Dr. Alex Jimenez, D.C., presents how hormonal dysfunction can be assessed and treated through various therapies specializing in hormones and how to regulate them in this 3 part series. This presentation will provide valuable information to many people dealing with hormonal dysfunction and how to utilize different holistic methods to optimize their health and wellness. Part 2 will look at the assessment for hormonal dysfunction. Part 3 will look at various treatments available for hormonal dysfunction. We refer patients to certified providers incorporating various hormone therapies to ensure optimal health and wellness. We encourage and appreciate each patient by referring them to associated medical providers based on their diagnosis when it is appropriate. We understand that education is an excellent way when asking our providers intricated questions at the patient’s request and understanding. Dr. Alex Jimenez, D.C., only utilizes this information as an educational service. Disclaimer
Table of Contents
What Are Hormones?
Dr. Alex Jimenez, D.C., presents: Today, we will look at utilizing foundational PTSD treatment strategy steps. As a treatment strategy, it is about the production, transportation, sensitivity, and detoxification of the hormone in PTSD. So let’s start with how interventions and major factors that influence these pathways within the access impact other body areas. How does an intervention on one hormone affect other hormones? So did you know that thyroid replacement can change the HPATG access in the body? So when people are dealing with hypothyroidism or subclinical hyperthyroidism and are being treated with suppressive thyroid hormone replacement, it induces changes in their bodies. This means they will become hypersensitive from ACTH to CRH or corticotropin-releasing hormone.
What this means is that they will produce and release more ACTH. When the patient becomes hypersensitive from an influx of hormones, it could lead to various issues with the other body systems that affect organ and muscle functionality. This is another reason patients feel great on even low doses of thyroid replacement; it stimulates the adrenals. Many patients tend to overrun their adrenals, and when they get treatment, they get a little hit to their adrenals when their doctors are helping their thyroid. So looking at the thyroid, we see the thyroid gland is producing t4, forming reverse T3 and t3. So when doctors look at the thyroid pharmacological doses of glucocorticoids, which is what they give for anti-inflammatory therapy to their patients, or if people have elevated glucocorticoids as in Cushing syndrome, what that does is it inhibit thyroid secretion because it reduces the TSH response to TRH, which makes less TSH. When there is less secretion in the thyroid can lead to overlapping issues associated with unnecessary weight gain, joint pain, and even metabolic syndrome.
To that point, stress inhibits the thyroid. In contrast, estrogens have the opposite effect, where they increase TSH secretion and the thyroid gland’s activity. So that’s a reason why women feel so much better on even low doses of estrogen replacement. So just like thyroid replacement in low amounts that bump the adrenals, if we’re giving low estrogen doses, it can bump up thyroid function. However, many doctors have to go slow when providing hormone treatments to patients because the additional hormones will affect the other hormones in the body. When it comes to hormone replacement therapy, it is important to learn how interventions within the communication node impact other nodes in the matrix. So, for example, let’s look at how the communication node affects the defense and repair node in the body. Research studies reveal HRT’s effects on inflammation markers and look at 271 women who used conjugated equine estrogen alone, who had a 121% increase in CRP after a year.
And if they used that in addition to synthetic progestin, they had a 150% increase in CRP after a year. So synthetic estrogen is not bioidentical; this is synthetic pregnant mare’s urine, and synthetic progestins are pro-inflammatory. What about the communication node and the assimilation node? This is an interesting study because many doctors are trying to help their patients and the future generation in society. So it’s important to know when the mother is stressed during pregnancy since that can change the baby’s microbiome. That means doctors have an opportunity to support early intervention in microbiome support. Knowing this is vital for prenatal stress based on questionnaires or elevated cortisol was strongly and persistently associated with infants’ microbiome and colonization patterns.
