Table of Contents
Introduction
The rotator cuff works together with the shoulder, providing movement and a full range of motion. The shoulders are one of the largest and most complex joints that can succumb to injuries that can make the shoulders unstable and cause unwanted pain-like symptoms to affect not only the shoulders but also the arms and the neck. These pain-like symptoms are caused by myofascial pain syndrome or trigger points. Trigger points can create small knots along the muscle fibers in any muscle group and causes referred pain to different locations in the upper body. One of the muscles that can be affected by trigger points is the teres minor muscle. Today’s article examines this muscle, how trigger points affect the teres minor muscle, and managing trigger points associated with the teres minor muscle. We refer patients to certified providers who specialize in musculoskeletal treatments to aid individuals suffering from trigger points associated with shoulder joints and the teres minor muscles. We also guide our patients by referring them to our associated medical providers based on their examination when appropriate. We ensure that education is the solution to asking our providers insightful questions. Dr. Jimenez DC observes this information as an educational service only. Disclaimer
What Is The Teres Minor Muscle?
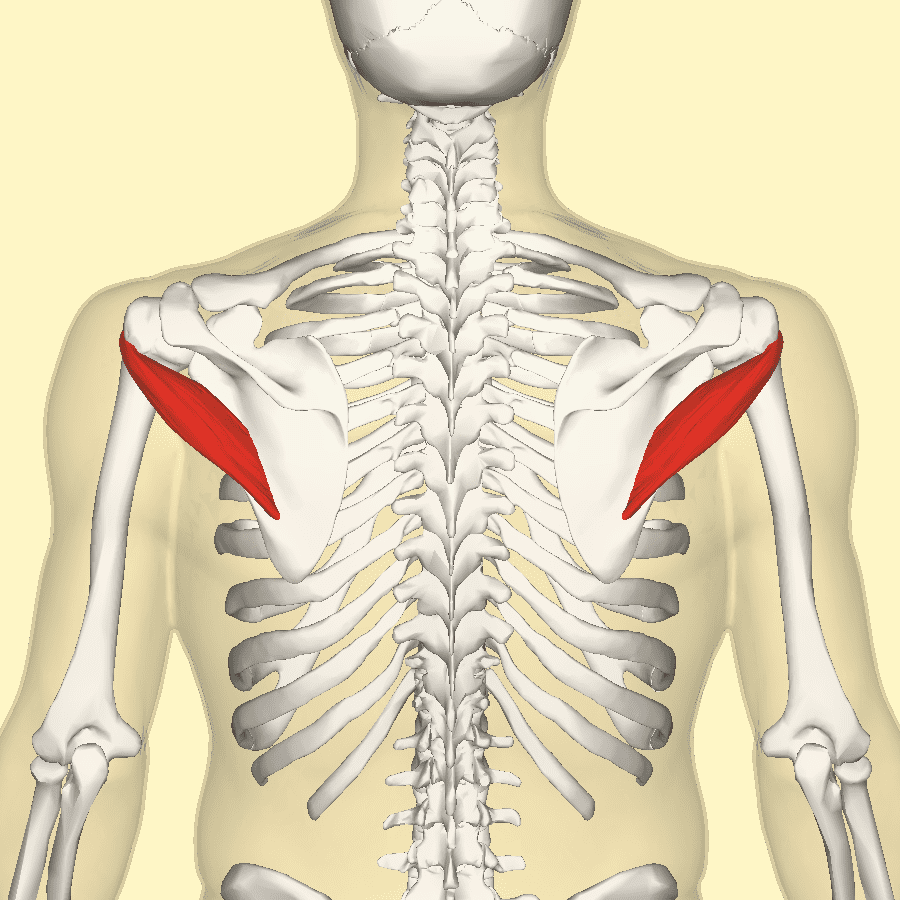
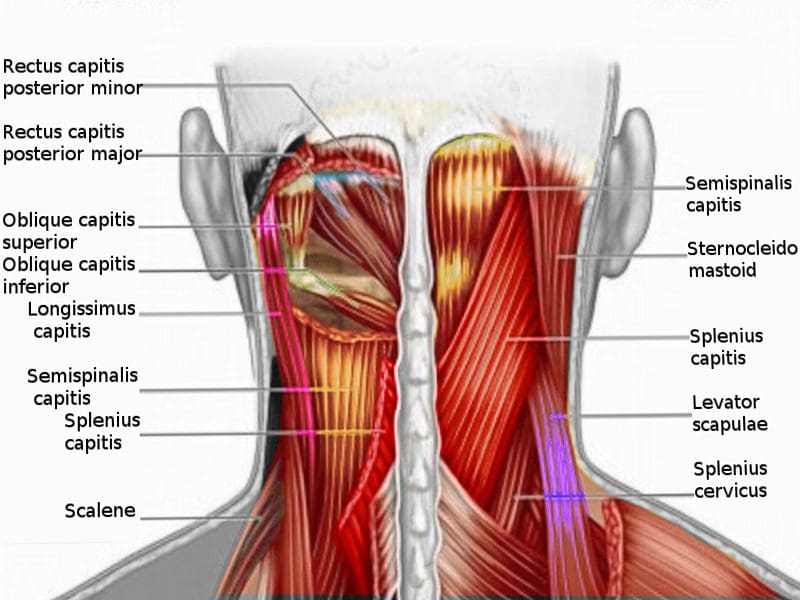
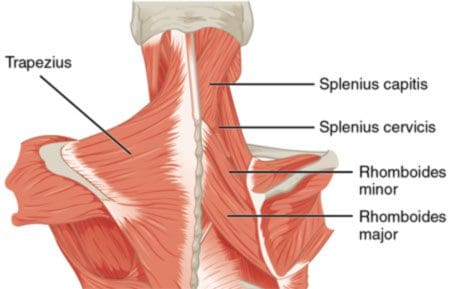
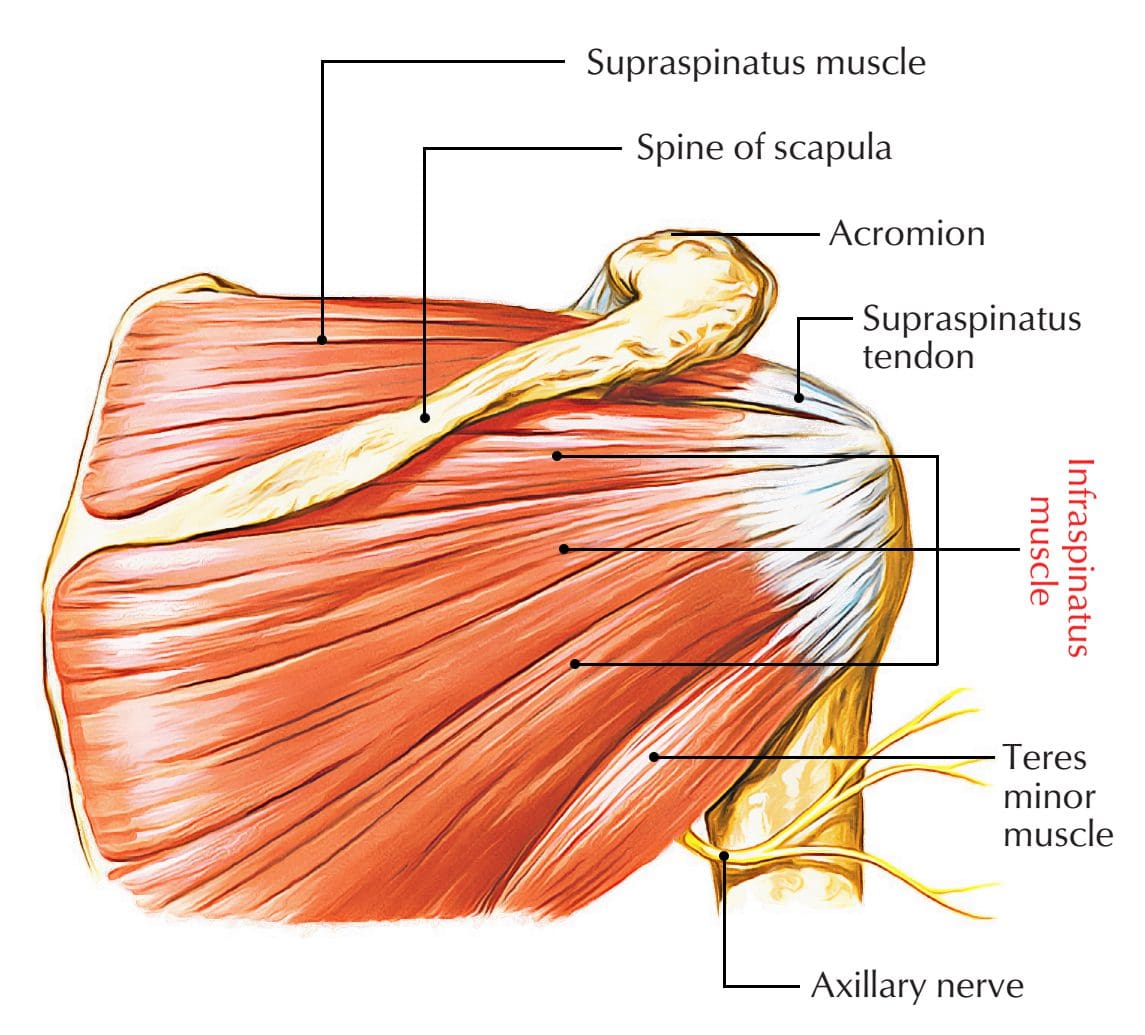
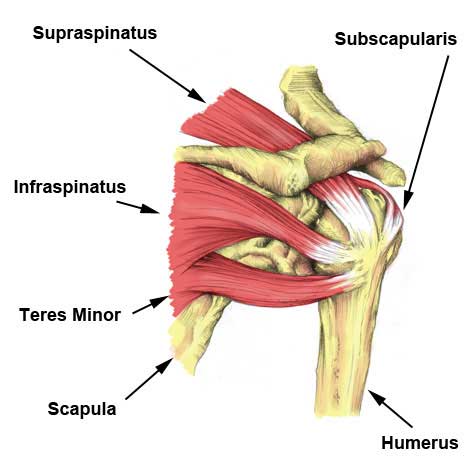
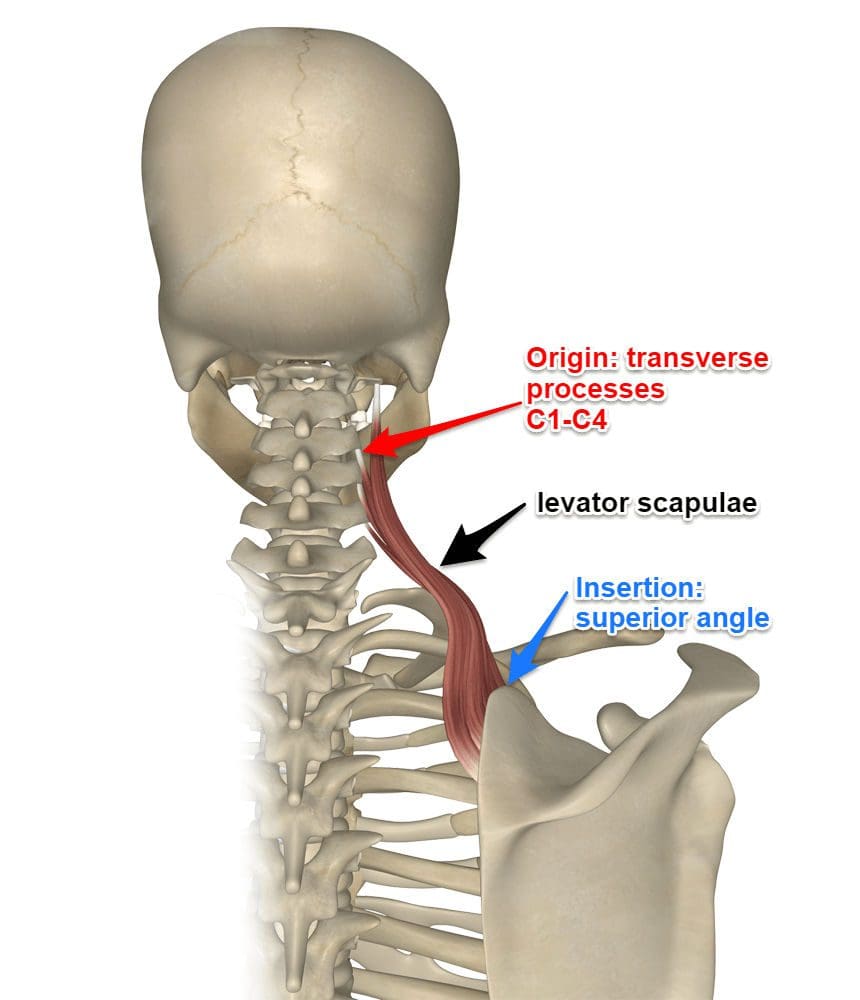
Have you been experiencing shoulder pain? Do you feel a tingling sensation that runs down to your fingertips? What about spasms or stiffness in your shoulders? Most of these symptoms are caused by trigger