Table of Contents
Introduction
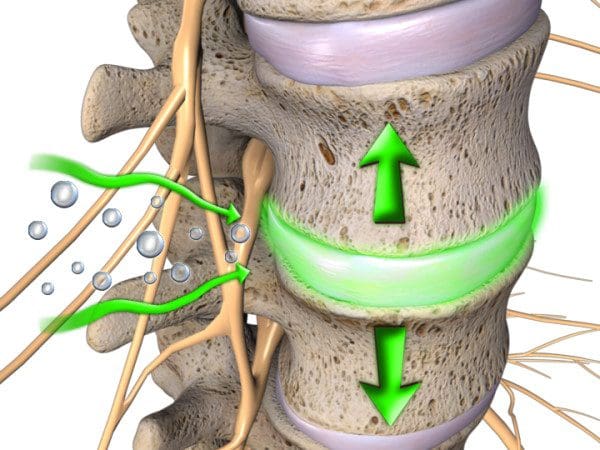
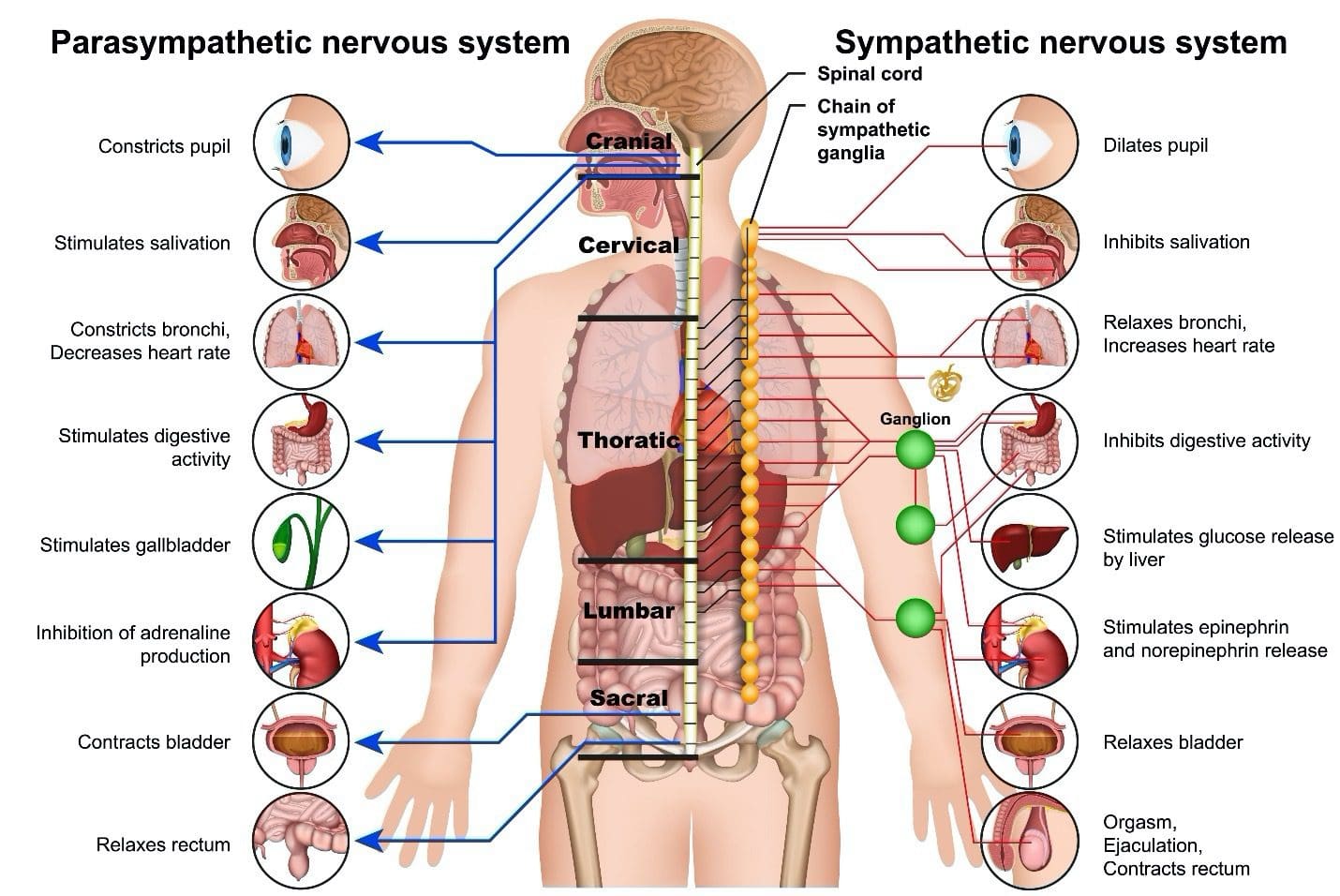
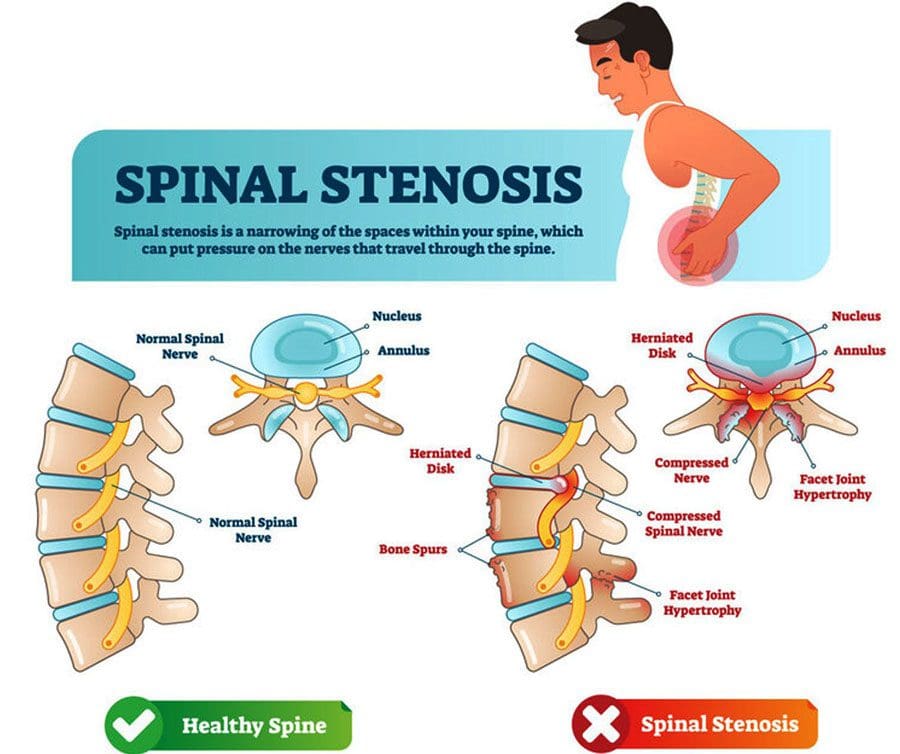
The body has many nerve roots that are intertwined and coming out from the spinal cord, which is part of the nervous system. One of the main components of the nervous system is the vagus nerve, which is part of the parasympathetic nervous system as it helps inform the brain about the state of the inner organs in the body. The vagus nerve helps maintain the body’s metabolism and homeostasis from diseases and injuries that occur either inside or outside the body. Many inner organs, muscles, or tissues get affected when a person has suffered from an injury or developed infections in their body. They can cause many symptoms that can dysfunction the body. It can affect the spine, nerve roots, internal organs, and joints, making the individual feel a sense of hopelessness. Today’s article will look at the unique connection of viscerosomatic reflexes and how it affects the body, as well as how viscerosomatic pain can affect the spine causing the individual many spinal issues. We refer patients to certified, skilled providers specializing in osteopathic and chiropractic treatments. We also guide our patients by referring to our associated medical providers based on their examination when it’s appropriate. We find that education is critical for asking insightful questions to our providers. Dr. Alex Jimenez DC provides this information as an educational service only. Disclaimer
Can my insurance cover it? Yes, it may. If you are uncertain, here is the link to all the insurance providers we cover. If you have any questions or concerns, please call Dr. Jimenez at 915-850-0900.
What Are Viscerosomatic Reflexes?
