How does spinal decompression help reduce somatosensory pain associated with individuals dealing with back and leg pain?
Table of Contents
Introduction
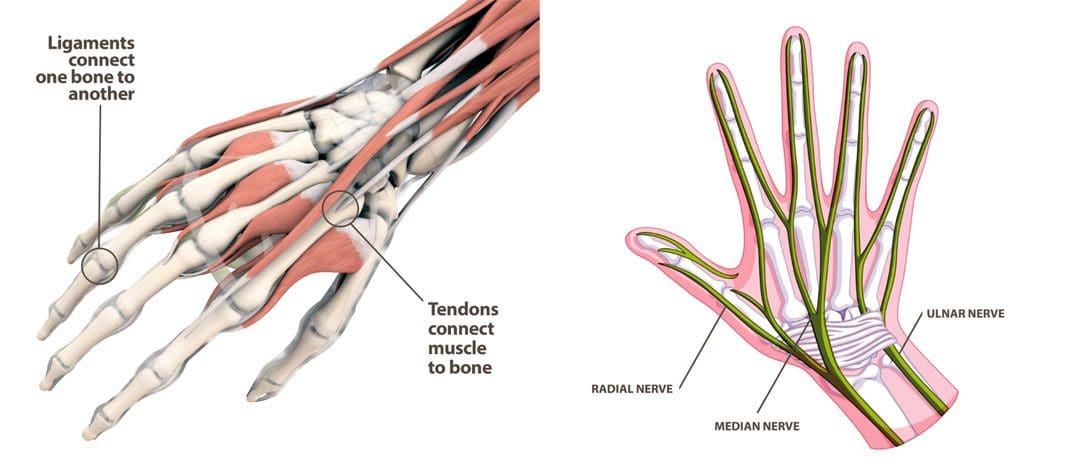
As we all know, the human body is a complex system that works together to perform various actions without feeling pain or discomfort. With muscles, organs, tissues, ligaments, bones, and nerve roots, each component has its job and interacts with other body parts. For instance, the spine collaborates with the central nervous system to instruct the muscles and organs to function correctly. Meanwhile, the nerve roots and muscles work together to provide mobility, stability, and flexibility to the upper and lower body extremities. However, as time passes, the body ages naturally, and this can lead to unwanted issues. Normal and traumatic factors can interfere with the neuron signals from the brain and cause somatosensory pain in the upper and lower extremities. This pain-like sensation can affect each body section, making the individual miserable. Luckily, there are ways to reduce somatosensory pain and provide relief to the body. Today’s article explores how somatosensory pain can impact the lower extremities, particularly the legs and back, and how non-surgical treatments like spinal decompression can alleviate somatosensory pain in the lower extremities. At the same time, we work hand-in-hand with certified medical providers who use our patient’s information to treat and mitigate somatosensory pain affecting the legs and back. We also inform them that non-surgical treatments like spinal decompression can help alleviate residual pain-like symptoms from the lower extremities. We encourage our patients to ask essential and important questions while seeking education from our associated medical providers about their pain. Dr. Alex Jimenez, D.C., incorporates this information as an educational service. Disclaimer
How Does Somatosensory Pain Affect The Legs & Back?
