Table of Contents
Introduction
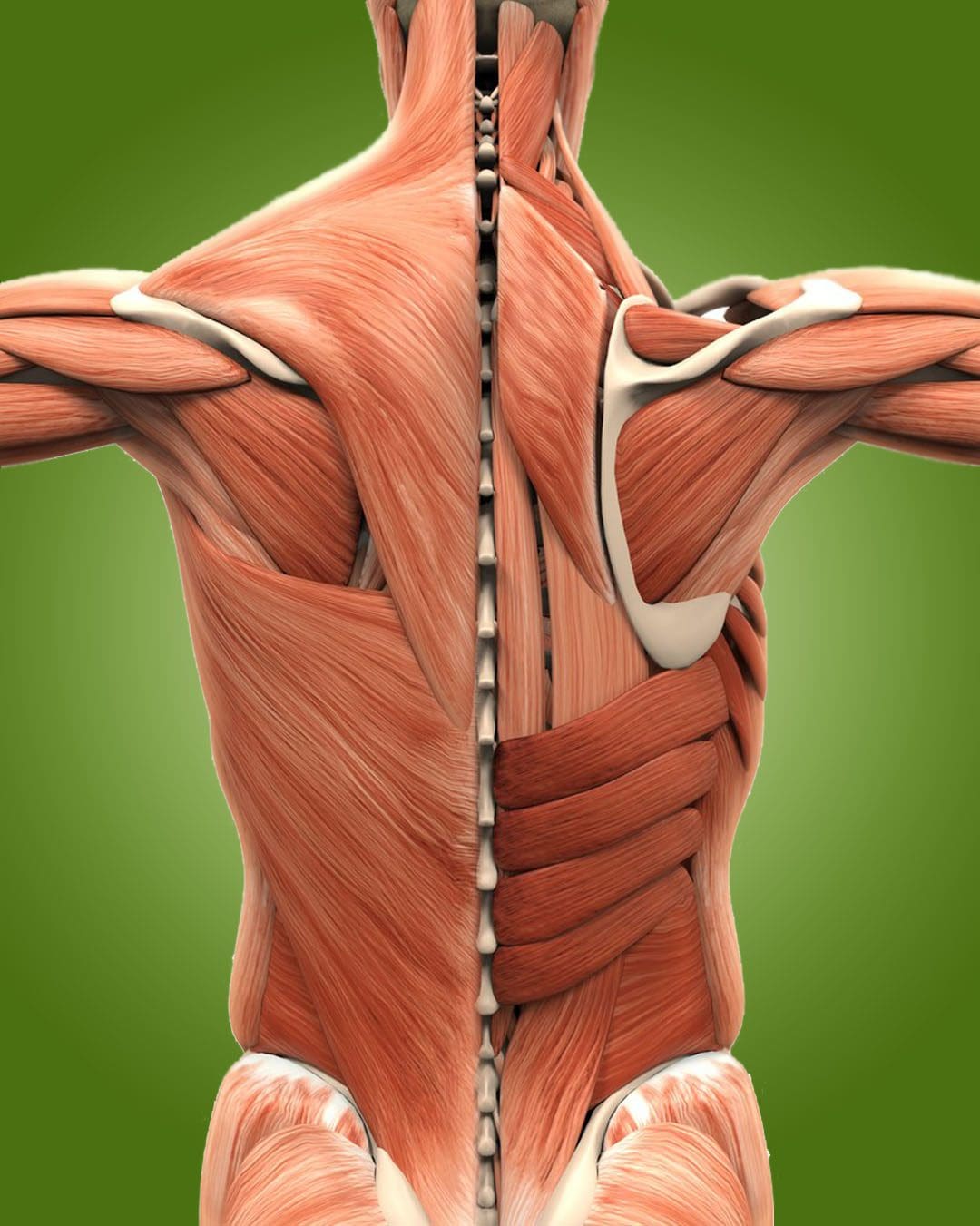
How a person walks or their gait performance can determine how their body’s balance and stability are functioning. Since the body has many muscles, ligaments, and tissues in the musculoskeletal system protecting the spine and the vital organs that work together to maintain proper functionality when a person is in motion; however, the body can succumb to numerous issues that can affect a person’s gait performance and cause the upper and lower extremities to develop myofascial trigger points in the muscle fibers. When these issues begin to cause dysfunction in the body, it can lead to many disorders associated with gait disturbances. Today we will focus on how to approach gait disturbances, how trigger points affect gait performances, and how treatment techniques like MET can help. We provide information about our patients to certified medical providers that offer available therapy techniques like MET (muscle energy techniques) for individuals dealing with gait disturbances associated with trigger points that correlate to how a person walks. We encourage each patient appropriately by referring them to our associated medical providers based on their diagnosis results. We accept that education is a spectacular way when asking our providers the most crucial questions at the patient’s acknowledgment. Dr. Alex Jimenez, D.C., assesses this information as an educational service. Disclaimer
How To Approach Gait Disturbances?
