Dr. Alex Jimenez, D.C., presents how to assess different hormones in the body and how different hormone tests can be used to determine the level in the body. This presentation allows many individuals to know what to expect when they are being diagnosed by their primary doctors. We refer patients to certified providers incorporating various hormone therapies to ensure optimal health and wellness. We encourage and appreciate each patient by referring them to associated medical providers based on their diagnosis when it is appropriate. We understand that education is an excellent way when asking our providers intricated questions at the patient’s request and understanding. Dr. Alex Jimenez, D.C., only utilizes this information as an educational service. Disclaimer
Assessing Hormones
Dr. Alex Jimenez, D.C., presents: Welcome to everything you need to know about assessing hormones and how to do the testing. We have decided to do this as a webinar because we only have a little time to do it during the module. After all, that’ll make your life easier. You’ll need to have this information under your belt because here is the most important thing you need to know. Hormone therapy is an art, not a science. If you find five or six practitioners who do hormone therapy, you will find five or six different ways to make a prescription and way more ways than that actually to do testing to monitor it.
Dr. Alex Jimenez, D.C., presents: The important thing is that you keep in mind what we know scientifically is a better or not-so-good way of taking care of the patients in terms of testing. Then find what works for you and become the expert in that. Because if you are consistent over time, you can work around the pros and cons of every given testing modality and figure out what you need to do, regardless of what type of test you end up doing. All right, so what do we need to worry about? There are many potential problems in measuring hormone levels because so many hormone levels fluctuate significantly. In order to evaluate hormones in the body, doctors need to know what, when, and who to test. So we’re going to talk about all of that.
Diagnosing Hormones In A Patient
Dr. Alex Jimenez, D.C., presents: Some vary during the day, some vary during a cycle, and some hormones don’t vary at all. So you need to remember which ones you need to worry about in terms of fluctuation. The studies that have been done don’t measure hormone levels. So, finding normal hormone levels is sometimes problematic. It may be different from what the labs currently use. And in the studies where they have come up with normal hormone levels, a lot of them are much older studies, and the methodology was more unreliable than what we use now. So by keeping that in mind regarding what people call normal hormone levels, many of these studies also would average out non-comparable groups. What this means is that they would be comparing, let’s say, a group of apples, oranges, and grapes and put them all together and say, oh yeah, so this average is going to work.
Dr. Alex Jimenez, D.C., presents: So it’s like doing a meta-analysis, and if you are taking a bunch of different data, you can’t necessarily say that this average makes sense. You probably are already aware of the fact that other labs end up developing different reference ranges. And so if you use multiple different labs, you can’t necessarily compare the test results you’re getting because the reference ranges are different. And, sometimes, even within a given lab, depending on which test kit patients use, like a test from Quest, they may one day use one test kit. So a reference range will be XYZ, and they went to the same lab another day, but they used a different test kit and have an entirely different reference range. And so you have to the point that out to the patients. If you’ve got a smart patient trying to track what’s happening with themselves, they may have the wrong impression during an examination.
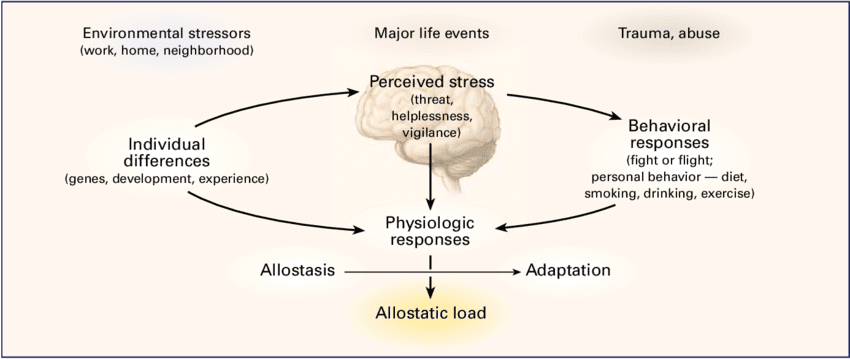
Estrogen & Progesterone
Dr. Alex Jimenez, D.C., presents: If you’ve got different reference ranges showing up on your test results, it is best to keep track of that in case you need to remember. Now there are big variations between individuals and even within the same individual. The serum concentrations of both natural and synthetic steroids might need to be clarified between other individuals. There’s a huge variation irrespective of the root of the administration of the hormones. What you expect from one person may be different from the next person. And, of course, within any individual, you’re going to get levels of fluctuation throughout the day based on lots of different things. Everything from perceived or actual stress that will change their hormone levels to foods they were eating that day can make a difference. Hydration status can make a difference. So some of the variations you see within a person, but with different blood draws, can be based on what was going on that day.