points associated with shoulder pain along the teres minor muscles. The teres minor muscles are part of the muscle group that supports the rotator cuffs. These muscles include the subscapularis, teres minor, supraspinatus, and infraspinatus and together assist in stabilizing the shoulder joint and even help perform arm movement. For the teres minor, this muscle is a narrow intrinsic shoulder muscle that extends from the lateral border of the scapula (shoulder blade). The teres minor is deep to the deltoid muscle as it has functions parallel to the other rotator cuff muscles, especially the infraspinatus. Studies reveal that even though the teres minor is often overlooked in normal shoulder function. To that point, the teres minor muscle becomes a key component for maintaining shoulder function when the other rotator cuff tendons fail from pathology that affects the shoulder and the rotator cuff joint.
How Do Trigger Points Affect The Teres Minor Muscle?
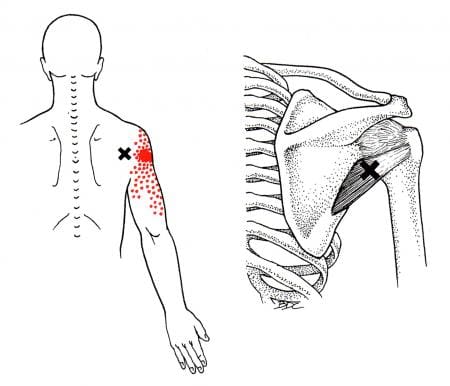
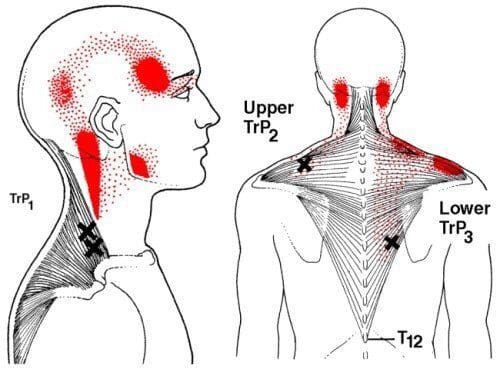
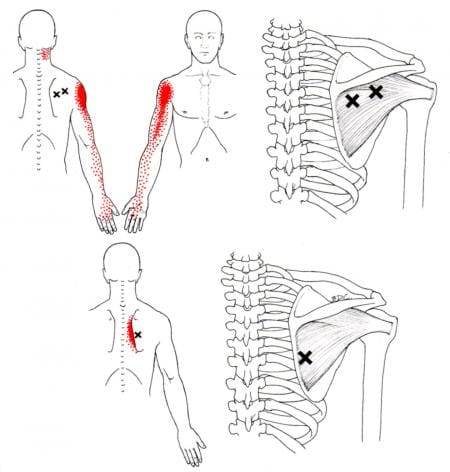
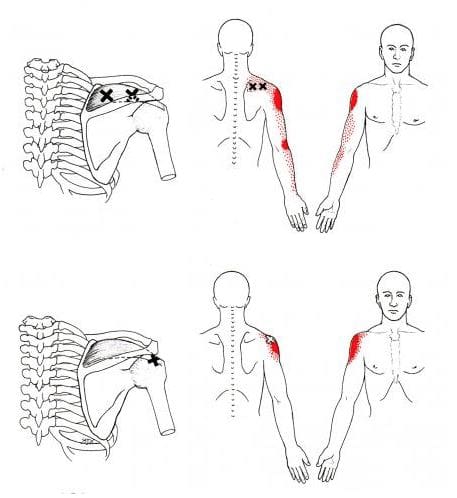
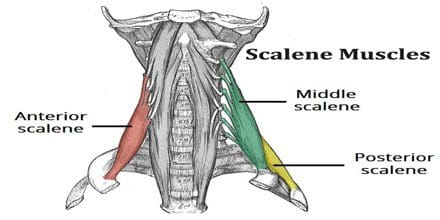
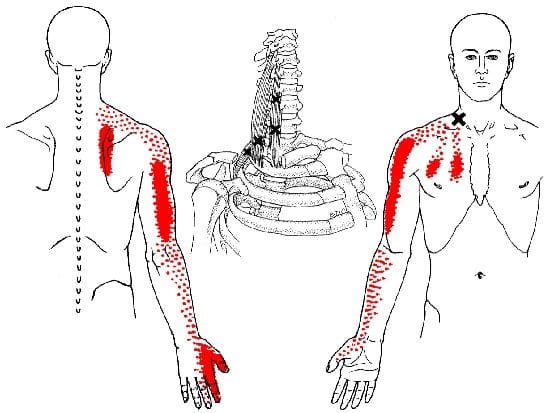
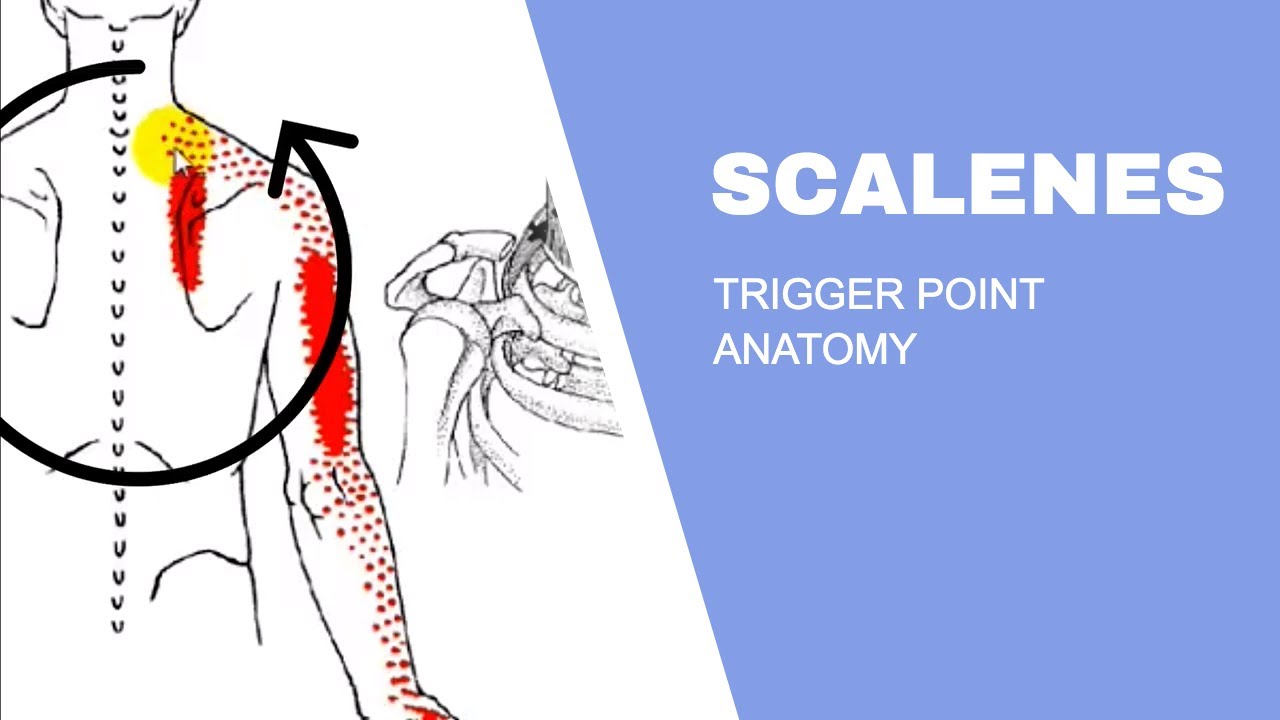
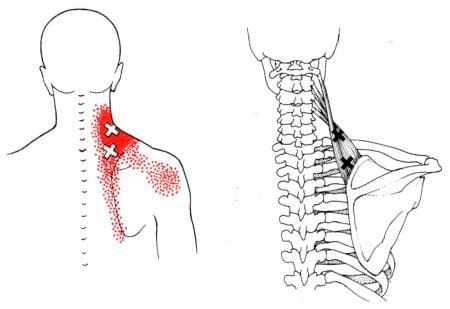
When pathology begins to affect the body, it affects the shoulders and the rotator cuffs. When pain affects the rotator cuffs, trigger points can develop and cause associated pain-like symptoms along the shoulders. Shoulder pain is the third common disorder in the musculoskeletal system. When the corresponding muscles in the shoulder are affected, trigger points can mimic other conditions that make it difficult to diagnose. According to Dr. Janet G. Travell, M.D., many patients often complain more of