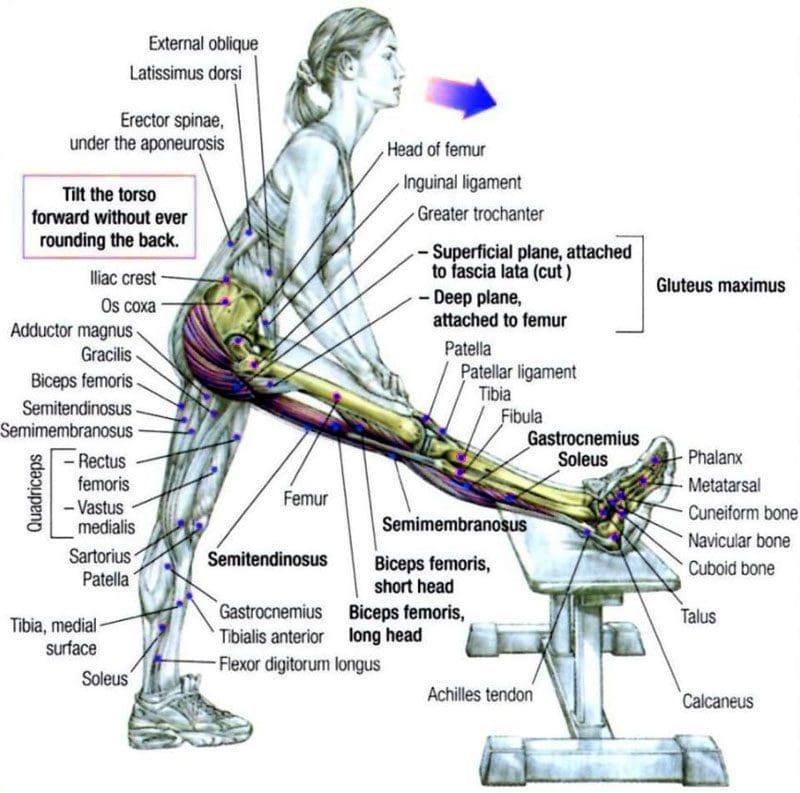
- Exercising (both mentally and physically)
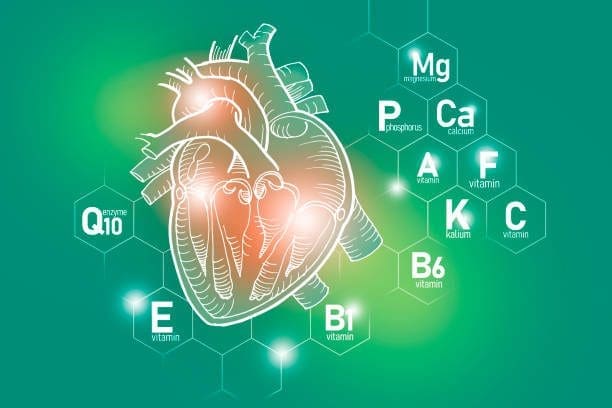
- Taking supplements to improve brain health
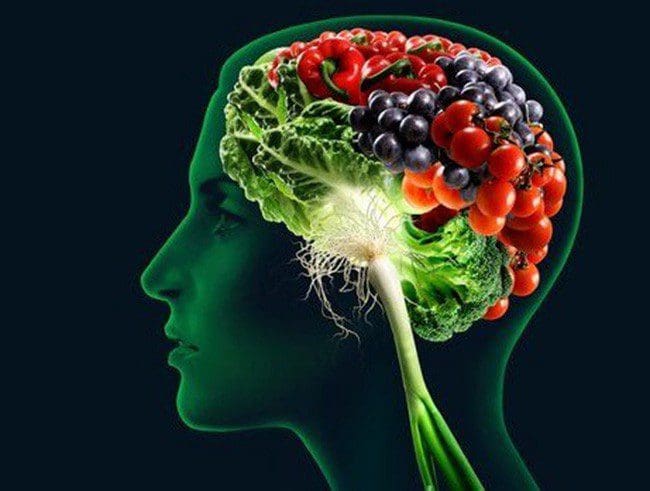
Nutritional Foods
Since the immune system relies on white blood cells that produce antibodies to combat bacteria, viruses, and other invaders, studies have found that eating nutritious foods that are beneficial to the brain are the same ones that actually help protect the cardiovascular system. As part of the central nervous system, the brain needs certain nutritional foods to stay healthy and keep the body from dysfunction. Research studies have found that in order for the brain to function the entire body, it needs omega-3 fatty acids and antioxidants to dampen the effects of inflammation and cellular stress from progressing in the brain while also helping with building and repairing the brain cells. Not only that but a plant-based diet has also been shown to reduce inflammatory biomarkers, but eating food that contains fiber can also lower BMI, which is linked to improved immunity.