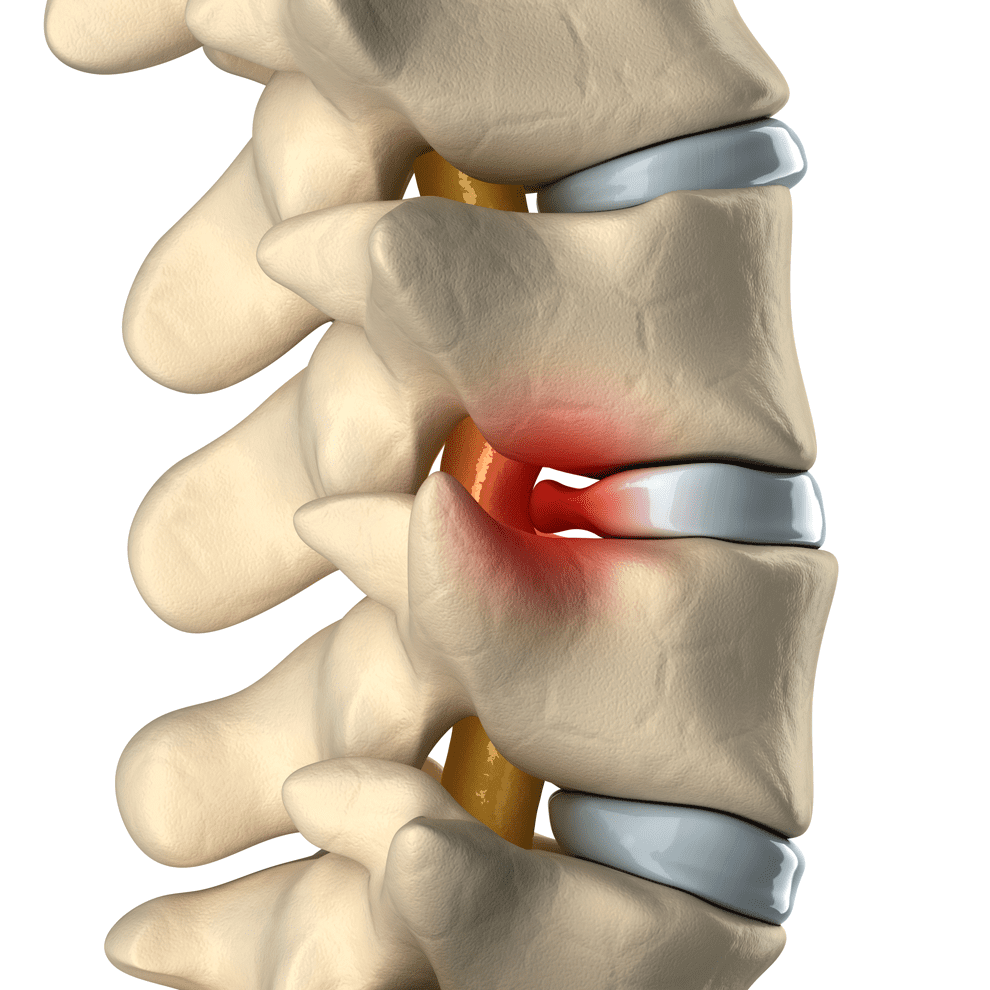
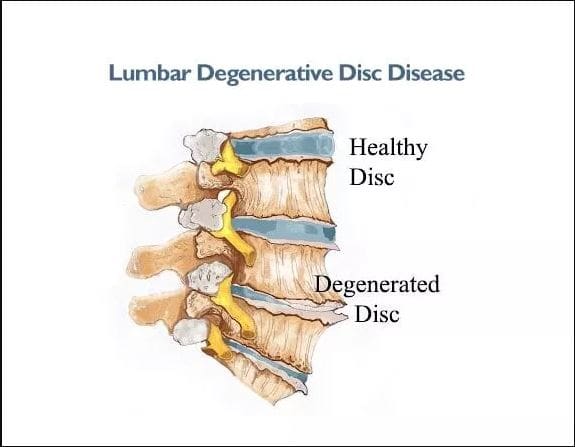
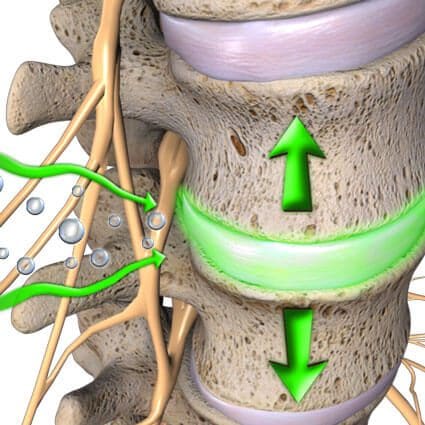
Are you experiencing numbness or tingling in your legs or back that disappears after a few minutes? Do you feel questionable pain in your lumbar spine after work? Or do you feel a warm sensation in the back of your legs that turns into sharp shooting pain? These issues may be related to the somatosensory system within the central nervous system, which provides voluntary reflexes to muscle groups. When normal movements or traumatic forces cause problems to the somatosensory system over time, it can lead to pain that affects the body’s extremities. (Finnerup, Kuner, & Jensen, 2021) This pain may be accompanied by burning, pricking, or squeezing sensations that affect the lumbar region. Many factors can be associated with somatosensory pain, which is part of the central nervous system and works with the spinal cord. When the spinal cord becomes compressed or aggravated due to injury or normal factors, it can lead to low back and leg pain. For example, a herniated disc in the lumbosacral area can cause nerve roots to send pain signals to the brain and cause abnormalities in the back and legs. (Aminoff & Goodin, 1988)
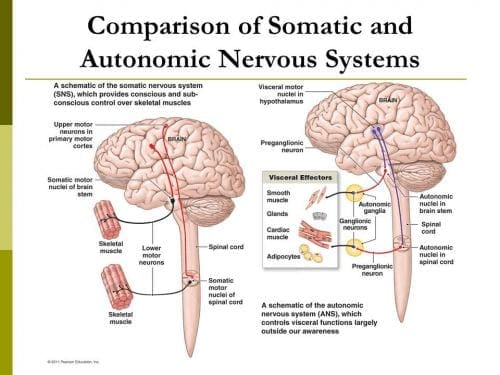
When people are dealing with back and leg pain from somatosensory pain, it can cause them to be miserable by reducing their quality of life and leading to a life of disability. (Rosenberger et al., 2020) At the same time, individuals dealing with somatosensory pain will also begin to feel inflammatory effects from the affected muscle area in the legs and back. Since inflammation is a body’s natural response when dealing with pain, the inflammatory cytokines can cause a cascading effect from the brain through the spinal cord, causing leg and back pain. (Matsuda, Huh, & Ji, 2019) To that point, somatosensory pain is associated with inflammation caused by normal or traumatic factors that can cause overlapping risk factors contributing to leg and back pain. Luckily, numerous treatments can reduce these overlapping risk factors caused by somatosensory pain and help restore the lower body extremities’ function.
