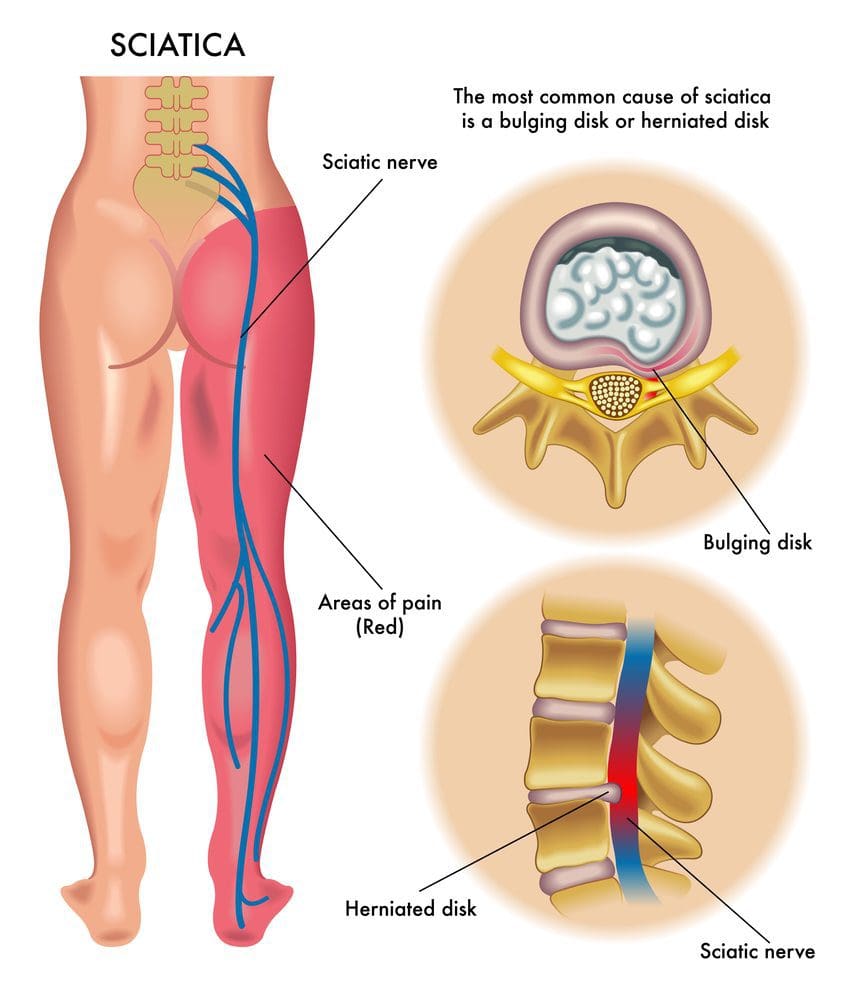
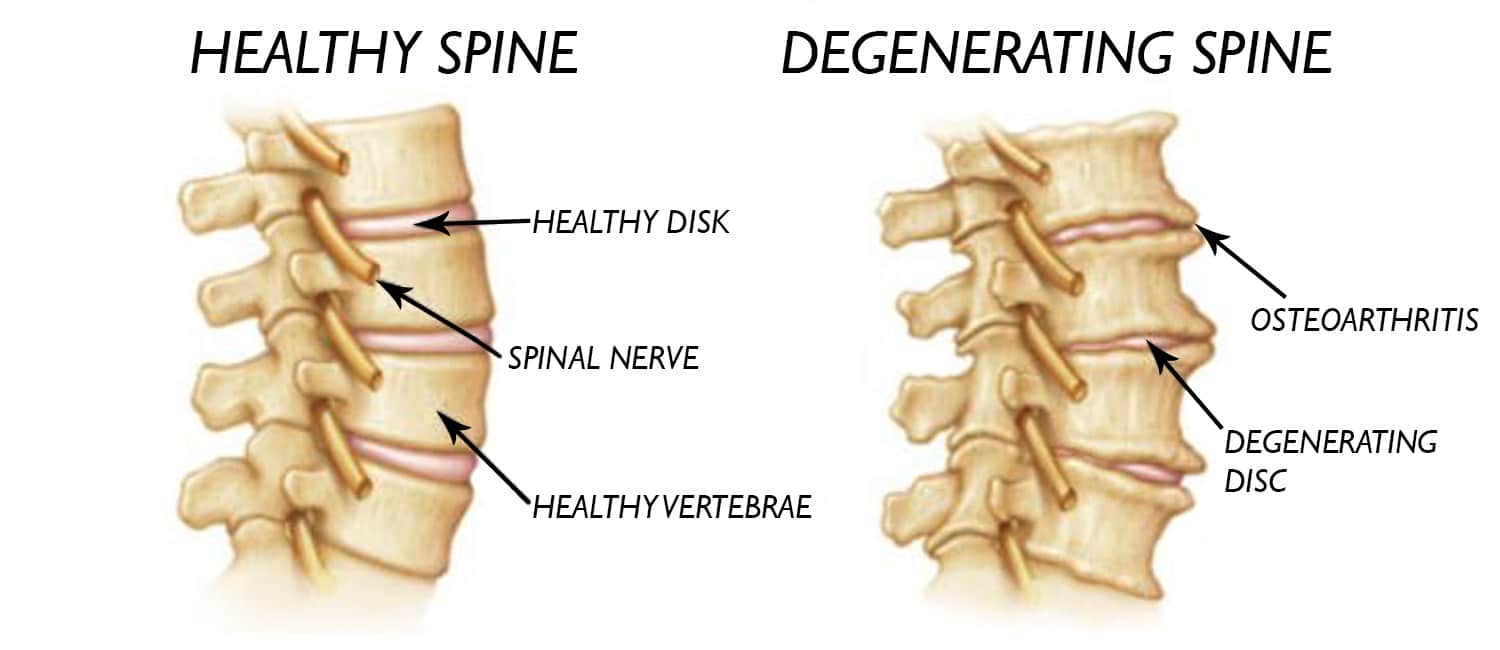
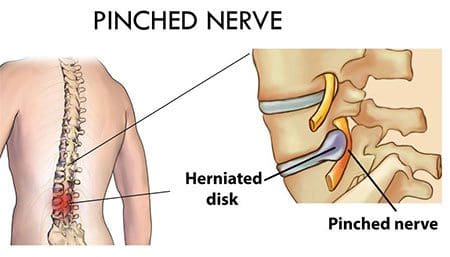
Sciatica is a radiculopathy, which is irritation of the nerve as it exits the spine and is typically caused by compression/pinching along the nerve’s path. Most sciatica cases improve within a few weeks of the injury incident. Left untreated, it can become chronic sciatica and can have long-term repercussions and effects. A herniated disc is the most common cause if it bulges next to the nerve; it can pinch off the nerve or leak fluid onto the nerve, causing inflammation, swelling, pain, numbness, and weakness. Another common cause is spinal stenosis. As the body ages, the canal through which the nerve and spinal cord run can begin to narrow, placing pressure on the nerves. Then there are muscle spasms, spinal fractures, and spinal cancer. Anything that changes the curvature of the spine, including pregnancy, can cause sciatica.