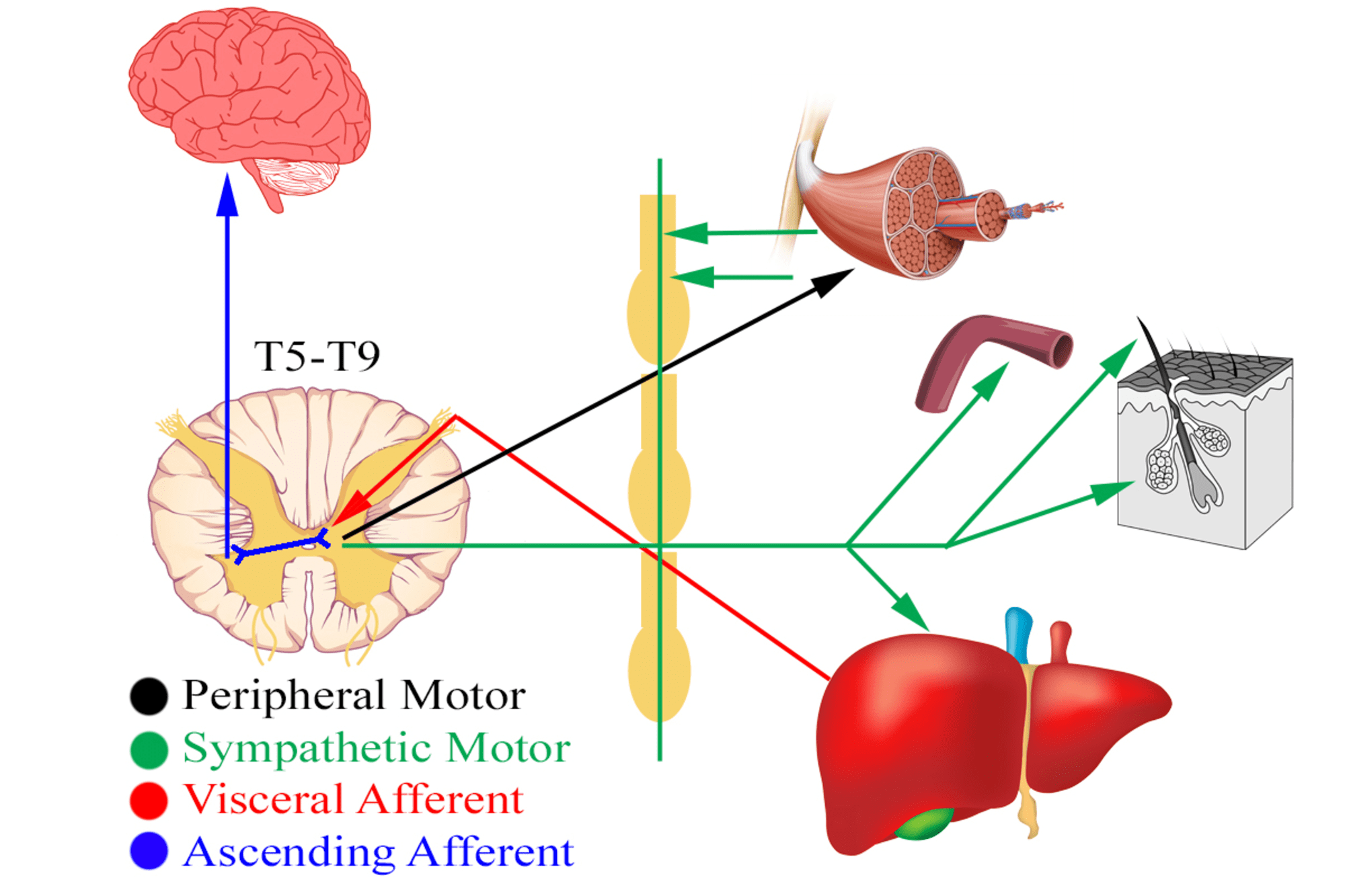
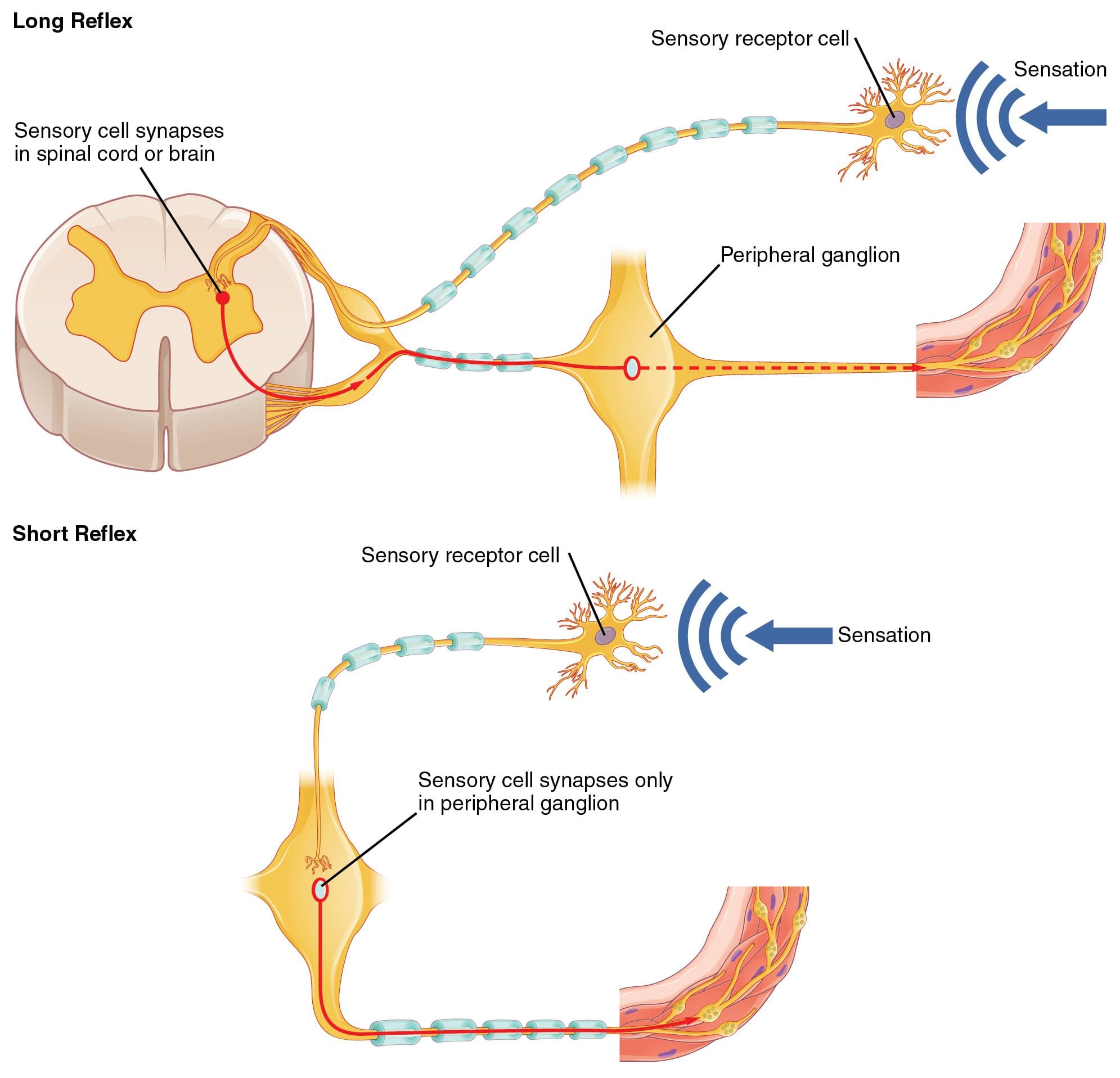
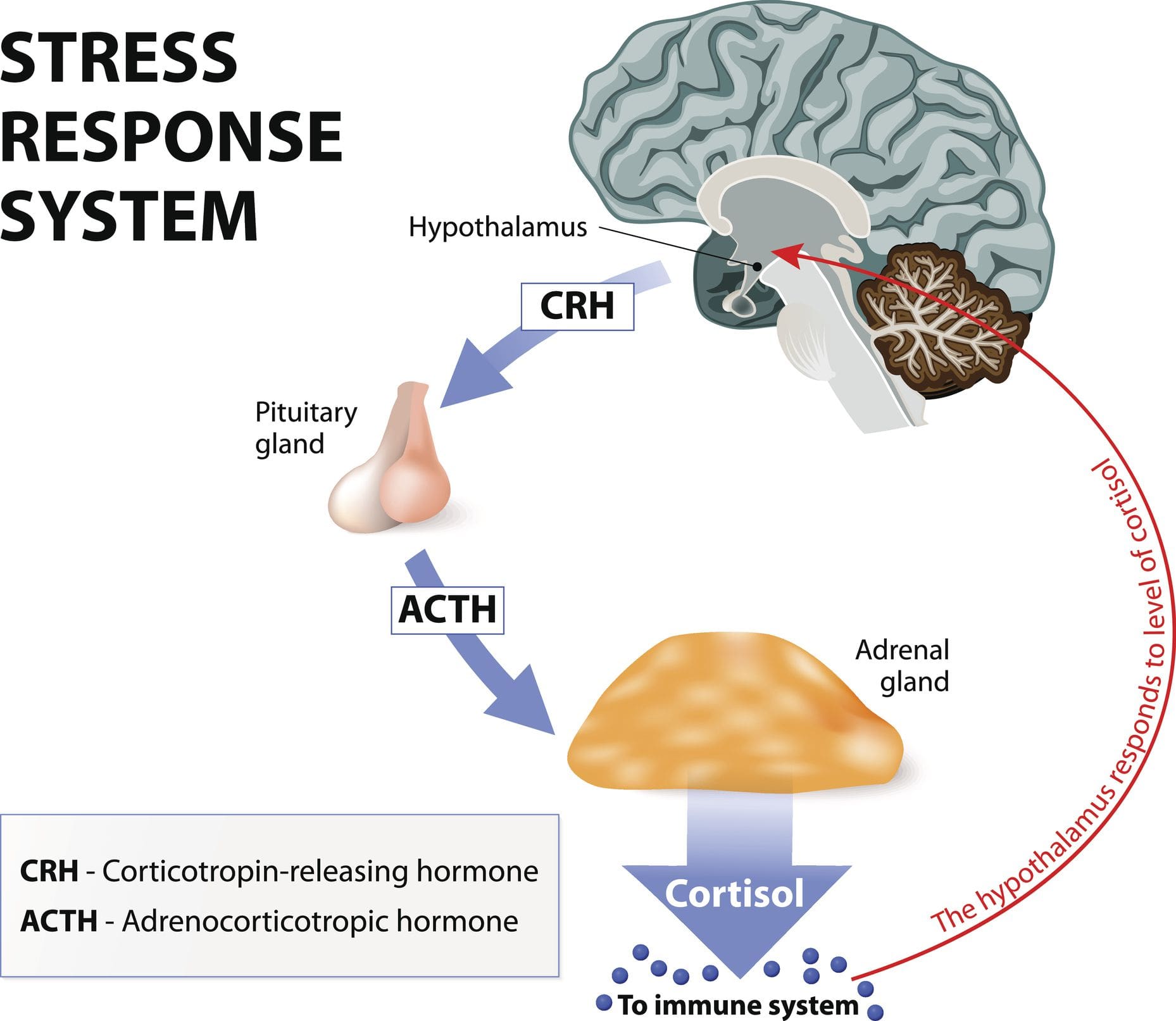
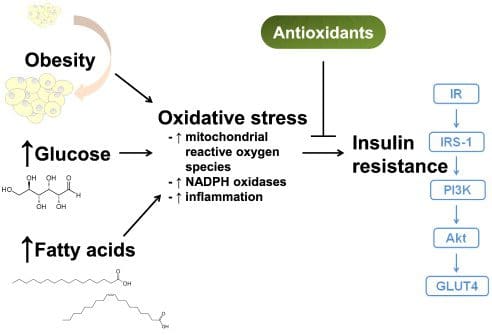
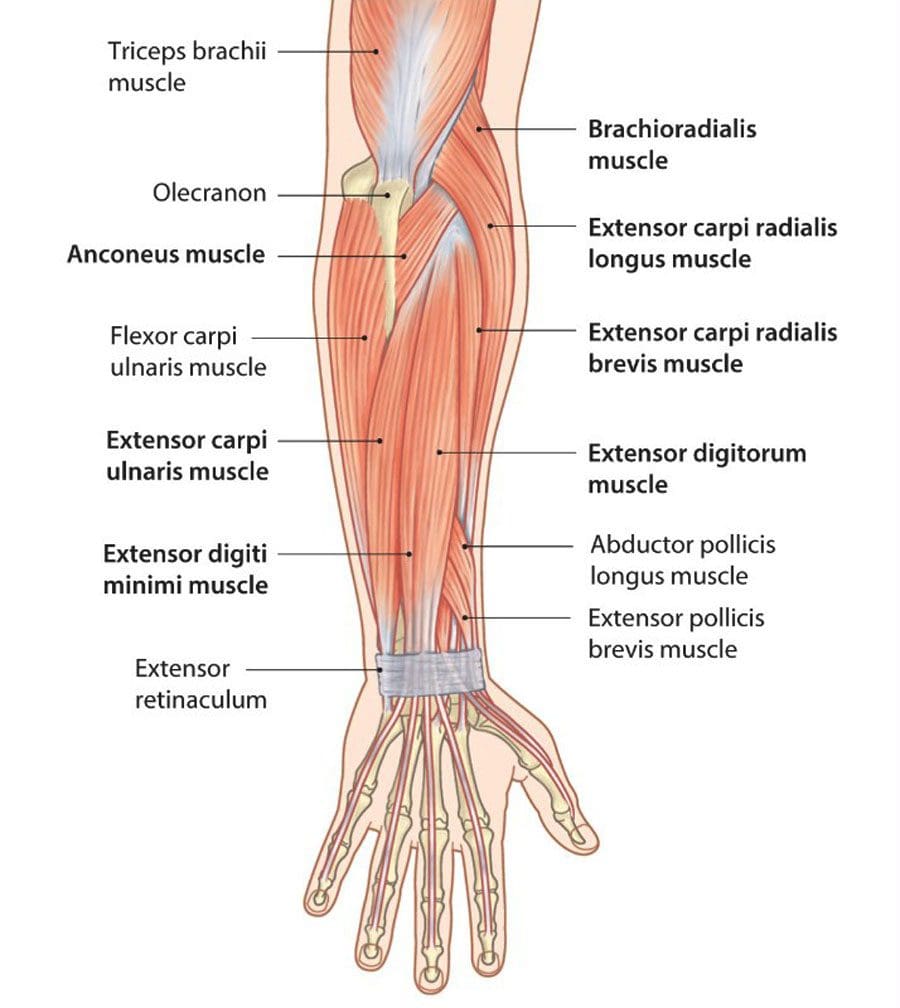
Have you experienced pain in your arms, legs, or back? How about feeling dysfunctional in your urinary tract? Have you noticed that not only your chest has started to hurt but also your gut and lower back? Many of these are signs of you having pain due to your viscerosomatic reflexes in your body. Research studies have defined viscerosomatic