the pain rather than the restricted motion of their shoulders. This is due to the infraspinatus muscle being affected by active trigger points, causing referred shoulder pain. To that point, infraspinatus-referred pain dominates and releases tension to the parallel muscle fibers, the teres minor. Other issues like hypertrophy can also affect the teres minor when there are rotator cuff tears. Studies reveal that when the rotator cuff suffers damage and begins to tear, it could potentially lead to teres minor hypertrophy and cause referred pain-like symptoms along the upper arm. Fortunately, there are ways to manage trigger points associated with the teres minor to alleviate the pain.
Treating Myofascial Teres Minor Pain- Video

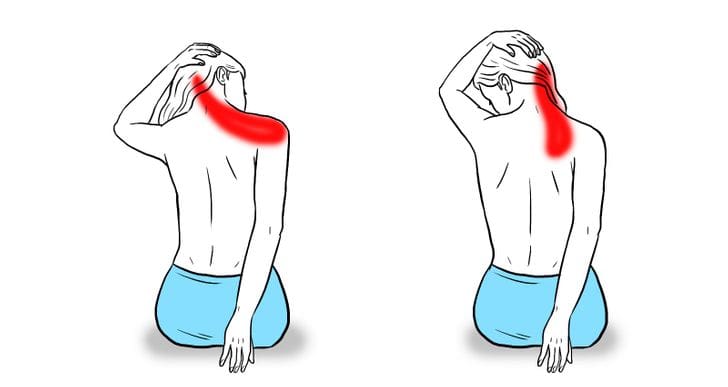
Feeling aches and pain when you are rotating or lifting your shoulders? What about feeling pain in your upper arm? Or do you feel tenderness on your shoulders or upper arm? Many people experiencing pain along their shoulders might be due to trigger points affecting the teres minor muscle. The teres minor muscle is part of the rotator cuff and helps stabilize the shoulders to prevent instability. When factors cause dysfunction in the rotator cuff can lead to the development of trigger points associated with the teres minor muscle, causing overlapping referred pain to the shoulders. Studies reveal that individuals who overuse their shoulder muscles can make them hypersensitive to mechanical pain. To that point, this allows active trigger points to play a role in the development of shoulder pain along the teres minor muscle. The video above shows where the teres minor muscle is located and how to release the trigger points from the muscle to reduce pain in the shoulders and the upper arms while preventing disability.