Move Better, Live Better- Video

When the body is dealing with somatosensory pain, it can cause many individuals to think they are only dealing with one source of pain from one muscle area. Still, it can lead to multifactorial issues that affect different body locations. This is known as referred pain, where one body section deals with pain but is in a different area. Referred pain can also be combined with somato-visceral/visceral-somatic pain, where the affected muscle or organ affects one or the other, causing more pain-like issues. However, numerous treatments can reduce somatosensory pain from causing more leg and back problems. Non-surgical therapies like chiropractic care and spinal decompression can help mitigate the effects of somatosensory pain affecting the lower body extremities causing leg and back pain. These treatments allow the pain specialist to incorporate various therapeutic techniques to stretch the affected muscles and realign the spine to its original position. Many individuals can see an improvement in their mobility and daily activities as the pain-like symptoms associated with somatosensory pain are reduced. (Gose, Naguszewski, & Naguszewski, 1998) When individuals dealing with somatosensory pain start thinking about their health and wellness to ease the pain they are experiencing, they can look into non-surgical treatments as they are cost-effective, safe, and provide a positive outcome. Additionally, non-surgical treatments can be personalized to the individual’s pain and begin to see improvement after a few treatment sessions. (Saal & Saal, 1989) Check out the video above to learn more about how non-surgical treatments can be combined with other therapies to improve a person’s well-being.