as regular visceral activity in the body stimulated by the somatosensory nerves that can help recognize abnormal viscerosomatic reflexes. These nerves are connected to the central nervous system, which travels through the spinal cord and can affect the body. The best example is when a doctor is giving a reflex test and uses a rubber mallet to hit the knee to see if a person still has reflexes in their body. Since the vagus nerve is part of the parasympathetic nervous system, when it becomes damaged, it can cause numerous effects on the body research studies have found that any visceral disturbances that are affecting the human body can cause an increase in muscle tension and decrease the pain in the corresponding spinal ligament that can restrict the muscle mobility to the tissues and affecting either the motor or sympathetic nerve. This causes the body to experience pain affecting one part of the body to the corresponding affected nerve.
How Does It Affect The Body?
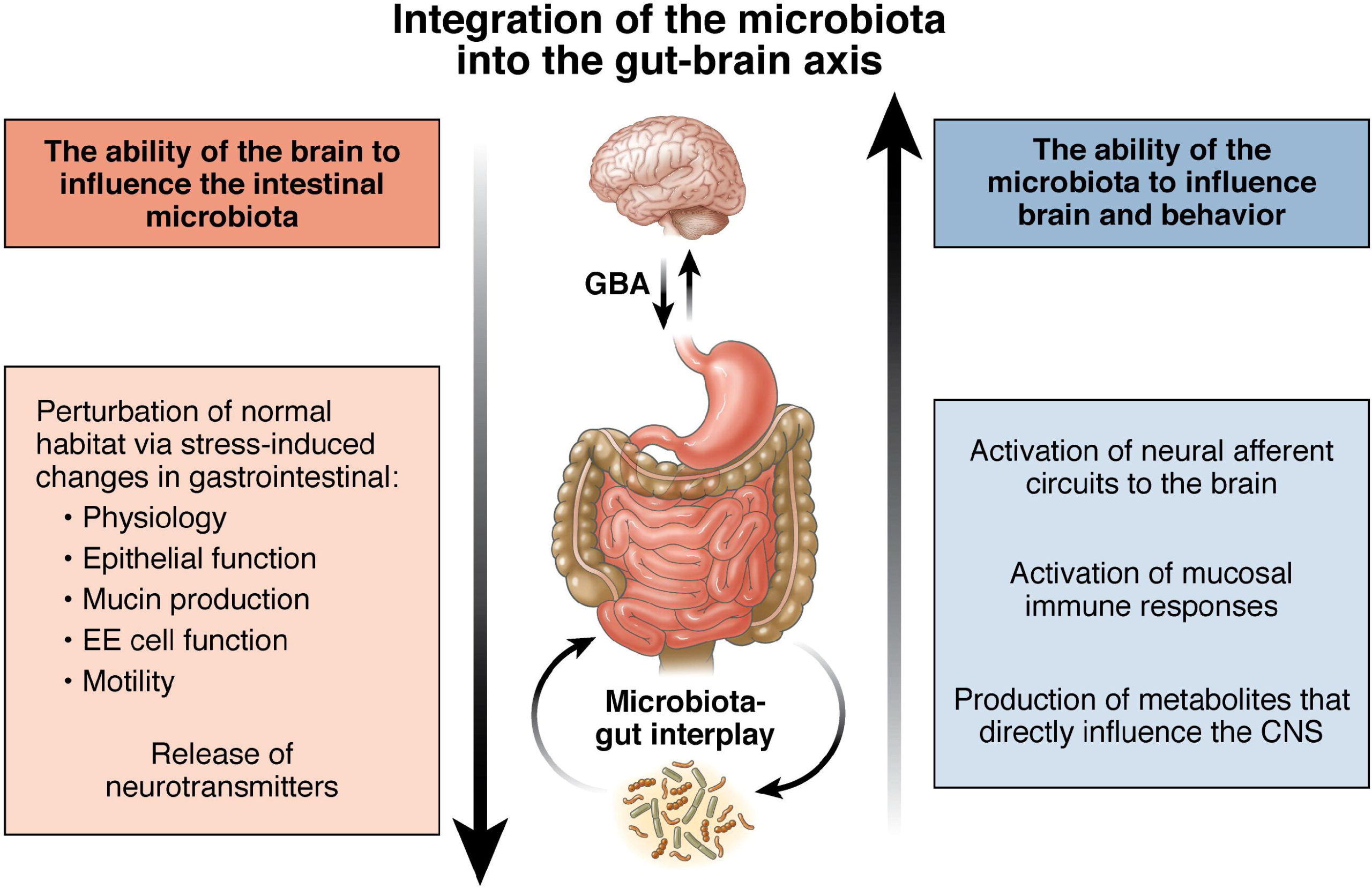
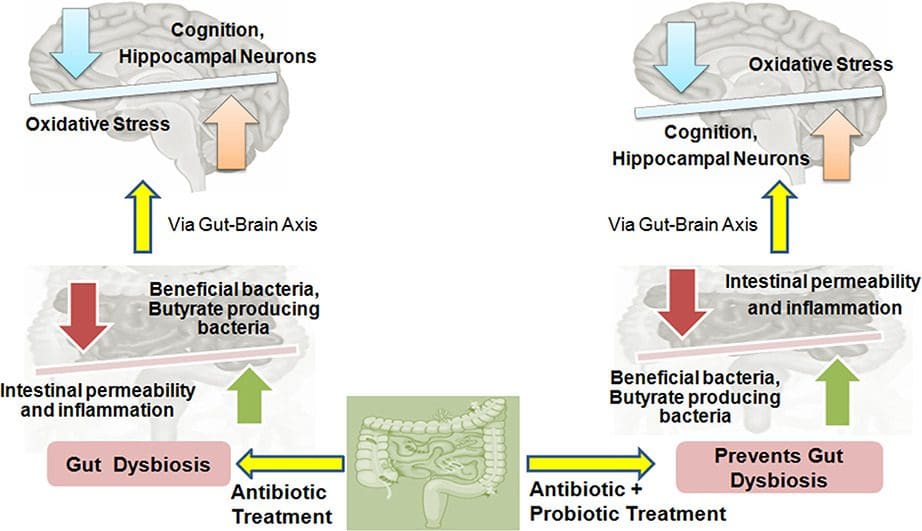
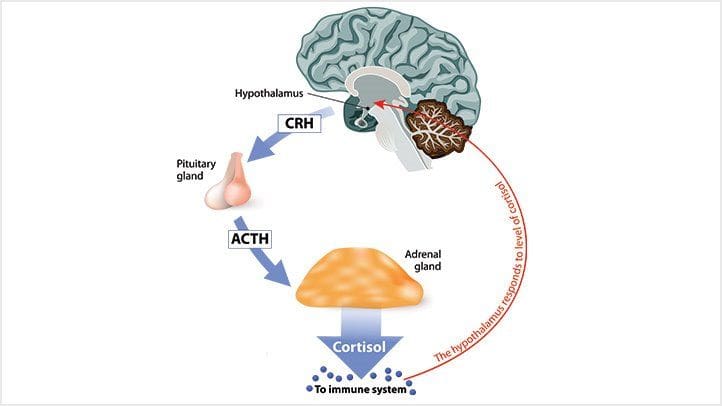