So we’re also here to learn how interventions on the matrix affect the hormone node or the communication node. So as an example, we’ll look at what happens in the assimilation node involving the communication node, as this affects antibiotics on the intestinal metabolome. Everyone knows about antibiotics’ impact on the microbiome, but a metabolome is a change in the metabolic function of a particular organ, the intestine. To that point, when there are so many metabolic pathways that antibiotics affect, the metabolism of steroid hormones was the most profoundly impacted. So eight metabolites that are part of this hormone pathway, which gives us PTSD, were increased in feces after antibiotic treatment. Then we have another way that the gut affects hormones, and this is looking at metabolic endotoxemia. Many doctors learn about metabolic endotoxemia in AFMCP, which mentions leaky gut or increased intestinal permeability. When many individuals are dealing with gut issues affecting their well-being, like problems in their joints or muscles causing them pain, we provide various solutions and develop a treatment plan with our associated providers based on the diagnosis.
Endotoxins Affecting Hormones
Dr. Alex Jimenez, D.C., presents: Endotoxins or lipopolysaccharides are from the cell membranes of bacteria. So bacterial endotoxins are translocated from the gut lumen because of increased intestinal permeability. So with that increased permeability, those endotoxins are translocated, which starts an inflammatory cascade. When endotoxins cause GI issues, the inflammatory markers can affect the upper and lower portions of the body and the gut-brain axis. When the gut-brain axis is affected by inflammation, it could lead to joint and muscle pain associated with somato-visceral and visceral-somatic problems. To that point, the inflammatory cascade from the leaky gut affects the ovary, reduces progesterone production, and contributes to luteal phase deficiency. That’s incredibly important for doctors to take care of patients that are there to optimize fertility. It is especially important for patients to let their doctors know when they have excess estrogen and that they are producing as much progesterone as possible. So we must worry about gut permeability in ovulation, luteal phase deficiency, and estrogen-progesterone imbalance. What about the biotransformation node? How does that affect the communication node? In preschool children, phthalates and thyroid function have an inverse association between the metabolites or the amount of folate and thyroid function in the system measured in children at age three. When inflammatory issues affect thyroid function in children, it can affect cognitive outcomes, thus reducing phthalates production in the thyroid, leading to mental problems.
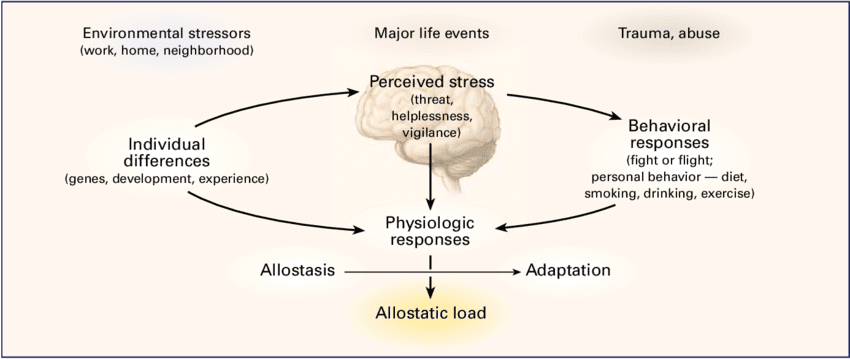
How do mental, emotional, and spiritual considerations contribute to the communication node? We want to start with the bottom of the matrix like we always do, which involves functional medicine. Functional medicine provides holistic approaches to identifying the root problem affecting the body and developing a personalized treatment plan for the patient. By looking at the lifestyle factors at the bottom of the Living Matrix, we can see how hormone dysfunction affects the communication nodes in the body. A recent paper found that there was a positive relationship between menopausal symptoms and social support and that menopausal symptom decrease as social support increases. Now let’s talk about how stress impacts HPA access. By looking at how stimulation from the sex hormone-producing parts of the body or the goads, the thyroid access, the adrenals, and the sympathetic nervous system (fight or flight) can add up all the stressors affecting us, called allostatic load.
And allostasis refers to our ability to respond to those stressors through stress-coping mechanisms. Many patients are asking us for guidance. They’re asking how they can frame their personal experiences and stressors. Still, they’re also asking how they prepare the societal events in a larger context, And many of us as functional medicine practitioners are seeking the same thing. And so, we’re going to show you in detail what stress does to the body and how to find ways of decreasing anxiety or stress in the body to prevent future issues in the organs, muscles, and joints.