Dr. Alex Jimenez, D.C., presents: So try to impress upon your patients as you’re getting testing done to keep the blood draw days the same. Now measuring in different body fluids like serum, urine, or saliva doesn’t necessarily tell us about concentration in other tissues, and doctors need to keep this in mind because the patient may get a false sense of security, and it won’t necessarily have anything to do with the tissue they are trying to treat. Now, many doctors must remember all the different kinds of estrogens they might need to keep track of during examination. So, when they notice estrogen, there’s an estrogen pool. There is free and bound estrogen in the body and estrogen production in the woman or a man in themselves. There are exogenous estrogens that you may be giving them. There are stored estrogens, metabolites, and all these different estrogens doctors need to keep track of. So this is just one example of having many estrogen levels in the body, and the patient is wondering, what is it the doctor is looking at? Could one test give me all this different information? And this is only estrogen. The same thing is true, although not quite as complicated. The same thing is true about the other hormones in the body.
Dr. Alex Jimenez, D.C., presents: Now for progesterone, it is the same ordeal. Other results look like this for estrogens and testosterone, and this is to remind us of all the different variability there is. By showing the variation between different people at their biological stages, for example, premenopausal and postmenopausal. The results that the doctor presents to the patient establish a lighter shade of green on the outside of the intercycle variability from within a given woman. And then the yellowy green is the inter-woman variability, meaning one woman to the next. And then that blue line in the middle is the average; this provides what information they might need to diagnose.
Testing Hormone Levels
Dr. Alex Jimenez, D.C., presents: All right, so let’s look at testing and assessing hormones as we look at all the hormone types, the different ways of testing them, and the pros and cons. There are decades of well-validated research on serum hormone levels. So for the estrogens, estrone, estradiol, and estriol, as well as the estrogen metabolites in the serum, the good news is it measures endogenous hormone production. So if you get a serum hormone level, we know what those results mean.
Dr. Alex Jimenez, D.C., presents: The bad news is these results give you the free and bound hormone. It shows you the total estrogens. However, you can’t order total estradiol and free estradiol test as they don’t offer them. There are limited data regarding serum levels of these metabolites in terms of prediction for health risk. And it can be difficult for some labs to get accurate quantification in postmenopausal women because the estrogen levels are very low. So, keeping that in mind is a matter of knowing your lab and how accurate they are. Now when it comes to saliva, the good news is it’s non-invasive. Patients can do this at home, making it convenient if doctors try to do a serial measurement of estradiols across a whole cycle in a premenopausal woman. Cause no one in the right mind will go to the lab and get blood drawn daily.
Dr. Alex Jimenez, D.C., presents: Knowing that salivary estradiol correlates well to free estradiol in serum allows doctors to see what’s in the saliva and what they want to see in the serum. The bad news about saliva is that there are fewer validation studies than serum. There are still quite a few, so it’s a valid testing method. It’s just that it’s not as well validated as a serum because it still needs to be done. Again, it can be very challenging for some labs because the estrogen levels in the saliva are much lower than in the serum. So doctors must ensure the lab is doing a good enough job assessing these very low levels. All saliva testing can be contaminated by blood from the oral mucosa.
Saliva Testing
Dr. Alex Jimenez, D.C., presents: So if the patient has periodontitis or something along those lines, doctors don’t want them to salivary levels; it is important to tell them to do it before they brush their teeth, not after, in case they bleed when they brush their teeth. But that’s true of any salivary test; you can’t get estrogen metabolites done through the saliva. And the bigger problem in a postmenopausal woman is that many get dry mouth after menopause. And so, it can be really difficult to do the test because they need to produce more saliva to get an adequate specimen. Now, if that happens, they can go for a 24-urine test. The 24-hour urine testing for estrogen and estrogen metabolites can be helpful if you’re trying to get the total daily production of the hormones. You can get measurements of estrogen metabolites, which are stable for a long time.
Dr. Alex Jimenez, D.C., presents: You have plenty of time for processing and get both free and conjugated estrogen measurements. So that’s helpful. The bad news, which is true for any 24-hour urine test, is it relies on accurate volume measurements and complete collections by the patients. Many patients will inadvertently screw that up. When they have a busy day, they’ll go pee and need to remember what they are supposed to do, which can be a problem. So, making sure the patient understands can help with the test results. You cannot use this for people with renal dysfunction because it’s based on creatinine correction. So if their creatinine is abnormal, they will need to be able to give you an adequate, appropriate level and sometimes give you some of these tests that do 24-hour urines will provide you with many metabolites that could be more clinically useful but are not.