Since the body has so many connections like the gut-brain axis, which helps regulate the body’s metabolism and homeostasis, the endocrine system that allows the transport of hormones to the rest of the muscles, tissues, and organs through the nerve roots, and the nerve roots themselves are connected as they help with the sensory-motor function with the arms and legs, so the body can move around. When these connections are being damaged and start to affect the rest of the body, it can lead to other health problems that do affect the body. Research studies have found that when the body is suffering from visceral pain in the organs can affect different areas. A couple of examples include:
- Bladder issues affecting the perineal area
- Cardiovascular disorders causing arm and neck pain
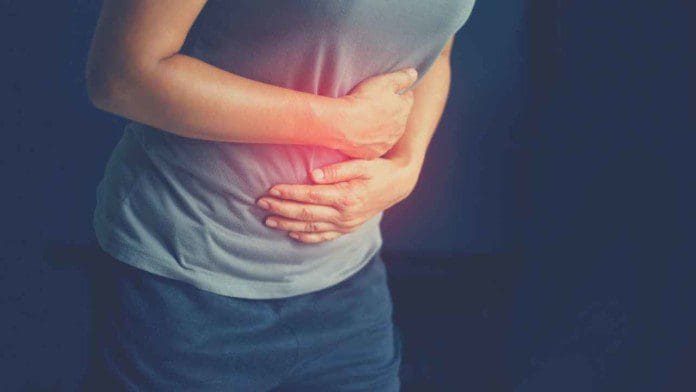
- GI disorders causing discomfort
Even though visceral pain’s effects are not life-threatening, it can dampen a person’s mood by causing a negative impact associated with distress, sleep, and work disturbances, and even causing sexual dysfunction in the body.