Spinal Decompression Reduces Somatosenosory Pain
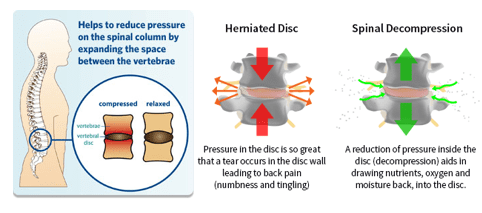
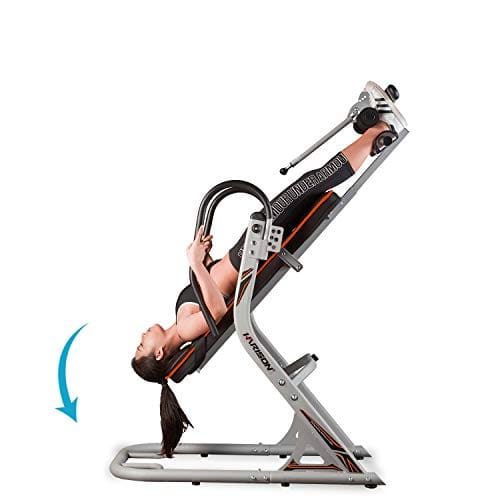
Now spinal decompression is a non-surgical treatment that can help reduce somatosensory pain affecting the legs and back. Since somatosensory pain correlates with the spinal cord, it can affect the lumbosacral spine and lead to back and leg pain. With spinal decompression, it utilizes gentle traction to gently pull the spine, which then can reduce the symptoms associated with somatosensory pain. Spinal decompression can help improve the somatosensory system by reducing pain and alleviating aggravated nerve root compression to relieve the legs and back. (Daniel, 2007)

Additionally, spinal decompression can be combined with other non-surgical treatments, like chiropractic, as it can help with reducing the effects of nerve entrapment and help restore the joint’s ROM (range of motion). (Kirkaldy-Willis & Cassidy, 1985) Spinal decompression can create a positive experience for many individuals dealing with leg and back pain associated with somatosensory pain while getting back their health and wellness.
References
Aminoff, M. J., & Goodin, D. S. (1988). Dermatomal somatosensory evoked potentials in lumbosacral root compression. J Neurol Neurosurg Psychiatry, 51(5), 740-742. https://doi.org/10.1136/jnnp.51.5.740-a
Daniel, D. M. (2007). Non-surgical spinal decompression therapy: does the scientific literature support efficacy claims made in the advertising media? Chiropr Osteopat, 15, 7. https://doi.org/10.1186/1746-1340-15-7
Finnerup, N. B., Kuner, R., & Jensen, T. S. (2021). Neuropathic Pain: From Mechanisms to Treatment. Physiol Rev, 101(1), 259-301. https://doi.org/10.1152/physrev.00045.2019
Gose, E. E., Naguszewski, W. K., & Naguszewski, R. K. (1998). Vertebral axial decompression therapy for pain associated with herniated or degenerated discs or facet syndrome: an outcome study. Neurol Res, 20(3), 186-190. https://doi.org/10.1080/01616412.1998.11740504
Kirkaldy-Willis, W. H., & Cassidy, J. D. (1985). Spinal manipulation in the treatment of low-back pain. Can Fam Physician, 31, 535-540. https://www.ncbi.nlm.nih.gov/pubmed/21274223
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2327983/pdf/canfamphys00205-0107.pdf
Matsuda, M., Huh, Y., & Ji, R. R. (2019). Roles of inflammation, neurogenic inflammation, and neuroinflammation in pain. J Anesth, 33(1), 131-139. https://doi.org/10.1007/s00540-018-2579-4
Rosenberger, D. C., Blechschmidt, V., Timmerman, H., Wolff, A., & Treede, R. D. (2020). Challenges of neuropathic pain: focus on diabetic neuropathy. J Neural Transm (Vienna), 127(4), 589-624. https://doi.org/10.1007/s00702-020-02145-7
Saal, J. A., & Saal, J. S. (1989). Nonoperative treatment of herniated lumbar intervertebral disc with radiculopathy. An outcome study. Spine (Phila Pa 1976), 14(4), 431-437. https://doi.org/10.1097/00007632-198904000-00018