Dr. Alex Jimenez, D.C., presents: Now for dried spot, you’re in testing, and you can get estrogen metabolites, which is good because the metabolites are stable for a long time, so that’s no problem. And you can measure both the free and conjugated estrogens on these spots in urine tests. The biggest problem here is that it has the least clinical validation studies. So, it’s a newer way of testing. It is popular and easy for patients, but there is little concern because of the few clinical validation studies they’ve done. Now, additional challenges are mentioned: to think about what a lab has to do; the measurements they need to be able to provide can vary enormously because there are very low levels of estrogen in older women, not on hormone replacement therapy.
Dr. Alex Jimenez, D.C., presents: And then up to measuring these super high doses in women getting ready for IVF. And, you know, the levels can vary by 10,000. Is it reasonable to assume that any test will be accurate for all those circumstances? It is also difficult to assess estrogen levels in women treated with aromatase inhibitors because they will likely have very low estrogen concentrations. So that may not be accurately detected by standardized testing. And then specificity is a problem because we talk about how estradiology focuses mostly on how it gets broken down into estrone and then how the estrones get broken down. But the reality is that estradiols convert it to more than a hundred different metabolites, which may interfere with accurate quantification.
Serum Testing
Dr. Alex Jimenez, D.C., presents: So, labs must keep that in mind and ensure that they’re getting adequate specificity for you. Another interesting tidbit is that exogenous sources of S-trial can lead to falsely elevated estradiol levels. So keep that in mind if you have a funny test result that makes no sense.
Dr. Alex Jimenez, D.C., presents: Progesterone and progesterone metabolites in the serum; there’s lots of literature to support using a progesterone level drawn hopefully on day 21 of a 28-day cycle to confirm ovulation. Progesterone has problems as it differs from estradiol. So it is acceptable to use serum progesterone levels for that, as the reproducibility of serum levels is limited if the serum levels are low. So if what that means is if you were to take a person in the first half of her cycle and draw a progesterone level three days in a row at the very beginning of the process and the progesterone should be low, you may not get similar numbers just because the hormone levels are low.
Dr. Alex Jimenez, D.C., presents: So the reproducibility makes doctors a little crazy, but that’s something they need to keep in mind with the serum. Again, saliva testing is not invasive; it’s convenient if you want to follow an entire cycle in a premenopausal woman. Also, research shows that a salivary level of 17 alpha hydroxyprogesterone is just as acceptable as a serum level for diagnosing congenital adrenal hyperplasia. Now the downside for progesterone’s metabolites salivary levels of progesterone in its metabolites is that you’ve got a rapid fluctuation of progesterone levels in the saliva. So, if you’ve got somebody who doesn’t wanna get their blood drawn and doesn’t mind spitting into a tube, you can use this instead.
Dr. Alex Jimenez, D.C., presents: So you should use more than one test result to make a decision; you may need serial sampling to get a feel for the average. There’s also a problem with cross-reactivity that might interfere with immunoassays and affect the results. And again, the same problem is having much lower progesterone levels in the saliva than in the serum. So for some labs, that can be challenging to get preliminary analysis and the same problem in terms of contamination by blood; however, that’s true of all cellular tests. The 24-hour urine and the spot dry urine testing for progesterone have the same problem because the progesterone metabolites will correlate with symptoms. So they’ve studied, for instance, allopregnanolone in urine. The level of that does connect with the sleep quality in perimenopausal women.
The Different Implications Of Hormone Testing
Dr. Alex Jimenez, D.C., presents: The implication is that if it’s correlating, it’s probably an accurate level; however, progesterone is hard to quantify in urine. And so, they use metabolites for assessment and determine the progesterone level based on the metabolites. That’s great, except there’s no literature describing the clinical utility of progesterone metabolites. So progesterone in the urine is relatively problematic regarding the accuracy and what you are getting. Part of the issue with serum progesterone is that very little of it is available, and non-protein ground, most of it is bound to all and other proteins; it’s the free progesterone that is available to the target tissues and also to saliva. So the progesterone that you’re measuring in the serum is mostly the bound-up progesterone, not what is clinically important.
Dr. Alex Jimenez, D.C., presents: Transdermal progesterone is extremely difficult to measure because anyone gets metabolism by five alpha reductases in the skin. It’s rapidly absorbed by red blood cell membranes and delivered to the tissue. And really, it comes down to that after the patient uses exogenous progesterone cream or gel, they get these crazy high levels of progesterone in the saliva and the capillary beds, but not in the serum. And so there could be a better way to measure what’s happening to the patient. So transdermal progesterone, trying to follow that with any testing is difficult.
Dr. Alex Jimenez, D.C., presents: There are decades of research on serum hormone levels. In serum testing, testosterone, and its metabolites, you can get both a total and a free hormone level test, and you can also get a DHT level, which is helpful. There are established serum ranges for the diagnosis of androgen insufficiency. So serum levels for testosterone are fine in general. It can be difficult to assist the whole serum if the levels are low, like in women and kids and hypogeal men. So, you need to know your lab and its methodology. Suppose you’re assessing testosterone in women, hypogeal men, or kids because they must ensure they’re doing the appropriate serum test to get these really low levels accurately.