How Stress Inhibits Estrogen
Dr. Alex Jimenez, D.C., presents: Does stress creates adrenal stress, and does it affect our fight or flight primary response hormone (adrenaline)? Stress can cause the sympathetic nervous system to increase blood pressure, respiration, heart rate, and general alertness while redirecting our blood to increase our adrenaline. So when you are in a situation, your adrenaline can cause you to fight or run, which causes your muscles to get blood, which decreases blood to your core or your non-essential organs. So the functional medicine model would identify various triggers or mediators, whether acute or chronic, that can act as an instigator of hormone dysfunction that can create overlapping issues that can disrupt adrenal function in the thyroid.
So, looking at these responses can help us see the physical problems that are happening if adrenaline is chronically increased over the long term, leading to anxiety, digestion problems, et cetera. Now cortisol is our vigilance hormone that helps maintain the emergency response to back up or support the adrenaline. An example would be a fire truck or police that come in after the immediate first responder. So cortisol facilitates the quick adrenaline response to keep the body going as needed. And it has many other roles as well. It helps with increased blood sugar and causes fat storage. So when people come in with weight around the middle and dealing with overlapping issues in their body, think of cortisol since it’s anti-inflammatory and regulates the nervous system. Cortisol can be both good and bad for the body, especially when an individual is dealing with stressful events affecting their health and causing issues affecting their mobility.
So now, let’s talk about how stress impacts the entire body and the immune system. Stress can increase susceptibility to infections, increasing their severity in the body. So here we see stress affecting the defense and repair node, leading to immune dysfunction and stress-induced immune dysfunction. An example would be if a person is dealing with a disorder that affects their gut, like SIBO or leaky gut; it can increase the production of pro-inflammatory cytokines and causes joint and muscle pain to the lower back, the hips, the knees, and overall wellness. When the pro-inflammatory cytokines affect the gut system, they can also cause thyroid dysfunction, disrupting hormone production.

So if someone’s taking that hormone replacement therapy (HRT), it can increase their inflammation, especially if they are stressed. So, as functional medicine practitioners, we’re always thinking and looking for pattern recognition as we start thinking about things differently from conventional methods regarding health and wellness.
What is it when you see a person dealing with chronic stress, and what is their response? They will usually answer, “I sweat a lot; I get nervous and anxious just remembering what has happened to me. I’m afraid of experiencing that ever again. Sometimes these pathways give me nightmares. Whenever I hear a loud noise, I think of carbon rings and get nauseous.” These are some tell-tale signs of someone dealing with chronic stress associated with PTSD, which can affect the hormone levels in the body. Many functional medicine providers can utilize available treatment regarding hormonal dysfunction in PTSD. So the general strategy for treating hormone dysfunction is the production, transport sensitivity, and detoxification of hormones in the body. Remember that when you have someone dealing with hormonal issues, it is best to devise a strategy to deal with this issue.
So what can we do to affect how hormones are produced or have been over-produced in the body? We want to look at how hormones are made, how they may be secreted within the body, and how they’re transported. Because what if they’re transported in a way that the transport molecule is low in concentration, allowing them to be free hormones? So that’s the interaction with other hormone sensitivity, and how do we change or look at cellular sensitivity to the hormonal signal? For example, progesterone affects estrogen receptors which cause detoxification or excretion of the hormone.
So before we think about giving or replacing a hormone, we ask what we can do to affect that hormone in the body. Specifically, how can we influence the hormone’s production, transport, sensitivity, detoxification, or elimination? So when it comes to hormone production, what are the building blocks for thyroid hormones and cortisol? So if we’re low on thyroid hormones, we want to ensure that we have the building blocks of serotonin. So what affects synthesis? If a gland is inflamed with autoimmune thyroiditis, it may not be able to make enough thyroid hormone. And that’s why people with autoimmune thyroiditis have low thyroid function. What about hormone transportation? Do the levels of one hormone in the body impact the levels of another? Estrogen and progesterone are often in a dance in the body. So does a hormone transport from the origin glands to the target tissue, which can impact its effectiveness?
