Table of Contents
Introduction
Inside the body lies the internal organs that provide the nutrients and energy for the body to stay in motion. The gut system helps the body energy by digesting the consumed food that gets turned into energy and nutrients beneficial for the vital organs, muscles, tissues, and growth that the body needs. The gut system also helps regulate the other body systems like the musculoskeletal system, the immune system, central nervous system, and the endocrine system. The gut system operates by transporting these nutrients to make the body operational, to name a few needs. When unwanted issues start to enter the gut system and cause havoc, it can lead to many chronic problems that will cause the body to be in constant pain while causing other issues that affect the entire body. Today’s article will look at how different gut issues start to affect the body and how an amino acid named glutamine can provide beneficial relief to various gut issues. Referring patients to qualified and skilled providers who specialize in gastroenterology treatments. We guide our patients by referring to our associated medical providers based on their examination when it’s appropriate. We find that education is essential for asking insightful questions to our providers. Dr. Alex Jimenez DC provides this information as an educational service only. Disclaimer
Can my insurance cover it? Yes, it may. If you are uncertain, here is the link to all the insurance providers we cover. If you have any questions or concerns, please call Dr. Jimenez at 915-850-0900.
How Gut Issues Affect The Body
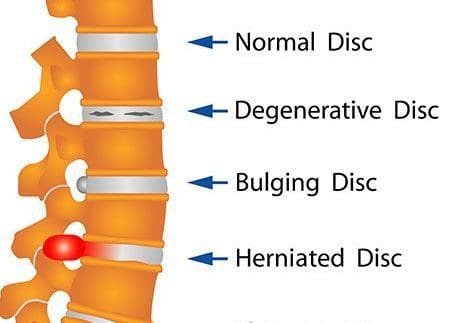
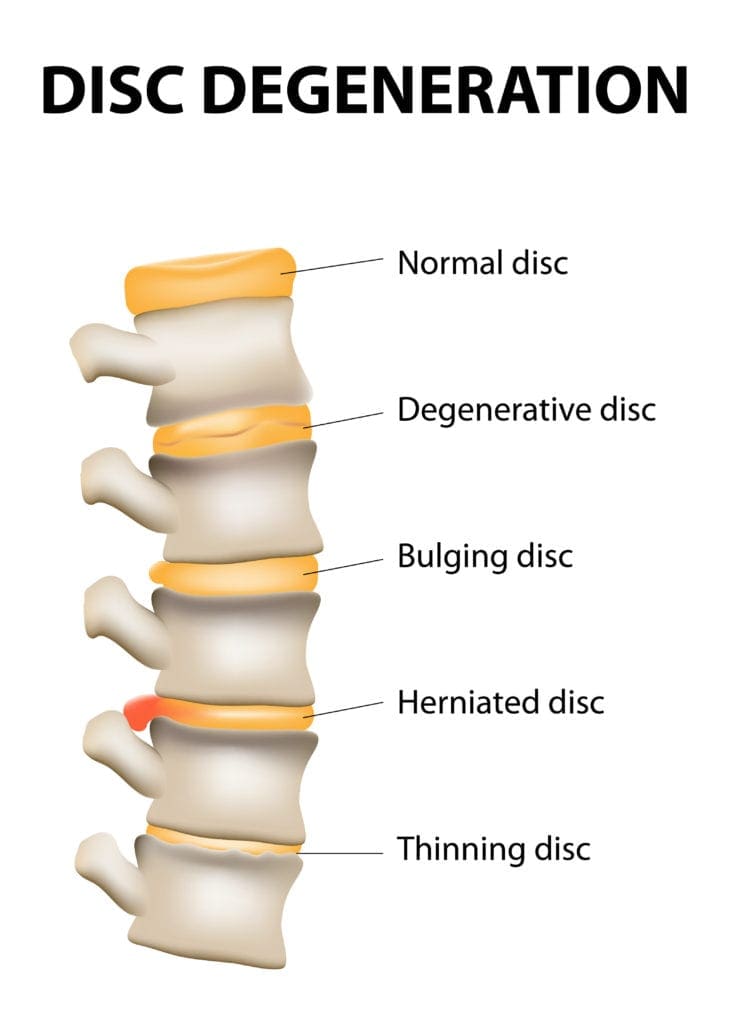
Have you been experiencing pain located in your gut? Does your gut seem to be extra sensitive after consuming food? Have you been anxious or stressed that it has been affecting your body? Experiencing these symptoms are signs that you might have some gut issues that are affecting your body. Research studies have found that gut issues or disorders usually develop when the gut has either underproduced or overproduced the beneficial gut bacteria that can influence harmful bacteria to attack the gut’s intestinal walls. Gut issues can also be influenced due to lifestyle choices or autoimmune disorders that affect the gut and the rest of the body and its systems. Additional information has found that when the microbiome is being challenged with factors that change the physiology of the gut microbiome. These changes will cause an increase in the intestinal permeability, which allows the harmful bacteria to leak out, causing the immune system to attack the exposed bacteria at the intestinal walls leading to inflammatory issues.