Dr. Alex Jimenez, D.C., presents: For saliva testing, it is very convenient to obtain the sample. There are established ranges for diagnosis of antigen insufficiency, and it’s easy to use this testing for differentiating between gonadal and hypogonadal men. And you can get a free hormone level as lots of published research on using salivary levels for assessing testosterone. However, the problem is like with progesterone; you get this rapid fluctuation in saliva. You might need more than one saliva test result to get reliable information. So you don’t necessarily want to decide based on just one result. And again, you need to know your lab because the levels are much lower than in the serum. So it is challenging to get an accurate story and be careful about blood contamination. In urine testing, the 24-hour and spot urine have slightly different issues.
Dr. Alex Jimenez, D.C., presents: The 24-hour urine testing for testosterone can be used to get a total daily testosterone production. Patients will get a free hormone level and metabolites, which is nice. They can use that information to indirectly assess five alpha-reductase and aromatase activities based on how many different metabolites they’re getting. Only a few data support the clinical utility of all the measured metabolites. There is a polymorphism of UGT to B17; if the patient has that, their urinary testosterone level will return to zero, so keep that in mind if you ever get a test result. After all, it’s so low because it may be that your patient has this issue. Now spot urine will give you some of the same pros as you will get free hormone levels and metabolites. This allows you to use that information to assess the five alpha-reductase aromatase activities; however, the problem is there; like with the other hormones we’ve discussed, this testing generally has fewer clinical validation studies because it’s a newer form of testing, so keep that in mind.
Cortisol
Dr. Alex Jimenez, D.C., presents: Cortisol and its metabolites in the serum are similar to the other hormones mentioned, as there are validated reference ranges for cortisol. Lots of peer review literature detailing the use of this test, and patients can feel comfortable getting these results. It will tell them just total cortisol, not their free cortisol. So by keeping that in mind, they’ll get the diurnal pattern. They can only get a four-point test as they would with saliva because they don’t have normal ranges for four different times in the day. And many patients mention to their doctors as they get the serum cortisol, they go, “Wait, you don’t understand. I am so scared of my blood being drawn that it shoots my cortisol up, and I don’t normally look this bad.”
Dr. Alex Jimenez, D.C., presents: Keep in mind that in serum, they only have normal reference ranges for two times of the day, 7 to 9:00 AM and 3 to 5:00 PM. So you have to ensure that if you use serum cortisol, they go in fasting before nine o’clock, or they can go later in the day. And if they go later in the day, they don’t have to fast. So if you get cortisol at 10 or 11 in the morning, it isn’t very helpful to the results. Now the salivary testing, lots of people are becoming familiar with this.
Dr. Alex Jimenez, D.C., presents: You can get your diurnal pattern because many companies have kits where you’ve got four or five samples throughout the day. There is abundant peer-reviewed literature detailing the use of this. And this is for cortisol, not for the cortisol metabolic. It reflects the unbound plasma concentration, which is not what we’re seeing with the serum. The problem is that 11 beta hydroxy steroid dehydrogenase is an enzyme in the salivary glands that significantly converts cortisol to cortisone. So there are some questions about the results doctors are getting in the salivary cortisol and what’s happening or did it get converted to cortisone, and you’re not picking that up in the test?
Dr. Alex Jimenez, D.C., presents: So when looking at cortisol metabolites in the saliva, which some companies do and some don’t, the salivary cortisone correlates with cortisol exposure over 24 hours. There’s a moderate level of literature using this test but enough that you should feel comfortable. There are issues when your serum cortisol is really low, making it seem like the patient is crashing or under hydrocortisone therapy. That makes the salivary cortisone a superior serum marker compared to the salivary cortisol. Under these circumstances, because of how this is being processed, only a few companies are even looking at cortisone directly in the saliva. So at this point, because especially of the moderate literature level, you will primarily be doing cortisol levels in the saliva.
Urine Testing For Hormones
Dr. Alex Jimenez, D.C., presents: So let’s move on to the urine test. Now, in a 24-hour urine test, you can assess the cortisol ratio, which can be helpful when diagnosing. And 24-hour free cortisol correlates with the serum-free cortisol level; however, the only problem is there are limited clinical validation studies for this. And, in the 24-hour urine test, you’re not getting a diurnal cortisol pattern. And, in the spot urine, you can get the cortisol ratio, which can be helpful. You can have the patient do the spot urine test multiple times a day so you can get the diurnal change just like you would with saliva. But unfortunately, the spot you’re in testing has the least clinical validation studies. So you have to keep that in mind. So with this, primarily, people feel most comfortable with using either serum levels done at the right time of day, understanding that you’re not getting the unbound cortisol, or they’re doing a four-point salivary test.