Exercise
Research studies have found that by changing a lifestyle through exercising can actually reduce age-related cognitive decline and neurodegeneration. By maintaining a healthy weight can also benefit the immune system while also providing behavioral benefits to the brain as well. Other studies have also found that aerobic fitness can actually enhance the brain’s cognitive strategies to respond effectively to any challenges a person might face with when dealing certain situations. By making sure that the brain gets a workout either intellectually or physically can provide beneficial effects to the brain and the body.
Supplements
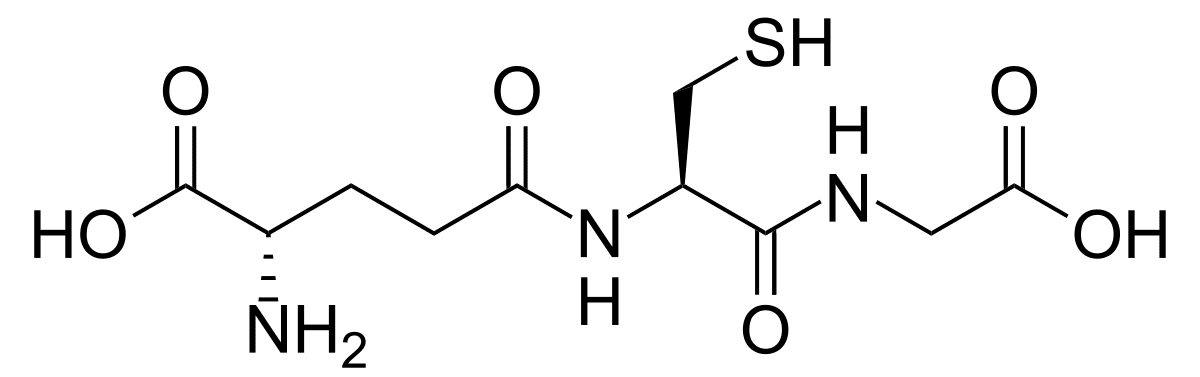
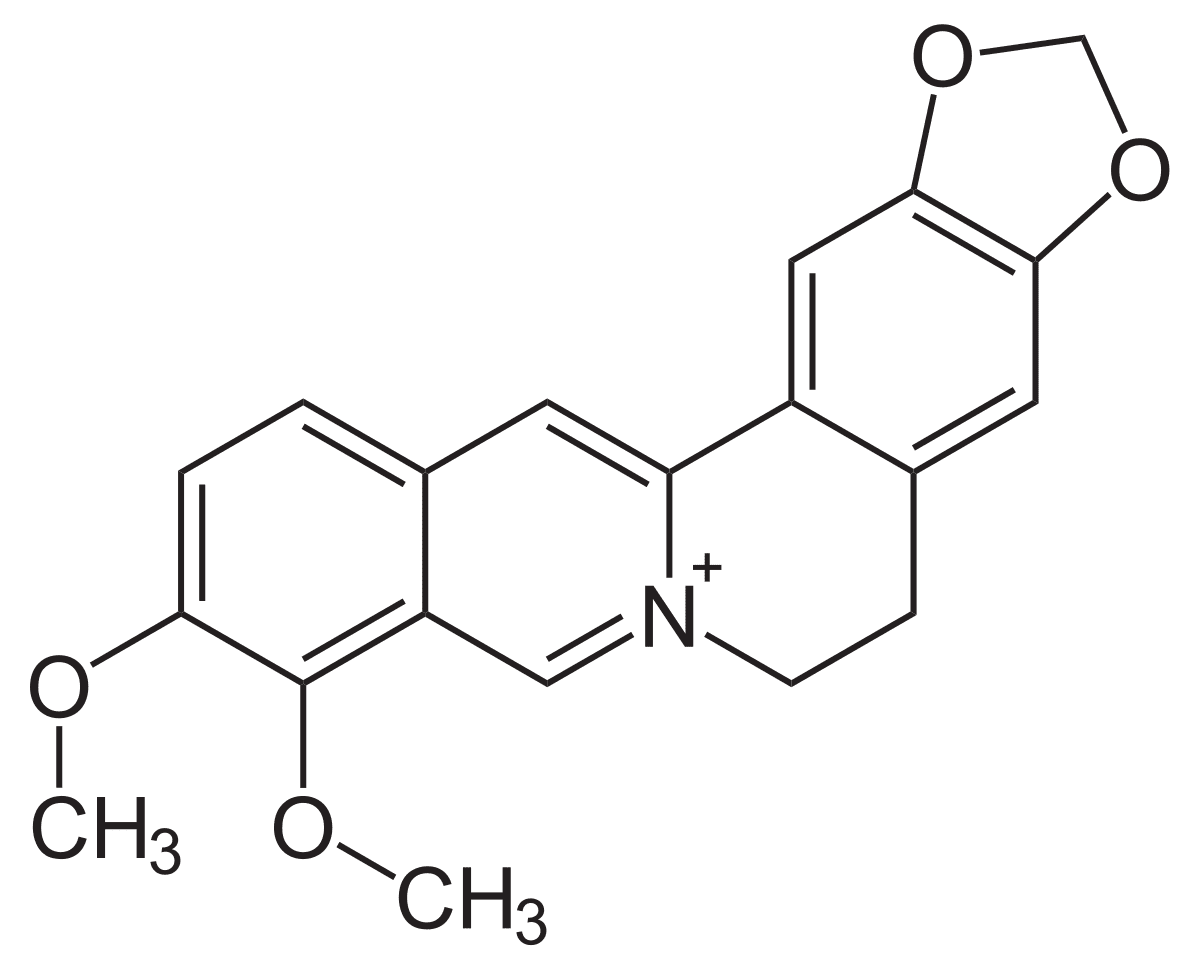
As stated previously, foods that contain omega-3 fatty acids and antioxidants are essential for optimal brain health. For omega-3 fatty acids, studies have found that the effects of EPA, DPA, and DHA from omega-3s can dampen the effects of a variety of neurodegenerative and neurological disorders while optimizing brain health. For antioxidants, research studies have found that when oxidative stress enters the brain capacity and starts to rise up it can cause neurodegenerative disorders and cause neuronal cell death in the brain. By consuming antioxidants either through food or supplemental form can dampen the effects of oxidative stress from the brain and provide neuroprotection.
Conclusion
All in all, by utilizing these small changes in the body, a person can begin to feel much better with the right type of foods and supplements that can optimize their brain health. Even doing puzzles or physical exercising can help provide neuroprotection to the brain from harmful pathogens. When an individual starts taking care of their body and their brain health, it can help relieve chronic illnesses that they might not realize that they have, while also feeling good about themselves.
