Table of Contents
Introduction
The calves are extremely important to the lower portions of the legs as they allow the individual to move around and help stabilize the entire body. The calves have two muscles: the gastrocnemius and the soleus, which provide plantarflexion and stability at the ankle joint. These two muscles work together to ensure that the upper body’s weight doesn’t lean forward too much to let the individual fall. However, when many people overuse the calf muscles constantly, it can cause the muscle fibers in the lower legs to be overstretched and develop small nodules known as trigger points to cause referred pain to the calves and the ankles that can affect a person’s ability to walk, run, or jump. Today’s article looks at the soleus muscle, how trigger points affect the muscle, and different methods to reduce pain while managing trigger points along the calves. We refer patients to certified providers that incorporate various techniques in the lower body extremities, like lower leg and calve pain therapies correlating to trigger points, to aid many people dealing with pain symptoms along the soleus muscles, causing muscle cramps and issues along the ankles. We encourage and appreciate each patient by referring them to associated medical providers based on their diagnosis when it is appropriate. We understand that education is an excellent way when asking our providers intricated questions at the patient’s request and understanding. Dr. Alex Jimenez, D.C., only utilizes this information as an educational service. Disclaimer
What Is The Soleus Muscle?
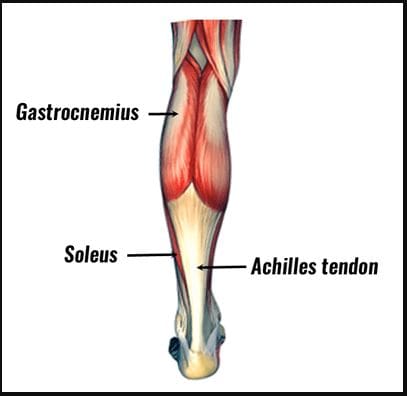
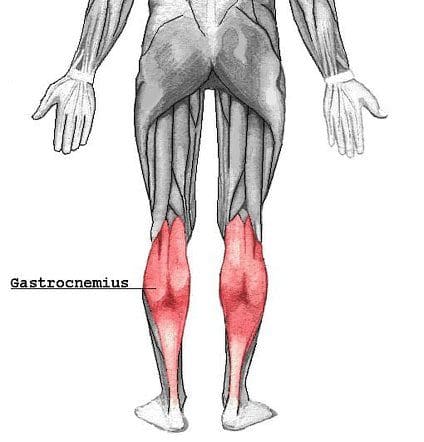
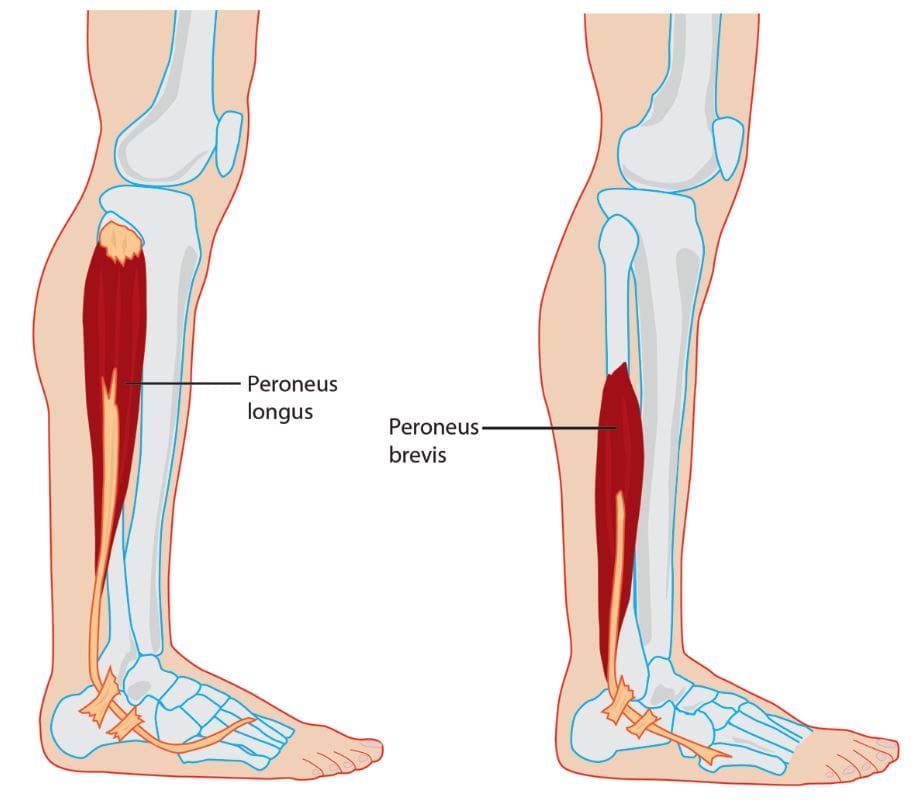
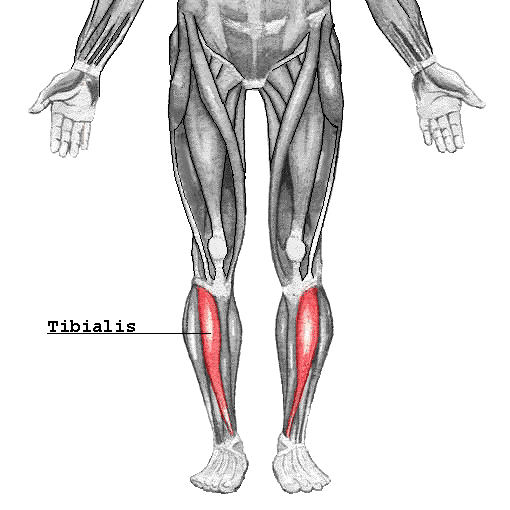
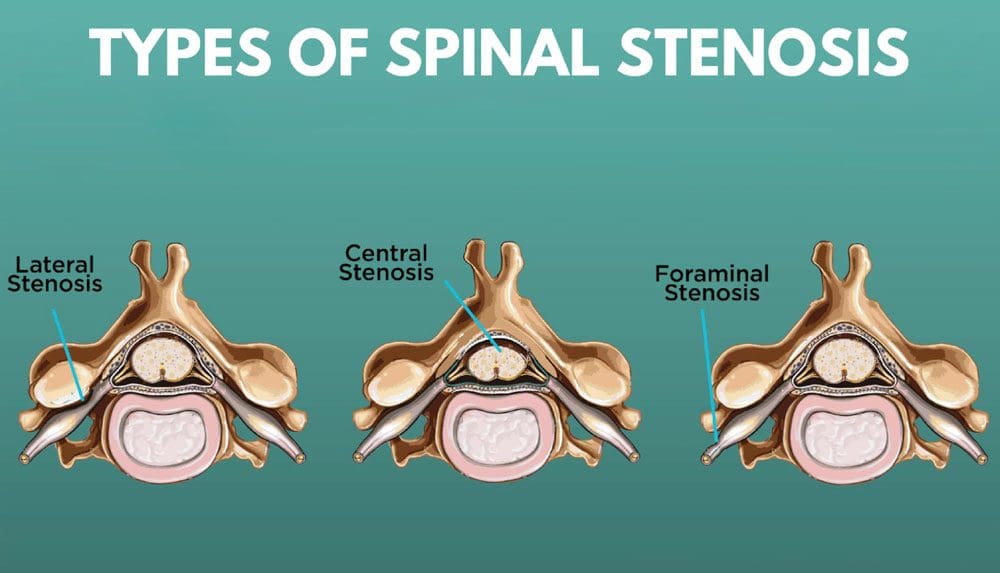
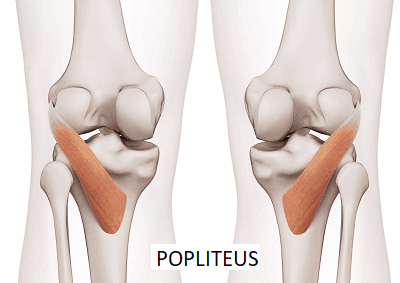
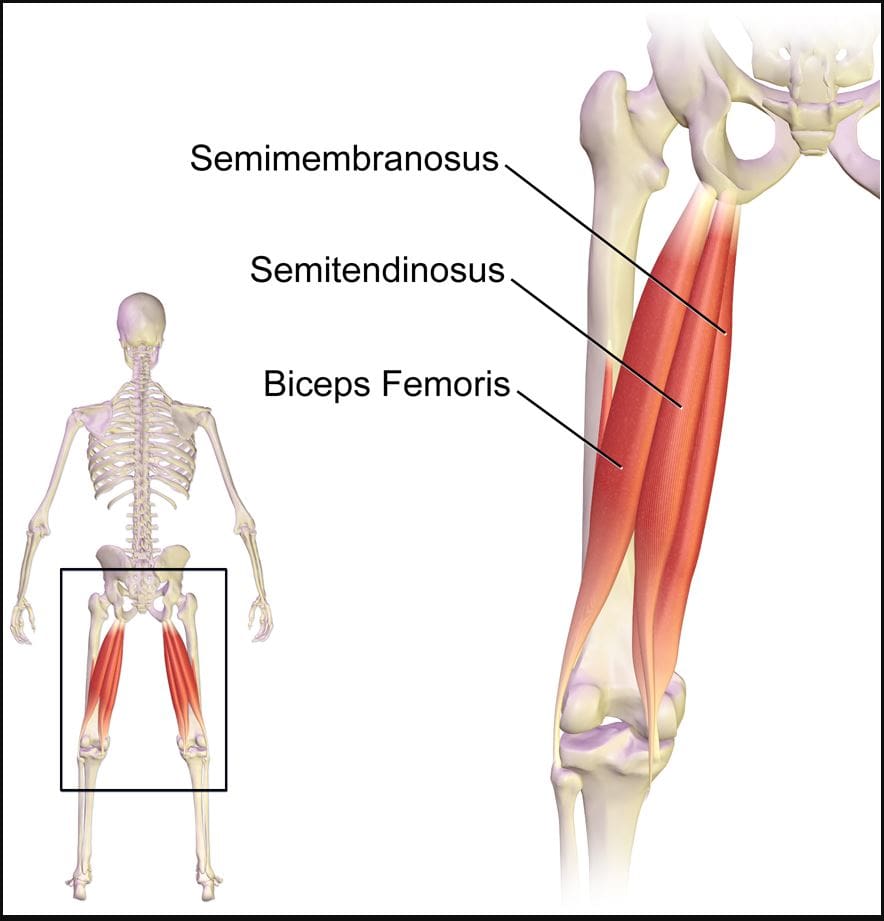
Do you feel a cramping sensation in your calves? Do your feet hurt when you are walking, jumping, or running? Or are you experiencing tightness in your calve muscles? When a person is experiencing calf pain in their legs, it could be trigger points causing overlapping issues in the soleus muscles. As stated earlier, the calves have two muscles: the gastrocnemius and the soleus. The gastrocnemius makes up the round shape of the calves and is a complex, superficial muscle. At the same time, the soleus is a large, flat muscle deep within the gastrocnemius and forms the calcaneal tendon (Achilles tendon), which can be mistaken as a nerve for the ankle. Studies reveal that the soleus muscle works together with the gastrocnemius, and these muscles constitute a plantar flexor. The soleus is part of a group of muscles known as antigravity muscles. It acts like a skeletal muscle and helps maintain good posture in the body to prevent the sheer body weight from falling forwards at the ankle when standing.