Dr. Alex Jimenez, D.C., presents: The four-point salivary test could see a pattern between what the patient told their doctors about their energy level throughout the day and how they felt and compared that with what the result returned. Many doctors note what they had expected the test result to be before the national labs even had it available.
DHEA Testing
Dr. Alex Jimenez, D.C., presents: We will discuss DHEA and DHEA sulfates separately since DHEA in the serum has many clinical validation studies that can make you feel comfortable getting adequate results. Now, DHEA has a diurnal pattern. So you have to ensure they get it done at the right time of day since this is fasting before nine o’clock in the morning, just like with cortisol. A DHEA done later in the day means nothing; however, a DHEA sulfate in the serum doesn’t follow a circadian pattern, so a single test done at any time is okay.
Dr. Alex Jimenez, D.C., presents: There are numerous clinical validation studies about DHEA; unfortunately, there is a problem with DHEA sulfate since it has a little circadian pattern. You may miss small variations in a DHEA over time in a person based on how they’re feeling and stressed out. So occasionally, it’s nice to check the DHEA in a patient as long as they’re done in the morning because then you’ll get a feel for the changes over time in the same individual you wouldn’t see with the DHEA sulfate.
Dr. Alex Jimenez, D.C., presents: Salivary testing for DHEA is where you measure free DHEA in the body, which is great. There’s a correlation with serum levels, and it’s not invasive. The problem is that the concentration is inversely related to the salivary flow rate and is also affected by the salivary pH. An example would be someone walking past the bakery, starting to salivate heavily based on what they just smelled. This could change their results for their salivation rate when they are doing their DHEA test. DHEA sulfate has the same basic problem in the saliva, related to the salivary flow rate and the salivary pH. So keep that in mind if you’re looking at salivary levels in urine, whether this is 24-hour or spot urine; there are no clinical validation studies about looking at either DHEA or DHEA sulfate in the urine. So, keep that in mind if you’re doing urine testing and they’re giving you a whole panel that includes DHEA or DHEA sulfate, you may need to know what those results mean.
Dr. Alex Jimenez, D.C., presents: For pituitary hormones, the preferred testing is the FSH, LH, and prolactin serum. Not convenient for serial measurements throughout the day to detect the LH surge, for instance, but the results are very accurate. And in saliva, there’s limited peer-reviewed literature detailing salivary pituitary hormones and whether or not they’re adequate. LH detection kits at home are convenient for urine tests since they are widely used and have been around for a long time. The LH surge correlates with the urine and works well with the LH surge’s serum. So if you’re trying to help people figure out where they are in their cycle and whether or not they’ve ovulated, this test is the way to go. It doesn’t do a good job of quantifying it; it just tells you there’s a surge because these are bigger hormones, so they don’t get into urine very easily.
Dr. Alex Jimenez, D.C., presents: So you’re going to know whether or not you’ve gotten the surge, you’re not going to know what the actual level is, and that’s okay because most of the time, it doesn’t matter what the hormone level is. So essentially, unless you’re just trying to find out if they got an LH surge, you want to use the serum for either FSH, LH, or prolactin. For sex hormone-binding globulin, most clinical validation studies are in the serum; you can’t measure it in saliva or urine, so that’s easy to remember. So we’ve already talked about the issues with different forms of testing, and there are only a few forms of testing that will give you everything you need to know about every hormone you need to know.
When Is The Best Time For Hormones?
Dr. Alex Jimenez, D.C., presents: So now, when is the best time to test hormones? Early morning is when the hormones will be the highest for most hormones. So, the best way to go and test hormone levels like cortisol and gonadal hormones is first thing in the morning since you have to be consistent and fast because what you’ve eaten can change hormone levels. So if you’ve always fasting, at least you’ll find consistency between specimens and the same person. You also need to know where they were in their cycle for certain tests. So, women patients who are still cycling need to record the first day of their next period to know what day you did their testing. Otherwise, they’ll have to use ovulation kits to know exactly where they are.
Dr. Alex Jimenez, D.C., presents: And of course, the downside here is that if you’re trying, for instance, to get a day-21 progesterone, and she typically has a 28-day cycle, so you tell her to go on day 21, but that particular month she has a 35-day cycle, you didn’t get the level that you were looking for. So it can be a little problematic, but remind them to keep track of it so that you won’t be able to look back and know where they were when they had their tests done. So, when do we want these tests in pre and perimenopausal women? Suppose you want progesterone on day 21. You can also do a sex hormone-binding globulin on that day. Menstruating women shoot for as close to day three for estradiol, estrone, FSH, testosterone, or a sex hormone-binding globulin.