Managing Trigger Points Associated With The Teres Minor Muscle

When many individuals suffer from shoulder pain associated with trigger points, they often explain and show their primary doctor where the pain is. Their doctors then examine their patients to pinpoint where the issue is before diagnosing the symptoms that are affecting them. Once the symptom is diagnosed as trigger points associated with shoulder pain, doctors would refer their patients to pain specialists like chiropractors or massage therapists to manage and reduce trigger points affecting their shoulders. Many pain specialists will use various techniques to relieve shoulder pain associated with trigger points. Studies reveal that the effects of dry needling on active trigger points in the teres muscle are effective for improving pain intensity, inter rotation range of motion, and extensibility on the shoulder. Other ways to manage trigger points associated with the teres minor muscle include:
- Reducing or avoiding excessive or repetitive load on the muscle
- Have a correct sleeping position to prevent shortening the shoulder muscles
- Applying a hot compress on the muscle to relax the stiff muscle and reduce trigger points from forming further
- Doing stretching exercises to relieve shoulder tension
Incorporating these can help restore shoulder mobility and prevent future trigger points from forming and causing shoulder pain.
Conclusion
The teres minor is part of a muscle group that supports the rotator cuffs in the shoulder. These muscles stabilize the shoulder joint and help perform arm movement. The teres minor is a narrow muscle extending the scapula’s lateral border (shoulder blade). When pathologies begin to affect the muscles in the shoulder area, it can lead to the development of trigger points along the teres minor muscle and cause referred pain along the shoulders and upper arms. To that point, many individuals will regain their range of motion in their shoulders without pain. Various treatments can help reduce the effects of referred pain along the shoulders and manage trigger point pain associated with the teres minor muscles.
References
Ceballos-Laita, Luis, et al. “Effects of Dry Needling in Teres Major Muscle in Elite Handball Athletes. A Randomised Controlled Trial.” Journal of Clinical Medicine, MDPI, 20 Sept. 2021, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8466529/.
Juneja, Pallavi, and John B Hubbard. “Anatomy, Shoulder and Upper Limb, Arm Teres Minor Muscle.” In: StatPearls [Internet]. Treasure Island (FL), StatPearls Publishing, 15 May 2022, https://www.ncbi.nlm.nih.gov/books/NBK513324/.
Ortega-Santiago, Ricardo, et al. “Pressure Pain Hypersensitivity and Referred Pain from Muscle Trigger Points in Elite Male Wheelchair Basketball Players.” Brazilian Journal of Physical Therapy, Associação Brasileira De Pesquisa e Pós-Graduação Em Fisioterapia, 2020, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7351965/.
Tokish, John M., et al. “Teres Minor Hypertrophy Is a Common and Negative Predictor of Outcomes after Rotator Cuff Repair.” Orthopaedic Journal of Sports Medicine, SAGE Publications, 29 July 2016, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4968368/.
Williams, Matthew D, et al. “Understanding the Importance of the Teres Minor for Shoulder Function: Functional Anatomy and Pathology.” The Journal of the American Academy of Orthopaedic Surgeons, U.S. National Library of Medicine, 1 Mar. 2018, https://pubmed.ncbi.nlm.nih.gov/29473831/.








 Chiropractic Education
Chiropractic Education










 Health Benefits
Health Benefits