How Do Trigger Points Affect The Soleus Muscle?
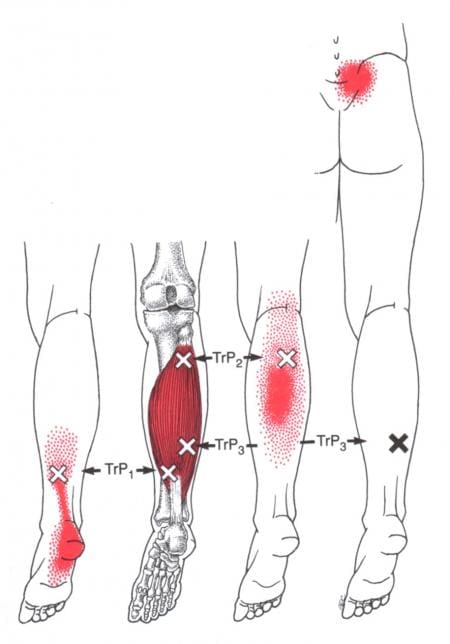
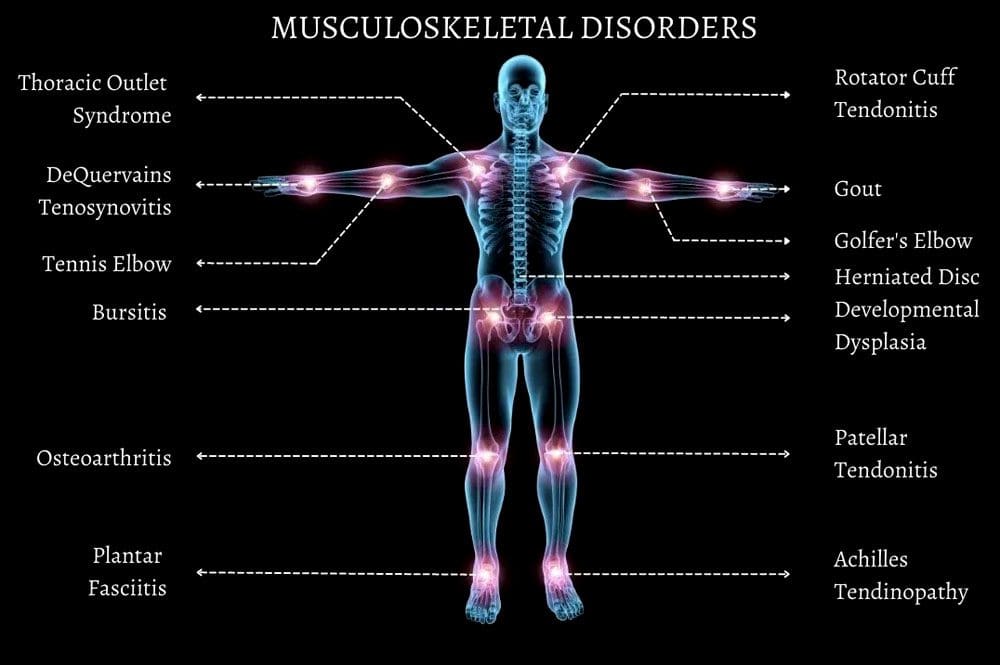
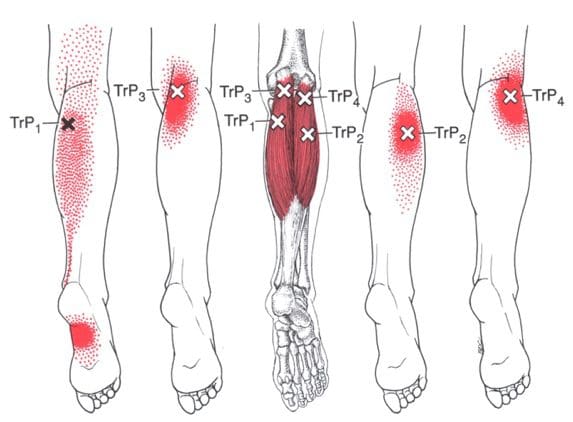
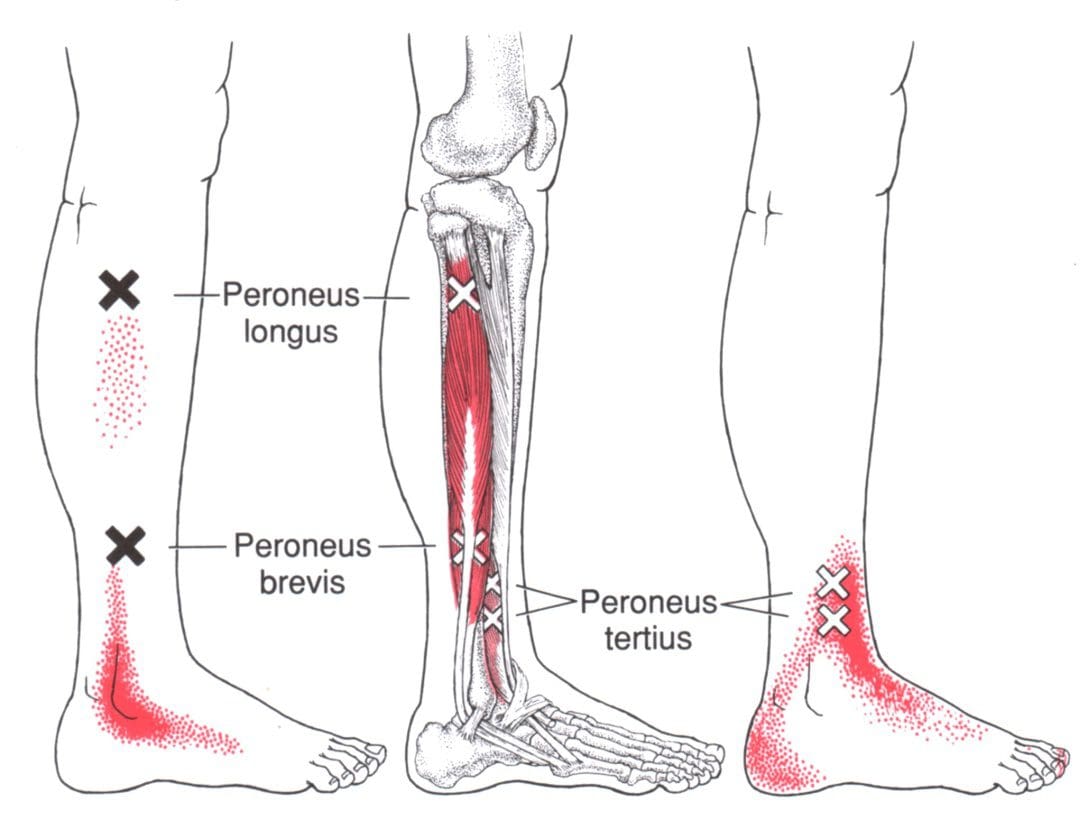
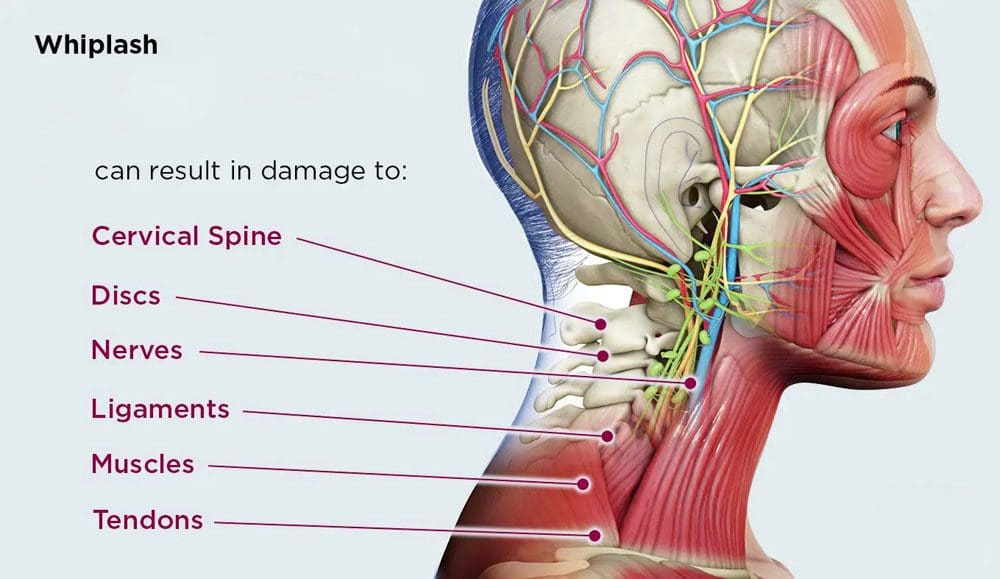
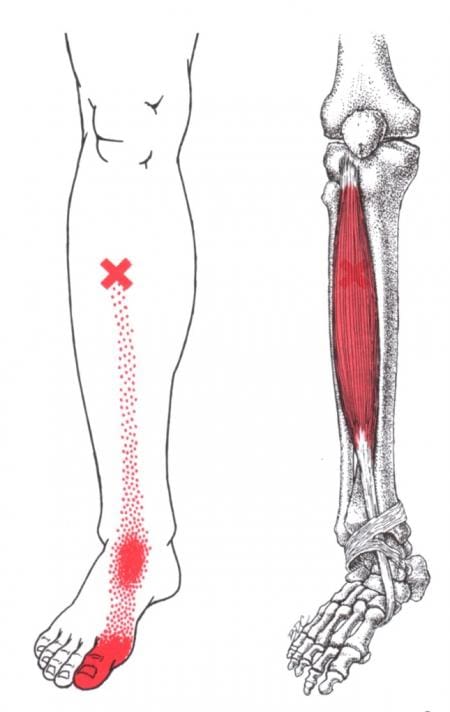
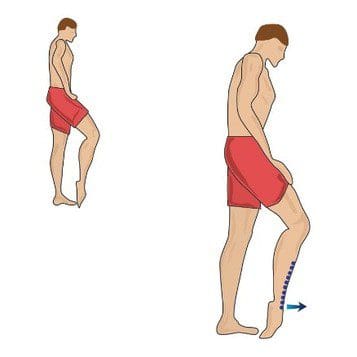
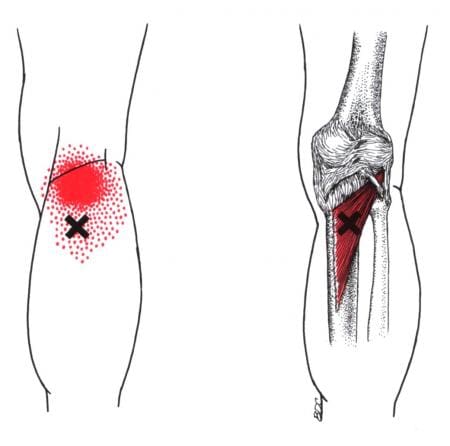
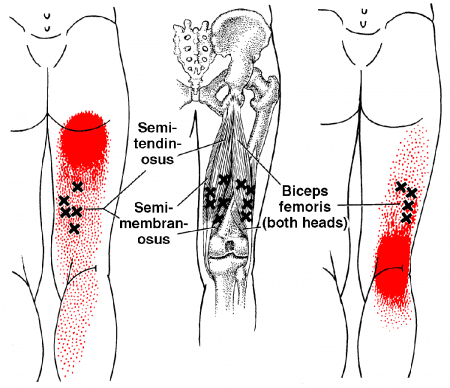
The calves are essential for the movement and mobility functions of the body. When the calve muscles have been overused to repetitive movements or have been dealing with trauma, it can cause the muscle fibers to tear and develop trigger points along the calves causing referred pain to