Dr. Alex Jimenez, D.C., presents: Now, even though these are ideal, can you get them on other days of their cycle? Yes, but they will have different accuracy. And, of course, it may be an additional day than day three because what if day three happens to land on the weekend and the lab’s not open? So, please consider that what you are looking for here is to test the hormone levels when they’re at their highest. And that’s why we’re shooting for three and 21. So, you know, here’s day three and four. And so the FSH is going to be a nice level here. The estradiol bounces around a lot at this point, so trying to get it in this part of the cycle would be less helpful. And, with progesterone, you’re going to get your peak here, so that’s why you want to try to shoot for 21 days because you know that’s going to be the easiest way to ensure you’re getting it. And also, it’ll help you be more consistent from cycle to cycle if you’re always trying to get it at the same time of the process.
Hormone Replacement Therapy
Dr. Alex Jimenez, D.C., presents: Now here’s where it gets tricky since it’s one thing to find out where the person is before you put them in any hormone replacement therapy; however, monitoring hormone replacement therapy gets more problematic still. If you’re using oral estrogen, it is recommended to get a serum baseline before HRT and then monitor during treatment; if you’re doing oral estrogen, the salivary levels don’t reflect the exogenous estrogen use at all, so they’re not very helpful.
Dr. Alex Jimenez, D.C., presents: And oral estrogen or any hormones that undergo this test must accurately reflect the liver’s first-pass metabolism and the urines’ levels. So if you’re doing oral estrogen replacement therapy, the only way to assess it is with serum because doctors will convince the patient with the module, so you probably don’t want to use oral estrogen anyway. If you’re using sublingual estrogen, the levels will rise and fall rapidly within hours. And so the serum’s not effective in terms of measuring. The saliva will make no sense if you’re doing sublingual because you just had your estrogen there. So what does it mean? It means that 24-hour urine and drive urine testing with sublingual hormones aren’t recommended because there’s always a question of how much you are swallowing and how much is getting absorbed sublingually.
Dr. Alex Jimenez, D.C., presents: Now, if you notice that it says in sublingual, there could be better testing methods. Since you don’t know how much was swallowed and got the first-pass metabolism effect, the result in a 24-hour or dried spot urine may need to be clarified. So that’s problematic. You can still do sublingual estrogen replacement therapy; it just means there’s no great way to test it. If you’re using estrogen creams, serum testing can be effective, and we know that clinical parameters correlate to serum levels when using estrogen creams, so we can do that. In saliva, estradiol and estriol are actively transported into the saliva; the levels are way higher than you would see in the serum and are highly variable. So salivary levels for creams don’t make sense, and there are no good peer-reviewed studies detailing the effective estrogen cream on urinary levels.
Using Hormone Creams & Patches
Dr. Alex Jimenez, D.C., presents: It is probably not a great idea to use urine levels for someone using estrogen creams at the time. If you’re using labial or vaginal estrogen, the serum test appears to be the best choice for monitoring absorption. The salivary levels don’t reflect any dose changes. So basically, it’s probably a waste of time to get a salivary level trying to do urine testing; using vaginal or labial estrogen might be problematic because how do you know you didn’t contaminate the urine specimen. And if you’re using a patch, serum values will rise dose-dependently and then rapidly decline the following removal. It may be helpful, we know that the serum values change based on when you put the patch on and when you take it off, but it is still problematic.
Dr. Alex Jimenez, D.C., presents: There’s no peer-reviewed evidence showing that salivary estrogen can be used to monitor the estrogen patch. And when it comes to the urine testing and the estrogen patch, it does appear that the values in the urine will go up dose-dependently. It may be relatively accurate, but it’s not the best clinically validated test for an estrogen patch. The take-home message here is that no testing is perfect and many of us adjust the dose to the lowest amount, the lowest level we can get, and still have our symptoms controlled. That doesn’t mean they don’t test; you must try to ensure you’re not overdosing on this person. But keep in mind that there are a lot of limitations around what testing can be helpful depending on what form of estrogen replacement you’re using.
Dr. Alex Jimenez, D.C., presents: Now, progesterone and oral progesterone, if you’re using that, the levels rise and fall quickly. You may not be able to catch a serum level that makes sense if you’re taking your progesterone in the evening and then measuring in the morning. Because most women, if they’re taking oral progesterone, will take it in the evening because it helps them sleep. There’s also a problem with the cross-reactivity of metabolites with the immunoassays. So progesterone replacement therapy, if oral, you must take the serum levels with a grain of salt. The same thing with saliva and 24-hour urine testing. We talked about how you’re not getting progesterone; you’re getting progesterone metabolites, so that might be useful. But there’s the problem of how clinically valid the use of progesterone metabolites is. So oral use of progesterone, getting a level, and following it is a little tricky.