Other research studies have found that gut bacteria provides an essential role in the body as it helps supply the vital nutrients beneficial for the body’s health. When abnormal changes affect gut bacteria, the gut ecosystem accelerates dysbiosis, causing many chronic issues. Many individuals will begin to lose their quality of life due to pain. Fortunately, there are ways to alleviate the chronic issues affecting the gut and even help lower the harmful bacteria by replenishing the beneficial bacteria while reducing inflammatory markers.
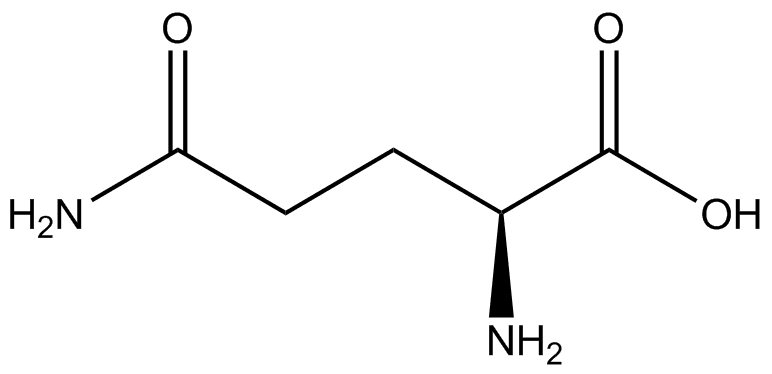
An Overview About Glutamine-Video
Have you been experiencing issues that are affecting your gut? Has your torso area been feeling tender to the touch? How about random pain spots that are in your abdomen? You could be experiencing gut issues affecting your overall health and wellness. Why not incorporate glutamine into your daily supplementation. Research studies mentioned that glutamine is an amino acid with beneficial properties in replenishing the immune system and metabolizing in the gut and other vital organs that need glutamine to nourish the cellular structure for the body to feel better and provide energy for many individuals. The video above includes information about the benefits of glutamine and how it can help the body.
How Glutamine Helps The Gut
As stated earlier, glutamine is an amino acid with beneficial properties that are utilized to provide energy for the entire body. Research studies have shown that glutamine in the gut system can maintain the intestinal structure and function as the body ages while regulating the tight junction proteins. Glutamine has also helped modulate the gut intestinal permeability effects of HPA-axis stress that affects the gut and protects the cells from apoptosis and cellular stress. Additional research studies have provided that when individuals take glutamine as part of their daily regime, they will have a better inflammatory response and redox balance in the gut with the combination of physical activities. Utilizing glutamine for gut health can help improve the gut function and gastrointestinal permeability function for many athletic individuals.
Conclusion
Overall, the gut system utilizes glutamine for optimal gut health in dampening the effects of gut issues and disorders that will affect the body. The gut provides the transportation of the essential nutrients for the rest of the body systems that need them to function correctly. When unwanted factors or unhealthy lifestyles affect the gut system, it can increase the harmful bacteria in the gut and diminish the beneficial bacteria. This will cause the inflammatory cytokines to attack the intestinal permeability walls and cause more issues that will affect the body. Beneficial supplements and nutrients that help alleviate inflammatory factors or alleviate gut issues are there to provide relief by dampening these harmful effects and repairing the body. Incorporating glutamine into your gut will help the body recover over time and become pain-free.
References
Almeida, Ewin B, et al. “L-Glutamine Supplementation Improves the Benefits of Combined-Exercise Training on Oral Redox Balance and Inflammatory Status in Elderly Individuals.” Oxidative Medicine and Cellular Longevity, Hindawi, 22 Jan. 2020, www.ncbi.nlm.nih.gov/pmc/articles/PMC7204202/.
Clapp, Megan, et al. “Gut Microbiota’s Effect on Mental Health: The Gut-Brain Axis.” Clinics and Practice, PAGEPress Scientific Publications, Pavia, Italy, 15 Sept. 2017, www.ncbi.nlm.nih.gov/pmc/articles/PMC5641835/.
Cruzat, Vinicius, et al. “Glutamine: Metabolism and Immune Function, Supplementation and Clinical Translation.” Nutrients, MDPI, 23 Oct. 2018, www.ncbi.nlm.nih.gov/pmc/articles/PMC6266414/.
Kim, Min-Hyun, and Hyeyoung Kim. “The Roles of Glutamine in the Intestine and Its Implication in Intestinal Diseases.” International Journal of Molecular Sciences, MDPI, 12 May 2017, www.ncbi.nlm.nih.gov/pmc/articles/PMC5454963/.
Nouvenne, Antonio, et al. “Digestive Disorders and Intestinal Microbiota.” Acta Bio-Medica : Atenei Parmensis, Mattioli 1885, 17 Dec. 2018, www.ncbi.nlm.nih.gov/pmc/articles/PMC6502202/.
Zhang, Yu-Jie, et al. “Impacts of Gut Bacteria on Human Health and Diseases.” International Journal of Molecular Sciences, MDPI, 2 Apr. 2015, www.ncbi.nlm.nih.gov/pmc/articles/PMC4425030/.