Table of Contents
Repercussions From Sciatica
The repercussions can vary or be a combination that includes:
Chronic Pain
The pain can be anywhere along the nerve; typically, it travels from the lower spine through the buttocks, down the back of the leg, and into the foot.
- The condition can cause various types of pain: Burning, electrical, or shooting pain in the low back.
- Symptoms can come and go and may present only when sitting, standing, lying, or engaged in a particular activity.
- The severity of the pain can vary from mild to severe, mildly uncomfortable, to limiting function.
Posture Problems
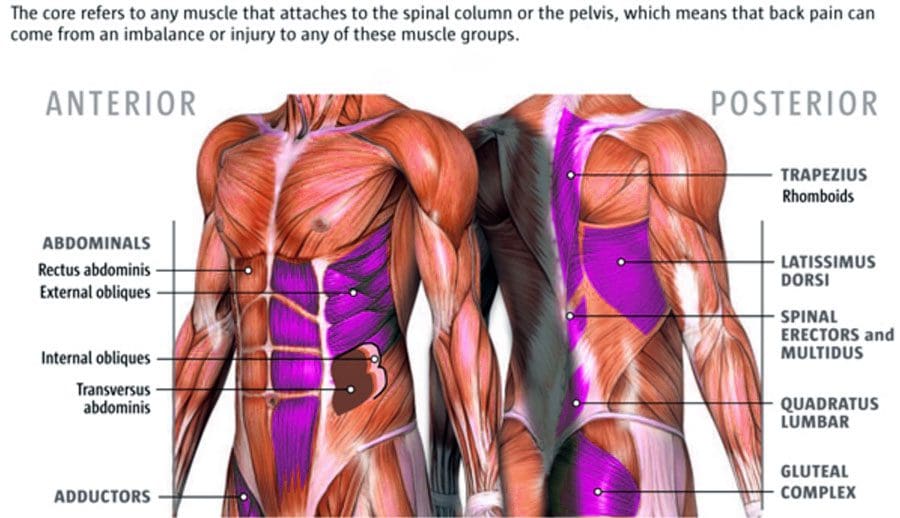
- When the body experiences chronic pain in a localized area, the body’s natural reaction is to avoid placing pressure, twisting or bending, or using a specific body part, manipulating healthy posture or walking gait to protect the low back or legs from pain.