References
Arshad, Nurul `Ain, et al. “Metabolic Syndrome and Its Effect on the Brain: Possible Mechanism.” CNS & Neurological Disorders Drug Targets, U.S. National Library of Medicine, 2018, https://pubmed.ncbi.nlm.nih.gov/30047340/.
Baek, Seung-Soo. “Role of Exercise on the Brain.” Journal of Exercise Rehabilitation, Korean Society of Exercise Rehabilitation, 31 Oct. 2016, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5091051/.
Burgess, Lana. “12 Best Brain Foods: Memory, Concentration, and Brain Health.” Medical News Today, MediLexicon International, 2 Jan. 2020, https://www.medicalnewstoday.com/articles/324044.
Dyall, Simon C. “Long-Chain Omega-3 Fatty Acids and the Brain: A Review of the Independent and Shared Effects of EPA, DPA, and DHA.” Frontiers in Aging Neuroscience, Frontiers Media S.A., 21 Apr. 2015, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4404917/.
Gomez-Pinilla, Fernando, and Charles Hillman. “The Influence of Exercise on Cognitive Abilities.” Comprehensive Physiology, U.S. National Library of Medicine, Jan. 2013, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3951958/.
Lee, Kyung Hee, et al. “Neuroprotective Effect of Antioxidants in the Brain.” International Journal of Molecular Sciences, MDPI, 28 Sept. 2020, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7582347/.
Medical Professionals, Cleveland Clinic. “Metabolic Syndrome: Causes, Symptoms, Diagnosis & Treatment.” Cleveland Clinic, 13 Apr. 2019, https://my.clevelandclinic.org/health/diseases/10783-metabolic-syndrome.
Publishing, Harvard Health. “Foods Linked to Better Brainpower.” Harvard Health, 6 Mar. 2021, https://www.health.harvard.edu/healthbeat/foods-linked-to-better-brainpower.
Staff, Mayo Clinic. “Metabolic Syndrome.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 6 May 2021, https://www.mayoclinic.org/diseases-conditions/metabolic-syndrome/symptoms-causes/syc-20351916.