If there is an overproduction of hormones attached to the transport protein, there won’t be enough free hormone, and there can be hormone deficiency symptoms. Or it can be the opposite if there needs to be more transport protein, then there will be too many free hormone molecules and hormone excess symptoms. Therefore, we want to know if we can impact the free hormone level and see if it is transformed. So we know that T4 becomes the active form of T3 or a thyroid inhibitor, reverse t3, and can we modulate those pathways? What about sensitivity? Are nutritional or dietary factors influencing the cellular response to cortisol, thyroid hormones, testosterone, estrogen, et cetera? With many cell membrane binding proteins, the cell membrane is involved in hormone metabolism. And if the cell membranes are rigid, insulin, for example, has a hard time getting in it now as we look into hormone detoxification. How do we alter the metabolism of estrogens or testosterone?
And what can we do to affect estrogen’s binding and excretion? So, can estrogen have to be eliminated healthily? And that depends on whether there’s hydroxylation on a particular carbon, but it also has to be excreted in terms of total amounts. So constipation, for example, will decrease the quantity of estrogen excreted. So we use the vault as a metaphor and the theme, as we said, is to treat the matrix first before directly addressing hormone dysfunction.
Cortisol Affecting The Communication Nodes
Dr. Alex Jimenez, D.C., presents: In the Living Matrix, we have to unlock or treat all the nodes to open the vault to get inside and address hormones. This is because the endocrine system is so complex it often self-corrects when other imbalances are addressed. And remember, hormonal imbalance is often an appropriate response by the body to imbalances elsewhere. That’s why treating other imbalances often addresses the hormonal issue. And also, remember hormones like picograms are in very low concentrations. So it’s very hard to be precise when we give patients hormones and allow the body to auto-correct. That’s why we say to treat the matrix first. And when we get inside the communication node in the body, we look at the center of the matrix and discover the body’s emotional, mental, and spiritual functions to help normalize hormones. And while these are addressed, how can we fix the hormonal communication nodes?
When inside the communication node, the treatment must follow an order: adrenal, thyroid, and sex steroids. So these are important concepts to remember, treat adrenals, thyroid, and finally, sex steroids. And the way we depict the pathways will be consistent. So here you see the standard representation we will use for the steroidogenic path. And you see all of the different hormones here. The enzymes in the steroidogenic pathway are color-coded, so many doctors can know which enzyme affects which step. Next, we will look at the modulation of the steroid pathways through lifestyle, like exercise, and how stress affects aromatase, making estrogen.
Now, as we get into the real, heavy part here about the steroid pathways, we inform many of our patients to take a deep breath as it shows that taking a deep breath can increase a person’s cognition and provide the ability to understand everything. So the big picture here is everything starts with cholesterol and how it affects the hormones in the body. So cholesterol forms the mineral corticoid aldosterone, which then develops cortisol, ultimately creating androgens and estrogens. When patients are given consultation on what is going on with their bodies, many don’t realize that high cholesterol could potentially lead to chronic stress, which is associated with cardiovascular issues that can ultimately invoke visceral-somatic disorders.
Inflammation, Insulin, & Cortisol Affecting Hormones
Dr. Alex Jimenez, D.C., presents: When a female patient is dealing with fibroids or endometriosis, many doctors devise a treatment plan with other medical providers to reduce the formation of the estrogen hormones by inhibiting and modulating the aromatase enzymes. This allows the patient to make small changes to their lifestyle habits by ensuring their zinc levels are normal, not drinking alcoholic beverages constantly, finding ways to reduce their stress levels, and normalizing their insulin intake. Each treatment plan caters to the individual as they find ways to reduce their cortisol levels and regulate healthy hormone production. This will allow the body to increase estrogen production while decreasing the aromatase. So when we are discussing stress, it can negatively impact the hormone pathways directly by increasing cortisol, thus causing the pituitary glands to increase the CTH when stress is responding to the body. Many individuals are dealing with chronic stress in their bodies, which can cause overlapping risk profiles to the musculoskeletal system, causing muscle and joint pain.