travel down the ankles. Trigger points along the soleus muscle are tricky to diagnose since they cause referred pain to the surrounding muscles. “Myofascial Pain and Dysfunction,” written by Dr. Janet G. Travell, M.D., mention that, unlike the latent trigger points that can affect the gastrocnemius, active trigger points can affect the soleus muscle and cause tenderness referred to the heel. When muscle tenderness affects the heels, it can cause trigger points to mimic chronic conditions like plantar fasciitis. Additional studies reveal that musculoskeletal impairments like trigger points in the soleus muscle could potentially lead to biomechanical changes in the ankle. When trigger points cause hypersensitivity spots in the skeletal muscle taut band, it can restrict the soleus muscle to allow ankle dorsiflexion. Individuals with active soleus trigger points are prone to develop low back pain due to ankle dorsiflexion restriction, leading to them leaning over and lifting objects improperly.
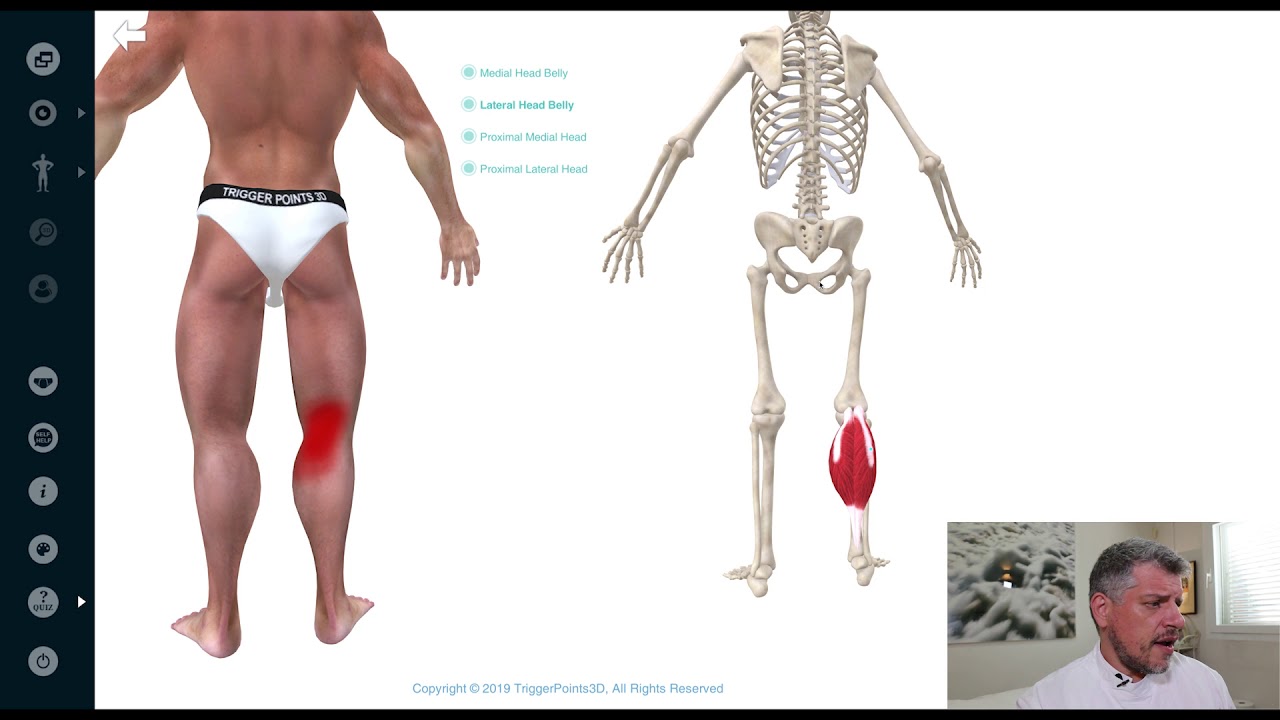
Trigger Point Of The Week: Soleus – Video

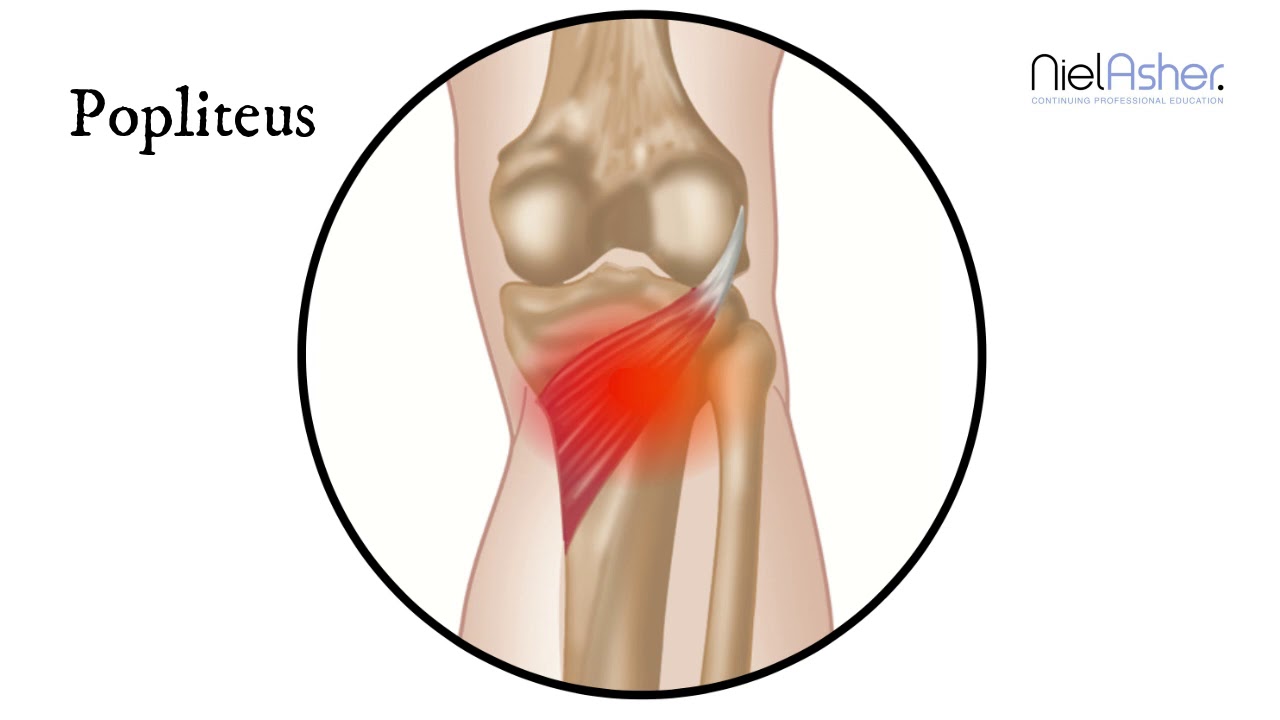
Have you been dealing with pain traveling down from your calves to your ankles? Experiencing stiffness around your ankles? Or do you feel like you are about to fall? These pain-like issues are associated with trigger points along the soleus muscles along the calves. The soleus is one of the two muscles (the other is the gastrocnemius) that make up the calves and acts as a skeletal muscle to help maintain good posture in the body. When trigger points affect the soleus muscle, they can cause referred pain to the calves and mimic chronic issues like plantar fasciitis at the ankles. The video above explains where the soleus muscles are located, deep within the gastrocnemius, where the trigger points are causing referred pain to the ankles, and where they are in the soleus muscle fibers in the calves. Even though trigger points can cause referred pain in the affected muscle fibers of the body, they are treatable and can be managed through different methods to help the calves.