An Overview Of Viscerosomatic Reflexes-Video

Have you experienced cardiovascular issues that are causing arm and neck pain? Have you been feeling some discomfort in your gut or your pelvic area? Have you been experiencing pain that is negatively impacting your quality of life? This could be due to viscerosomatic pain affecting your body and causing these symptoms. The video above explains how the viscerosomatic reflexes are connected to their corresponding muscles and organs. When the body is suffering from issues that affect the related muscles, it is known as viscerosomatic pain. Research studies have shown that individuals suffering from viscerosomatic pain will have multifaceted problems in the viscerosomatic reflexes. This type of pain does affect the spinal neurons causing the visceral neurons to become overly sensitive in the body and the affected areas.
How Does Viscerosomatic Pain Affect The Spine?
Research studies have found that viscerosomatic can affect the spine by affecting the gut system. Many individuals that are suffering from IBS (irritable bowel syndrome) will often complain about being in pain in their torso areas. They don’t realize that processing the visceral and somatic stimuli can cause the gut to become hypersensitive and affect the spinal cord neurons to overlap. Another research study has mentioned that pelvic pain in an individual can cause more symptoms that involve many organ systems causing visceral symptoms combined with somatovisceral convergence. When viscerosomatic pain affects many body parts, it can be difficult for a diagnosis to be conducted.
Conclusion
The body has many nerve roots that connect the body by branching out of the spine and providing sensory-motor functions to the corresponding muscles and tissues. When the body becomes injured, it can cause nerve not only damage to the body but also affect the muscles and organs. This is known as viscerosomatic pain and can be challenging to diagnose due to its being multifaceted with multiple symptoms. This pain can cause the affected organs to become hypersensitive and impact a person’s quality of life. When the body starts healing from viscerosomatic pain, the effects will become less for the individual as they heal the affected organs.
References
Bath, Megan, and Justin Owens. “Physiology, Viscerosomatic Reflexes.” In: StatPearls [Internet]. Treasure Island (FL), StatPearls Publishing, 8 May 2022, www.ncbi.nlm.nih.gov/books/NBK559218/.
Hoffman, Donna. “Understanding Multisymptom Presentations in Chronic Pelvic Pain: The Inter-Relationships between the Viscera and Myofascial Pelvic Floor Dysfunction.” Current Pain and Headache Reports, U.S. National Library of Medicine, Oct. 2011, pubmed.ncbi.nlm.nih.gov/21739128/.
Sengupta, Jyoti N. “Visceral Pain: The Neurophysiological Mechanism.” Handbook of Experimental Pharmacology, U.S. National Library of Medicine, 2009, www.ncbi.nlm.nih.gov/pmc/articles/PMC3156094/.
Sikandar, Shafaq, and Anthony H Dickenson. “Visceral Pain: The Ins and Outs, the Ups and Downs.” Current Opinion in Supportive and Palliative Care, U.S. National Library of Medicine, Mar. 2012, www.ncbi.nlm.nih.gov/pmc/articles/PMC3272481/.
Silva, Andréia Cristina de Oliveira, et al. “Effect of Osteopathic Visceral Manipulation on Pain, Cervical Range of Motion, and Upper Trapezius Muscle Activity in Patients with Chronic Nonspecific Neck Pain and Functional Dyspepsia: A Randomized, Double-Blind, Placebo-Controlled Pilot Study.” Evidence-Based Complementary and Alternative Medicine : ECAM, Hindawi, 11 Nov. 2018, www.ncbi.nlm.nih.gov/pmc/articles/PMC6252226/.
Verne, G Nicholas, et al. “Viscerosomatic Facilitation in a Subset of IBS Patients, an Effect Mediated by N-Methyl-D-Aspartate Receptors.” The Journal of Pain, U.S. National Library of Medicine, Sept. 2012, www.ncbi.nlm.nih.gov/pmc/articles/PMC3489925/.