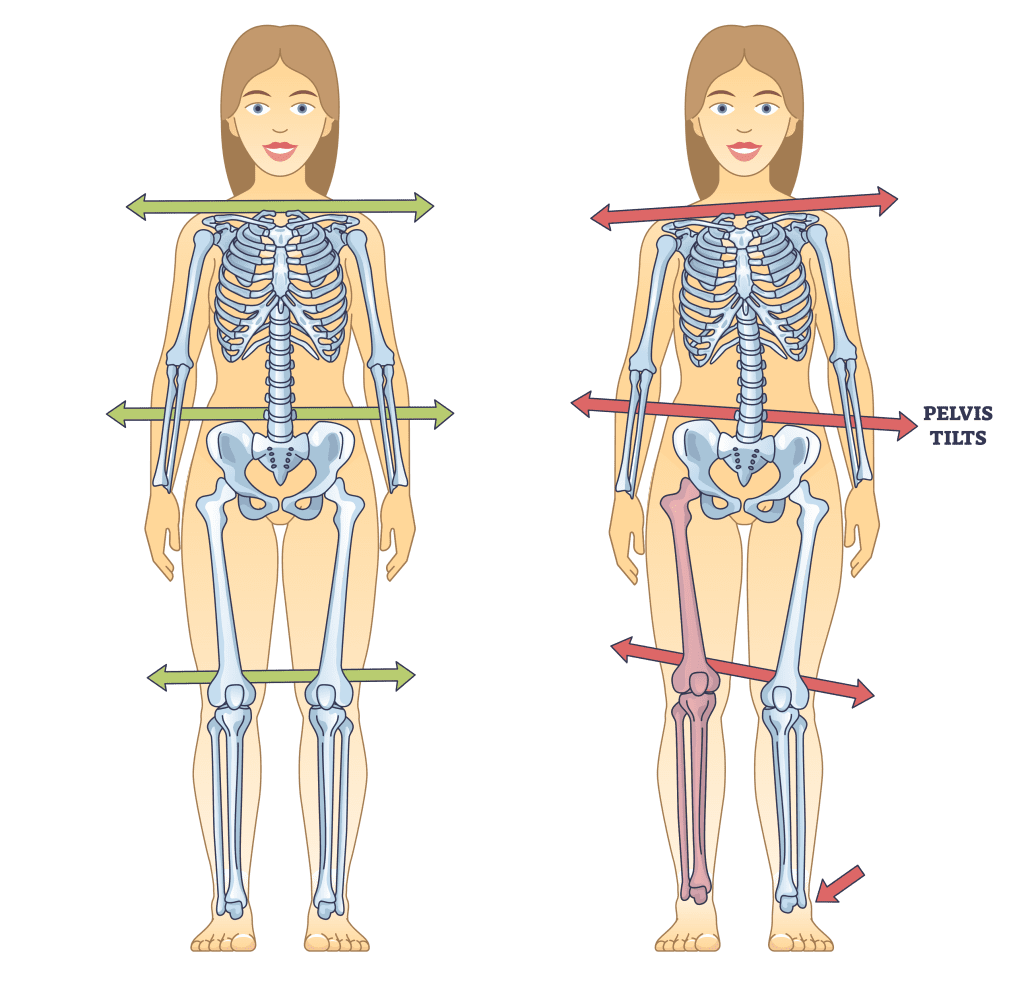
Have you been dealing with mobility issues when walking? How about feeling stiffness in your hips or lower body extremities? Or have you experienced headaches or neck pain? Many of these issues are associated with gait disturbances that can affect your ability to walk. When it comes to gait disturbances, studies reveal that underlying systemic disorders or other environmental factors could trigger the prevalence of gait disturbances. Regarding