Different Methods To Reduce Pain And Manage Trigger Points In The Calves
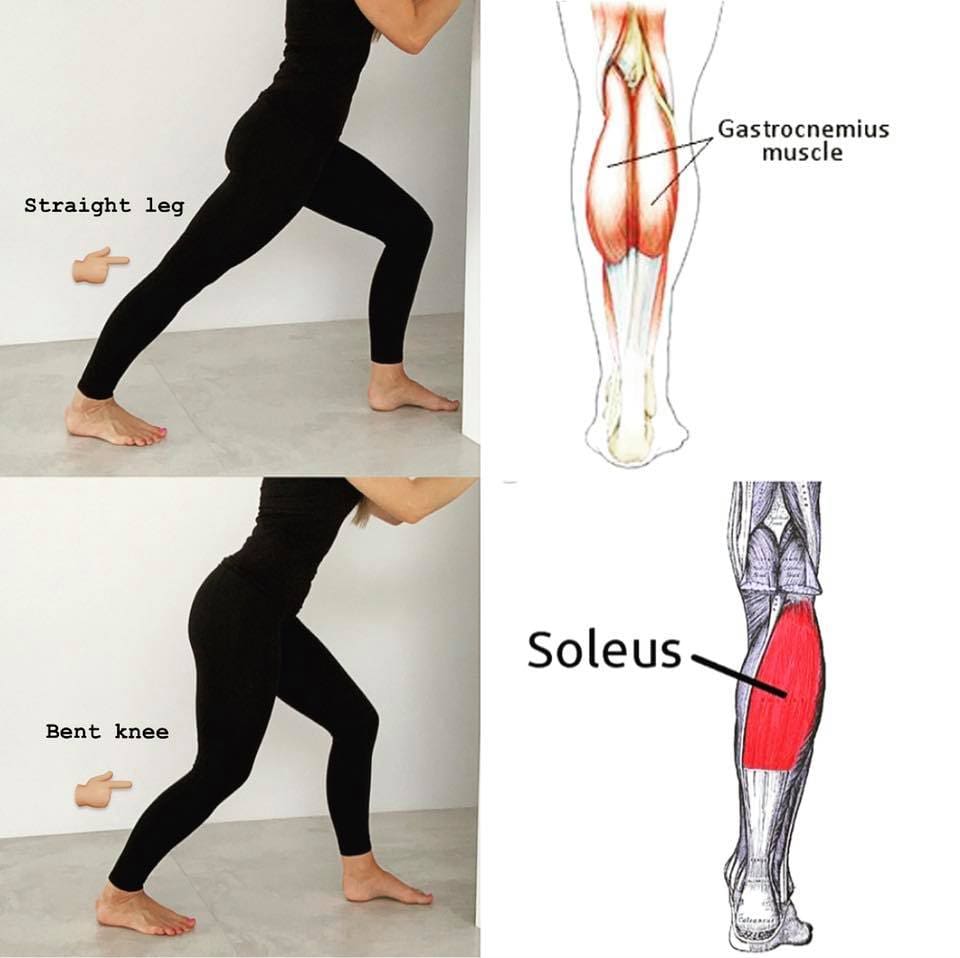
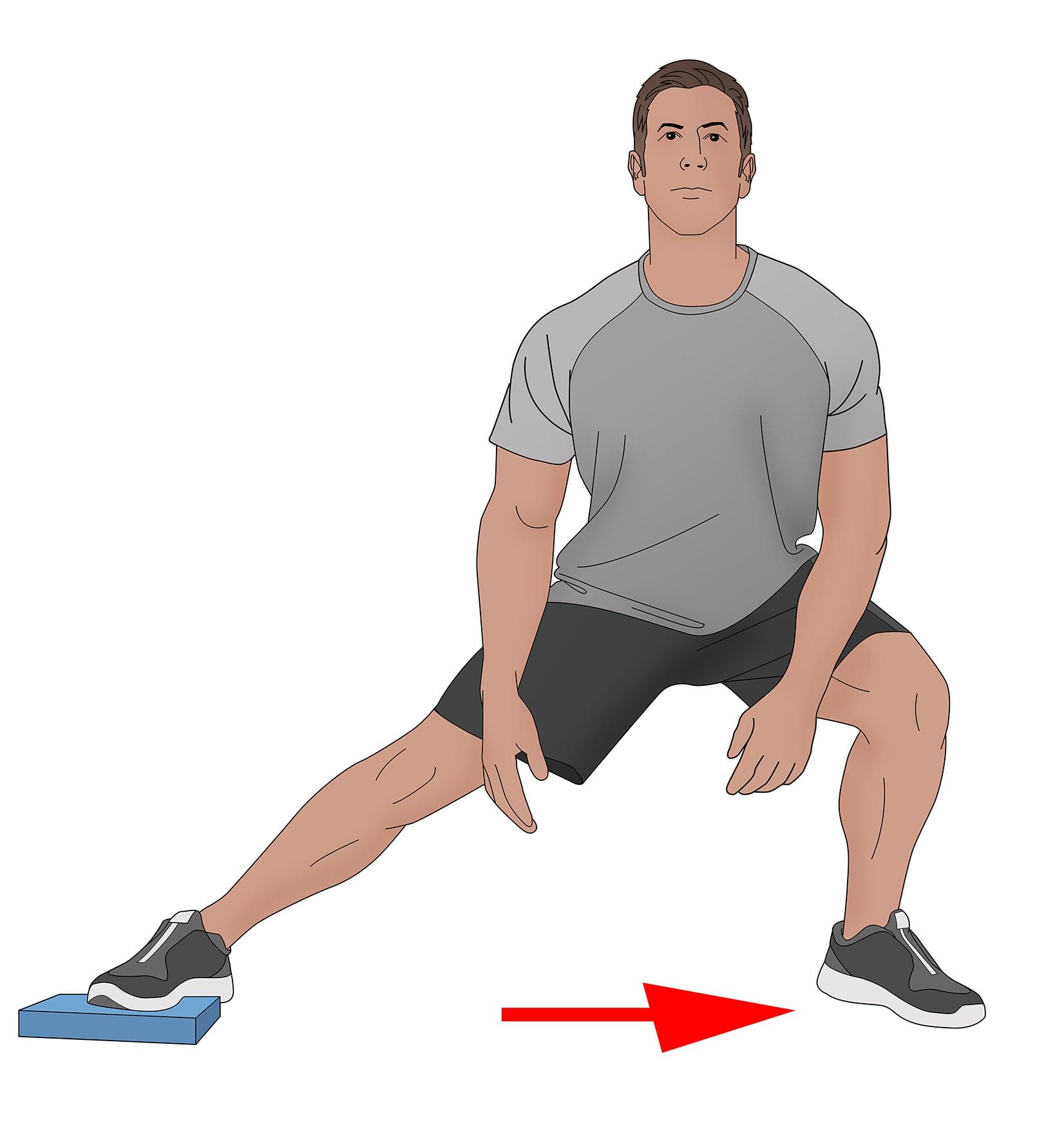
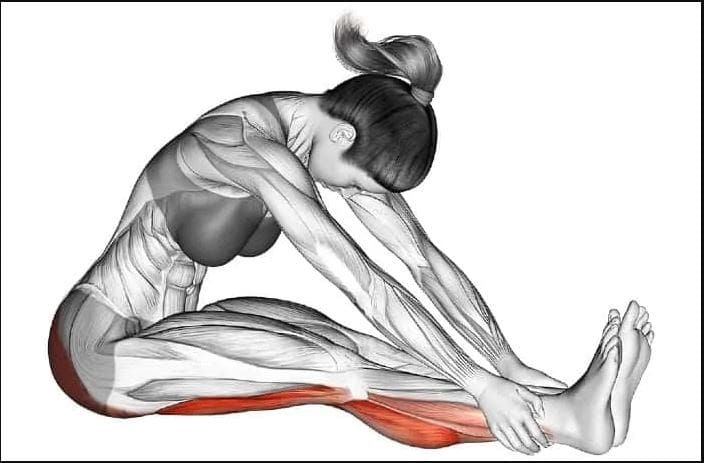
Even though trigger points can affect the soleus muscles and cause referred pain to the ankles, different methods can reduce the pain and help manage trigger points in the calves. Studies reveal that when there are multitudes of therapies that can help manage trigger points, it can help reduce the pain affecting the soleus muscle by optimizing muscle function and preventing the development of chronic pain syndromes. Besides therapies that target trigger points, corrective actions and stretches can help release the pain from the soleus muscle. Incorporating calf stretches, having a correct posture when sitting down, wearing long loose socks while sleeping, and wearing low heels can prevent the soleus muscle from shortening and help manage trigger points from re-occurring in the calves. When people start to take care of their calve muscles, it can help their mobility and stability at the ankles.
Conclusion
As part of the calf muscles and an antigravity muscle, the soleus works with the gastrocnemius to help with stability and plantarflexion to the ankles. This muscle is deep within the gastrocnemius and helps maintain good posture in the body that prevents a person from falling forward