- This is referred to as muscle/posture guarding, which removes pressure from the site but alters the body’s natural alignment, affecting the spine’s characteristics and causing adverse side effects, like upper back and neck pain, headaches, and fatigue.
- Unhealthy and awkward postures can negatively affect digestion, organ function, and breathing.
Loss of Balance
- Sciatica commonly causes numbness and tingling in the leg, calf, foot, and toes.
- The hidden danger behind numbness; it alters the body’s proprioception or awareness of its position.
- When proprioception becomes inhibited or altered, communication signals from the body to the brain/vice versa get jumbled/interrupted, confusing the brain, throwing the body off balance.
- This can result in falling injuries.
Numbness or Weakness
- Sciatica is more problematic if the pain comes with neurological symptoms like numbness, muscle, or leg weakness.
- This means there is an increased level of possible nerve damage if muscular weakness, which requires aggressive treatment.
Declining Reflexes
- Depending on where the nerve is compressed, pain and numbness can affect the lower leg area and feet.
- Damage to the nerve can cause the inability to flex the foot up.
- The knee-jerk reflex, known as the patellar reflex, is the kicking motion of the lower leg when tapped on the patellar tendon.
- Sciatica can numb the area, causing a delayed reaction or severe unresponsiveness to stimulation.
Permanent Nerve Damage
- If left untreated, neurological symptoms like numbness and leg weakness can progress to permanent nerve damage.
- However, this happens rarely but explains the importance of taking the injury seriously so full recovery is achievable.
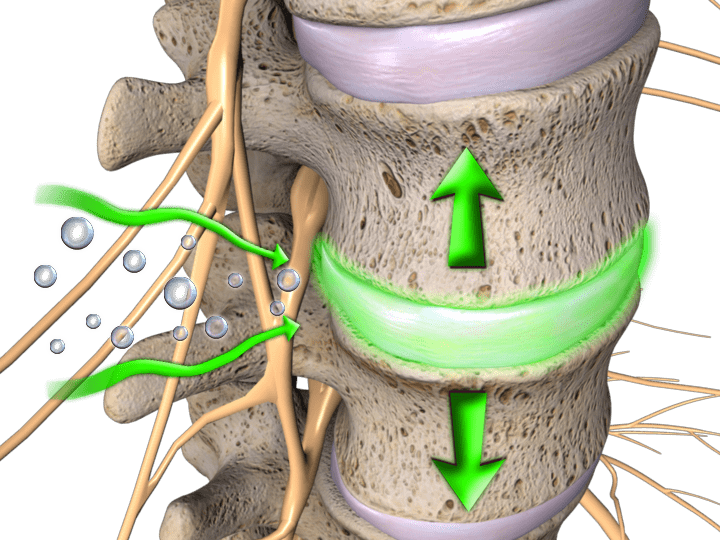
Non-Surgical Sciatica Relief
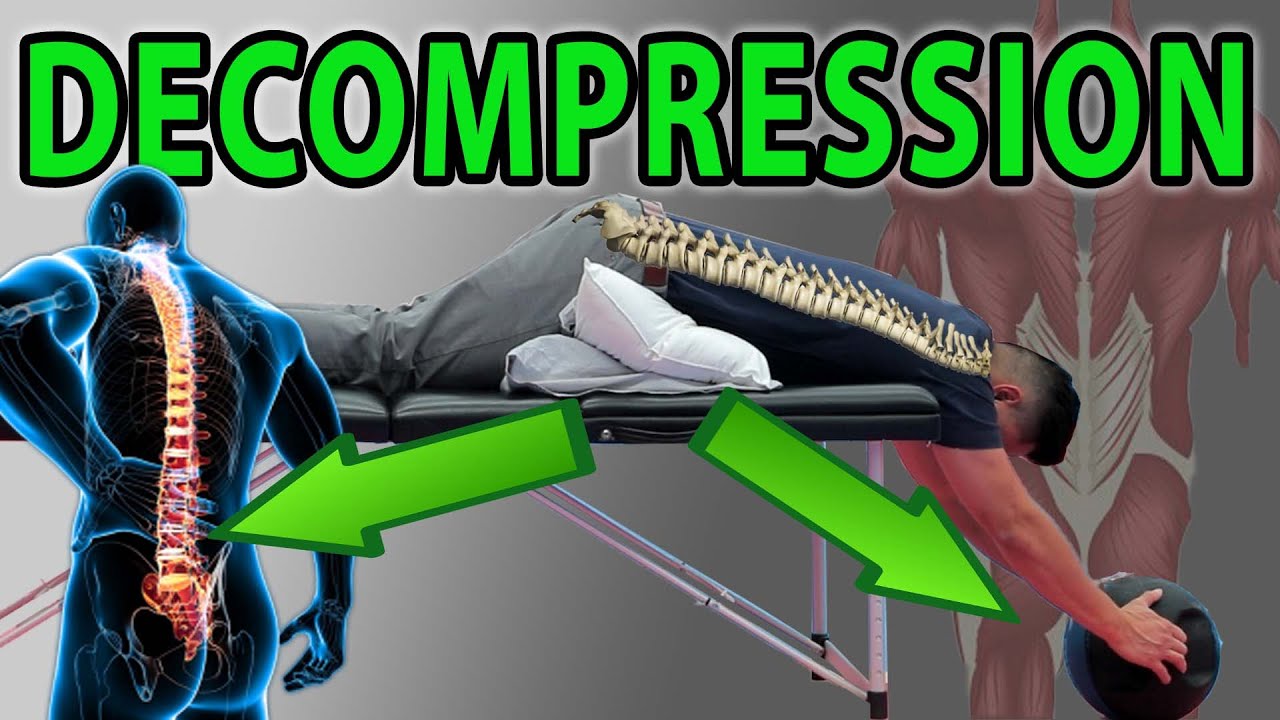
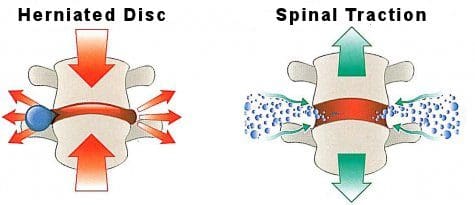
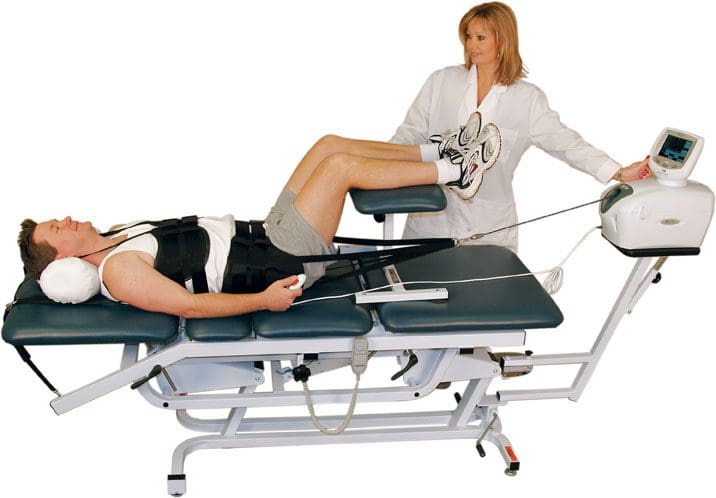
Spinal Decompression Effective Long-Term Solution
References
Berry, James A et al. “A Review of Lumbar Radiculopathy, Diagnosis, and Treatment.” Cureus vol. 11,10 e5934. Oct 17 2019, doi:10.7759/cureus.5934
Davis D, Maini K, Vasudevan A. Sciatica. [Updated 2022 Feb 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507908/
Giuffre BA, Jeanmonod R. Anatomy, Sciatic Nerve. [Updated 2021 Jul 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482431/
Nori, Subhadra L. and Michael F. Stretanski. “Foot Drop.” StatPearls, StatPearls Publishing, Dec 15, 2021.