gait disturbances, it is important to know that as the body ages, it can cause issues to the musculoskeletal system naturally, and environmental factors can further affect the central nervous system to cause gait disturbances. Additional studies have mentioned that gait disorders in the elderly could potentially lead to various issues that affect a person’s quality of life. When approaching gait disturbances, many doctors will examine to see the causes of these gait disturbances that correlate with the musculoskeletal system. It could be:
- Orthopedic problems
- Neurological conditions
- Musculoskeletal disturbances
- Metabolic disturbances
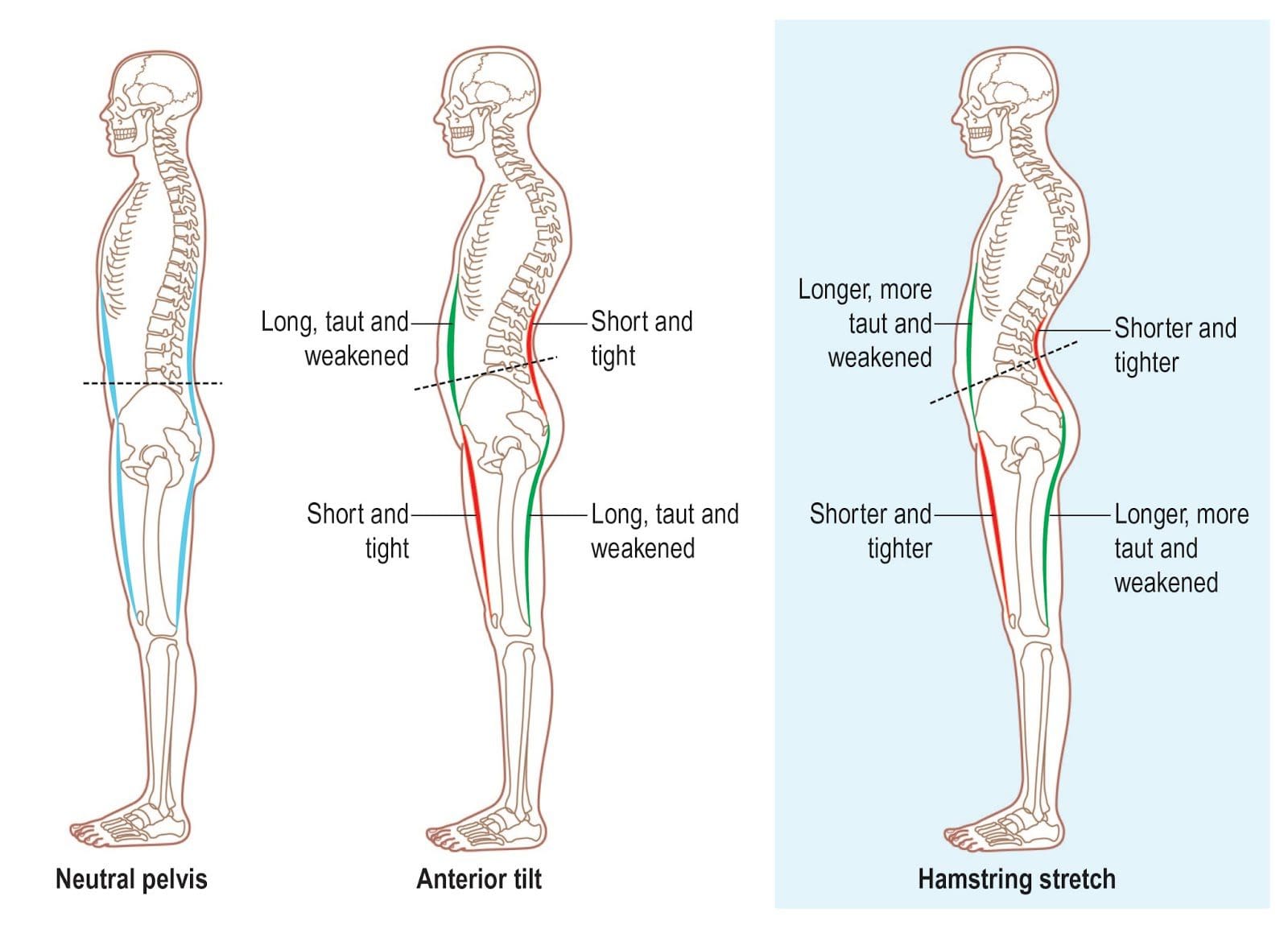
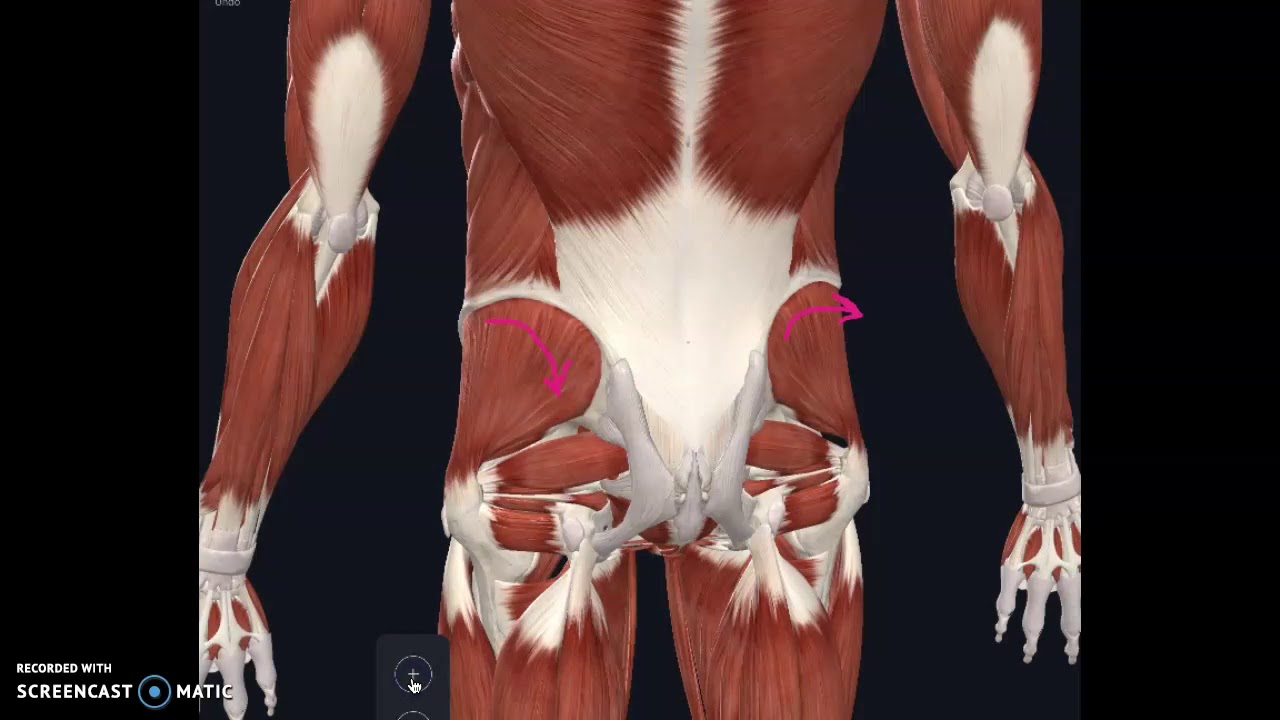
Many of these issues can cause the lower half of the body to shift the skeletal joints, leading to tight, stiff muscles and developing tiny hard nodules in the muscle fibers that can further affect gait performance.