at the ankles when standing. When the soleus muscles have been overused, they can develop tiny knots in the muscle fibers known as trigger points that can cause referred pain to the ankles. Trigger points along the soleus muscles can cause overlapping features in the calves by restricting ankle dorsiflexion, causing individuals to develop low back pain associated with leaning forward. However, various therapies can manage trigger points through multiple treatments that can reduce the pain and allow stability back to the calves, enabling the individual to continue walking without feeling pain.
References
Binstead, Justin T, et al. “Anatomy, Bony Pelvis and Lower Limb, Calf – Statpearls – NCBI Bookshelf.” In: StatPearls [Internet]. Treasure Island (FL), StatPearls Publishing, 29 May 2022, https://www.ncbi.nlm.nih.gov/books/NBK459362/.
Jurkovicova, Emma. “Soleus Muscle.” Kenhub, Kenhub, 14 Feb. 2022, https://www.kenhub.com/en/library/anatomy/soleus-muscle.
Travell, J. G., et al. Myofascial Pain and Dysfunction: The Trigger Point Manual: Vol. 2:the Lower Extremities. Williams & Wilkins, 1999.
Valera-Calero, Juan Antonio, et al. “Prediction Model of Soleus Muscle Depth Based on Anthropometric Features: Potential Applications for Dry Needling.” Diagnostics (Basel, Switzerland), U.S. National Library of Medicine, 7 May 2020, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7277950/.