Dr. Alex Jimenez, D.C., presents: Now with creams and transdermal progesterone, none of the tests makes any sense because you get mentally increased levels in the serum that don’t rise in any particular way that makes sense. Like all steroid hormones, these are fat-soluble, so if it goes and sits in adipose rather than getting into the bloodstream, it doesn’t necessarily reflect a serum level. Doesn’t necessarily reflect the tissue levels in the uterus and the breast, which is where we care about it. So a serum level for progesterone cream is problematic. Salivary levels after progesterone cream go way up and don’t correspond to symptoms at all. So don’t bother getting salivary level after a progesterone cream. There’s some evidence in urine testing that you can get small increases in the pregnant dial three glucosides if you use progesterone cream. And so it may turn out that we can use that as a measure of what your progesterone is doing.
Dr. Alex Jimenez, D.C., presents: But this still needs some more testing. So it would be best if you remembered that there needs to be a reliable method to track what’s happening when a person uses progesterone cream. So please take your time with getting a level and making a decision based on it. Now, vaginal progesterone suppositories have the same problem. You get minimally increased levels in the serum, which will not give you an adequate result. Progesterone melts or atrocious; you can use serum levels in at troche because you get a more accurate level in the serum than if you had taken it orally. There’s a lack of peer-reviewed research on salivary levels after vaginal progesterone suppositories. And you have to be careful if you’re trying to do urine testing because how do you know you didn’t contaminate the sample?
Dr. Alex Jimenez, D.C., presents: You can’t use a salivary level because you just had the troche or the melt in the person’s mouth. And then, there is at least a potential problem with getting a urine level for a troche or melt because, like a sublingual, how much of this are you swallowing? Individuals may consume some of it and are subject to first-pass metabolism, which means you won’t be able to pick it up in the urine. The larger portion will be absorbed into the capillary blood and probably be accurate in the 24-hour or dry urine test. But that needs to be adequately studied, so keep that in mind if you’re using atrocious or melts. And this is a study that showed that after applying topical progesterone, the saliva and the capillary blood levels were very different compared to those seen in the serum or whole blood.
It’s Important To Do Research
Dr. Alex Jimenez, D.C., presents: So this is just an important research study to remind you of the reliance on serum levels for progesterone. If you’re monitoring, topical dosing can lead to underestimated tissue levels, so you’ll give more than you need. So, be careful about relying on serum levels for topical progesterone because you’re going to overdose people like crazy. And remember, if you overdose on progesterone, it’s high up in the steroid hormone pathway, and you don’t know what this person’s body will do with it; they might turn it into pretty much anything else. Now, testosterone replacement therapy creams or gels can cause blood levels, and the serum level rapidly increases with the application and doesn’t reliably reflect dose changing, any dose changes. So the serum and blood levels are probably not the great way to go. In the saliva, the levels are much higher than the serum and are highly variable since they may give a false indication of overdose.
Dr. Alex Jimenez, D.C., presents: In the urine testing, there’s not good in the 24-hour urine. You probably want to use something other than 24-hour urine. The good news is the dried urine. Now in dried urine, the epitestosterone can be measured if there’s going to be suppression due to exogenous testosterone production if that’s what you think is going on. You can measure the epitestosterone in dry urine testing, which will tell you whether or not, you’ve suppressed this person’s production of testosterone by giving them some. Now, vaginal or labial application of testosterone, there’s no good way to get a blood level that makes sense. The salivary levels, like any other cream or application we might have on your hands, you have to be careful because if you’re handling the specimen vials, to get the saliva, you might get it into the testing medium.
Dr. Alex Jimenez, D.C., presents: And then, just like any vaginal or labial application, if you’re trying to get urine specimens, you have to be careful that you’re not contaminating the urine and getting a falsely elevated level. Blood levels are good if you’re doing testosterone injections, either injection or pellet. Get one-third baseline, and use them for monitoring. It gives you adequate levels. You’ll get a significant elevation in saliva after an IM injection, but there’s wide variability from person to person. So you must take that with a grain of salt regarding how accurate your result might be. The same thing happens in the 24-hour urine specimen. You’re going to get an elevation after an IM injection, but then, there’s a great deal of variability, so who knows how accurate it is?
Dr. Alex Jimenez, D.C., presents: With a salivary level, there’s only some correlation to the bioavailable testosterone. If you’re using a testosterone patch, you can get adequate levels, and there are good studies to show that a blood level will be okay. If you’re using a testosterone patch, the urinary levels, both in 24-hour urine and dry urinary levels, will reflect the increasing doses. You’re getting a reasonably good level with using that. Now, if you’re using DHEA treatment or oral DHEA, you’re going to get a rapid increase in the blood levels right after the oral supplementation as you get with the saliva. You get that also in saliva and also in urine. So you’re picking up on the fact that you took the DHEA test.