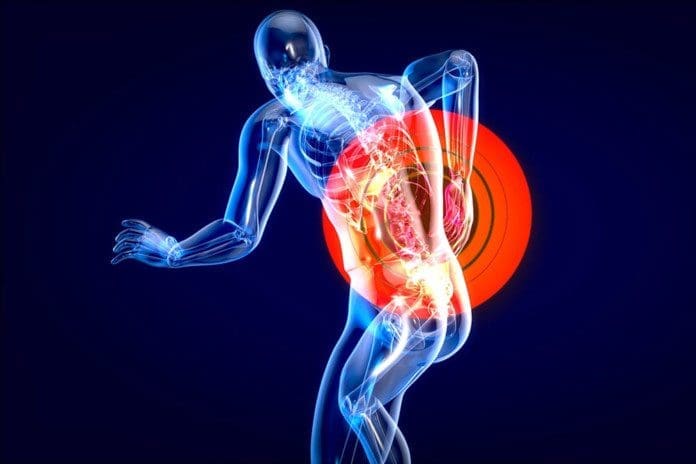
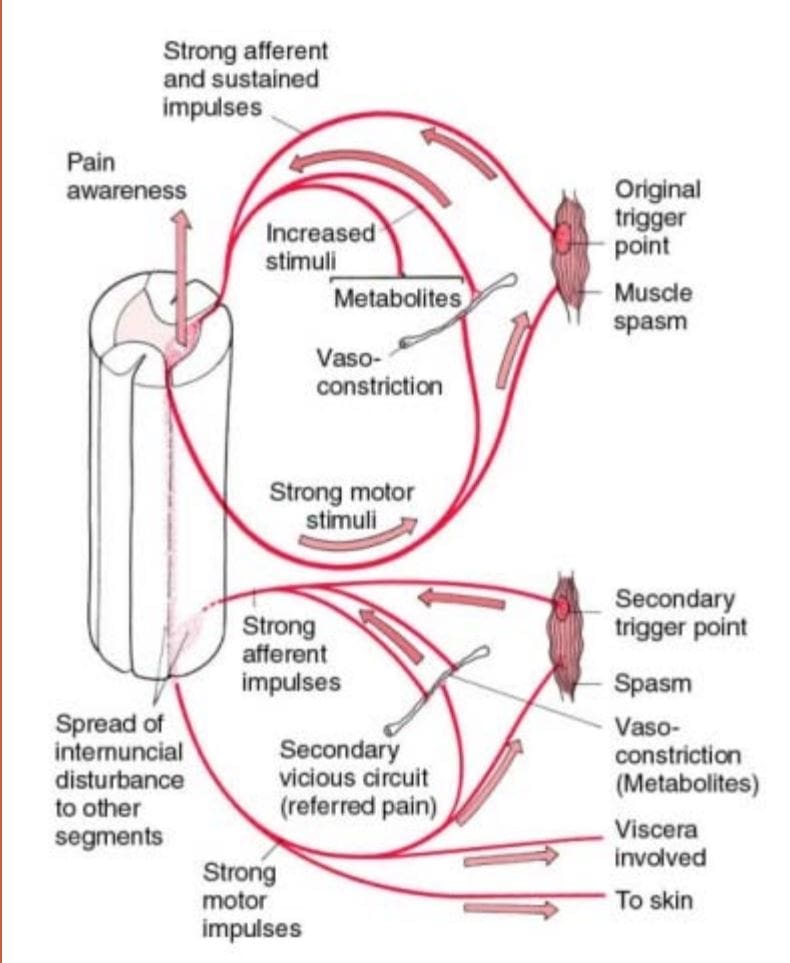
How Do Trigger Points Affect Gait Performances
So how can these tiny hard nodules affect gait performance in the body? These small hard nodules are trigger points and often correlate with overlapping risk profiles associated with musculoskeletal disorders. “Clinical Application of Neuromuscular Techniques,” written by Leon Chaitow, N.D., D.O, and Judith Walker DeLany, L.M.T., mentioned that various additional causes and maintaining factors may be associated with dysfunctional patterns that correlate with trigger point involvement. The book also says that different influences affecting the muscles can increase trigger point activity while inducing influences from acute or chronic soft tissue dysfunction. Research studies reveal that myofascial pain syndrome is a collection of sensory, motor, and autonomic symptoms that correlate with musculoskeletal symptoms like local/referred pain, decreased range of motion, and muscle weakness. When trigger points are causing problems in the muscle fibers, it can affect a person’s gait performance and cause them to lose function when walking.
Balance Issues Associated With Myofascial Trigger Points-Video

Have you been dealing with balancing issues when walking? Do your muscles feel tight in certain areas? Or do constant headaches or neck pain affect your day? The video above explains what can cause balancing issues that affect gait performance and cause numerous symptoms like headaches and neck pain. Many balance issues are associated with myofascial trigger points affecting your gait performance. Myofascial trigger points can overlap risk profiles that can affect the muscle fibers in the body. Many correlating factors can affect a person’s gait performance, leading to musculoskeletal disorders related to trigger points. When musculoskeletal disorders are correlated with myofascial trigger points, it can decrease a person’s health and wellness if not treated early on. Fortunately, some treatments incorporate techniques to reduce muscle and joint pain while alleviating symptoms associated with myofascial trigger points.
How The MET Technques Helps With Gait Performance & Trigger Points
When a person is dealing with imbalances affecting their gait performance and having overlapping risk profiles associated with trigger points, treatment techniques can help improve their gait while reducing pain-like symptoms. Many pain specialists will use the MET technique (muscle energy technique) to help stretch affected muscles that are stiff and help regain mobility back to the body. Therapies like chiropractic care utilize this technique combined with spinal manipulation to help realign the body while loosening up stiff muscles affecting gait performance. When a person continues treatment care to regain mobility, it allows them to be aware of how they walk and carry themselves without pain.