So the pituitary system produces cortisol when the body calls for it directly when the individual is dealing with acute stress. However, chronic stress can indirectly increase cortisol levels; it causes the enzyme 1720 lyase to be inhibited in the body, causing a decrease in anabolism, thus slowing down the body’s energy levels. So stress inhibits this enzyme. So when stress inhibits the 1720 lyase enzyme in the body, it can cause the pituitary system to produce more cortisol and cause more issues like joint to affect the individual. So those are the two ways that stress leads to more cortisol directly through ACTH and indirectly by inhibiting 1720 lyase.

Inflammation is important in the body as it also has a two-way path, as it can impact these pathways the same way stress does. Inflammation can inhibit the 1720 lyase enzyme, causing the body to be pro-inflammatory and can stimulate aromatase. Like stress, when the body is dealing with inflammation, the pro-inflammatory cytokines stimulate aromatase enzymes to cause an increase in estrogen formation. When this happens, it allows the doctors to notice why their patients are overly stressed and have inflammatory markers in their gut, muscles, and joints. To that point, inflammation can also increase an enzyme called 5alpha reductase. Now, 5alpha reductase causes the formation of a hormone called dihydrotestosterone (the active form of testosterone in the body cells other than the muscles, causing hair loss. So insulin, stress, and inflammation contribute to hair loss because insulin has the same effect. Insulin or blood sugar gives the body energy to move throughout the day. When individuals have too much or too little insulin in the body, it can lead to insulin resistance, correlating to metabolic syndrome associated with hair loss.
Holistic Methods For Hormones
Dr. Alex Jimenez, D.C., presents: How do insulin, cortisol, and inflammation play their part in the thyroid? Well, all of these hormones help make the body functional. When the thyroid has an underlying condition like hypo or hyperthyroidism, it can cause the body to over or underproduce hormones to regulate healthy normal body functions. So this forward feed cycle can cause the individual to have various issues affecting their body due to hormonal dysfunction. This combination of insulin resistance, high insulin, weight gain, and stress affects many patients, causing metabolic syndrome. To normalize hormonal function, we must look at all these factors driving hormonal dysfunction in patients.
When going for hormonal treatment, it is important to know about the different nutraceuticals and botanicals because before, it was called a lifestyle change back in the day. In a health clinic, specific neutraceuticals and botanicals can affect estrogen formation through the enzyme aromatase. However, various factors like diseases, medications, toxins, and elevated insulin can also increase aromatase enzymes, leading to more estrogen in the body. And then diseases, medications, and toxins do the same thing. A research study reveals that when men and women interact, the men’s cognitive performance declines, followed up with a mix-sex encounter. This can change how hormone function in the body when there are changes in formal function that can affect the central nervous system’s cognitive function in the body.
When middle age patients get examined by their doctors, the results can show if they have elevated insulin, an increase in stress and if there is inflammation in their bodies. This allows the doctors to work with associated specialists to develop a treatment plan that caters to the patient to begin small changes in their health and wellness journey.
Disclaimer
Professional Scope of Practice *
The information herein on "Dr. Alex Jimenez Presents: Assessing & Treating Hormonal Dysfunction" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Our information scope is limited to Chiropractic, musculoskeletal, physical medicines, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somatovisceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and/or functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez, DC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, RN*, CCST, IFMCP*, CIFM*, ATN*
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807, New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Florida
Florida License RN License # RN9617241 (Control No. 3558029)
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Presently Matriculated: ICHS: MSN* FNP (Family Nurse Practitioner Program)
Dr. Alex Jimenez DC, MSACP, RN* CIFM*, IFMCP*, ATN*, CCST
My Digital Business Card