Conclusion
Dr. Alex Jimenez, D.C., presents: The problem is variability in the blood, saliva, and urine results. Many don’t particularly appreciate using a lot of oral DHEA anyway because, like all steroid hormones, your body’s going to take it to the liver, and the liver has the opportunity to change it into something else before it even gets into the bloodstream to do its job. Other applications may be more helpful, like transdermal DHEA or topical DHEA; you’ll have to see how the patient feels in terms of symptoms because if you use topical DHEA, the blood levels you’ll get a big rise right after the initial application.
Dr. Alex Jimenez, D.C., presents: So what does that mean because it drops right away? Then, in the saliva after transdermal application of DHEA, the levels will increase, but not linearly. So that doesn’t make any sense. And there is no peer-reviewed research detailing what happens in DHEA levels in the urine after transdermal application. The bigger issue then becomes you might want to keep an eye on what the downstream breakdown products are doing because if you’re not able to get a good DHEA level, you might want at least look at testosterone and estradiol. And that’ll give you some fuel if you’ve overdosed or underdosed on the DHEA. Now, with the vaginal or labial application, the levels in the blood don’t go off at all.
Dr. Alex Jimenez, D.C., presents: There’s no research detailing levels after vaginal application looking at salivary or urinary levels. So you can’t use that as a way of monitoring it. So again, this will be just a matter of following the person and how they feel after using it. You’re not going to need to worry about getting any measurements afterward. It’s simply clinical. The test you choose depends on what you’re giving the person, the form you’re giving it in, and then what you’re trying to find out. By finding a treatment form you like and feel comfortable with, understand whether or not to get testing depending on the structure and replacement you’re using. And then, make sure that you are getting helpful information and not misleading information.


















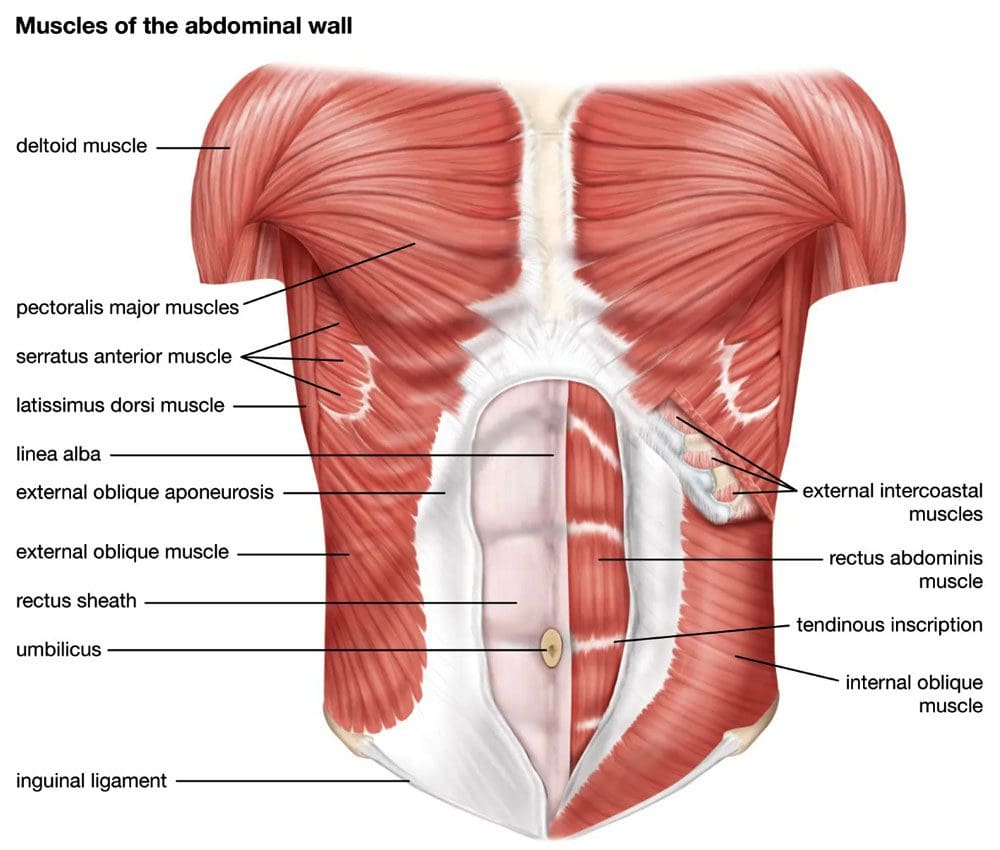 Oblique Muscles
Oblique Muscles