Conclusion
How a person walks is how their balance and stability function in different environments. A person’s gait performance has to maintain the functionality that allows the various muscles, ligaments, and tissues in the musculoskeletal system to move. When environmental factors or musculoskeletal disorders affect the different muscles, it can cause overlapping issues that affect gait performance. To that point, it leads to stiffness and pain associated with trigger points. Luckily techniques like the MET combined with chiropractic care can help realign the body and loosen up stiff muscles and joints to regain mobility back to the body and help improve overall gait performance.
References
Chaitow, Leon, and Judith Walker DeLany. Clinical Application of Neuromuscular Techniques. Churchill Livingstone, 2002.
Jafri, M Saleet. “Mechanisms of Myofascial Pain.” International Scholarly Research Notices, U.S. National Library of Medicine, 2014, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4285362/.
Marshall, Frederick J. “Approach to the Elderly Patient with Gait Disturbance.” Neurology. Clinical Practice, U.S. National Library of Medicine, June 2012, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3613197/.
Pirker, Walter, and Regina Katzenschlager. “Gait Disorders in Adults and the Elderly : A Clinical Guide.” Wiener Klinische Wochenschrift, U.S. National Library of Medicine, Feb. 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5318488/.









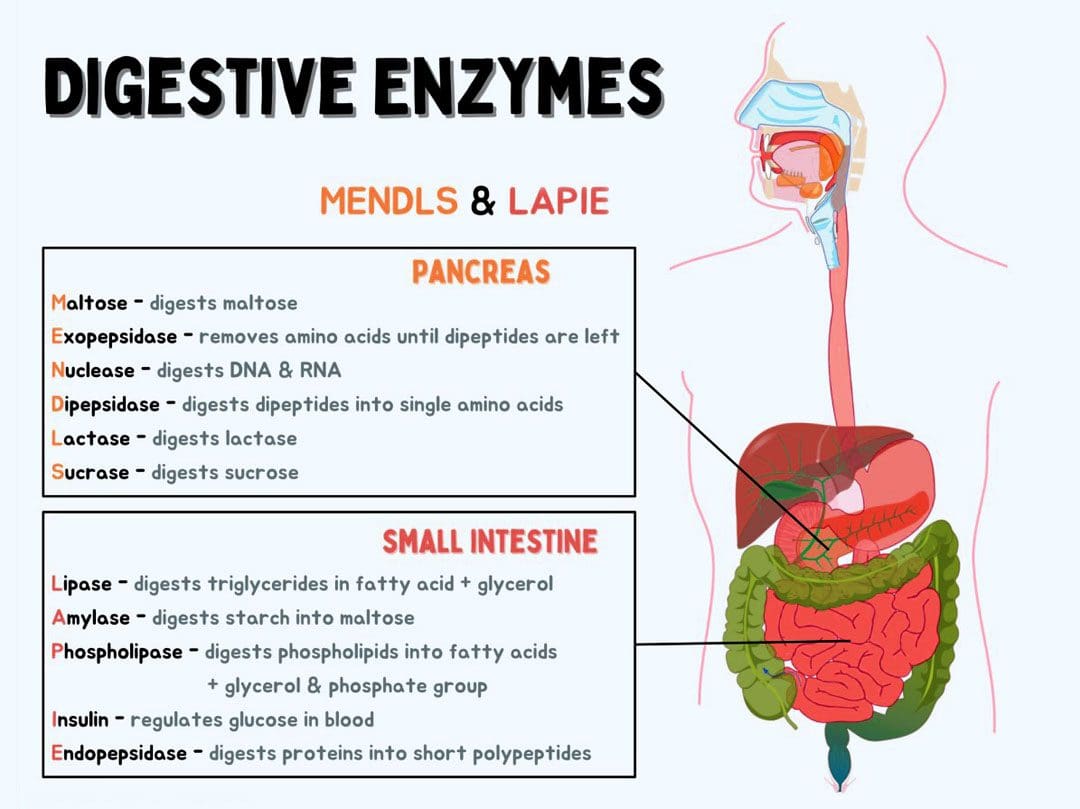 Digestive Enzymes
Digestive Enzymes