“For individuals with aches and pains throughout their body, can a foot detox help bring relief?”

Table of Contents
Foot Detox
A foot detox involves soaking the feet in an ionic bath to help remove toxins from the body. They can also be performed using acupressure, scrubs, foot masks, and pads. Combined with eliminating toxins, detox is also believed to help enhance blood circulation and provide body pain and discomfort relief. However, current evidence is limited and there has been no evidence to support that toxins can be released from the feet using an ionic bath. However, they have been found to provide other benefits, which include:
- Relaxation
- Lower stress levels
- Enhanced skin health and hydration.
- Reduced inflammation in individuals with skin disorders.
Foot detoxes are considered generally safe, but individuals are recommended to speak to their healthcare provider.
Potential Benefits
The potential health benefits include:
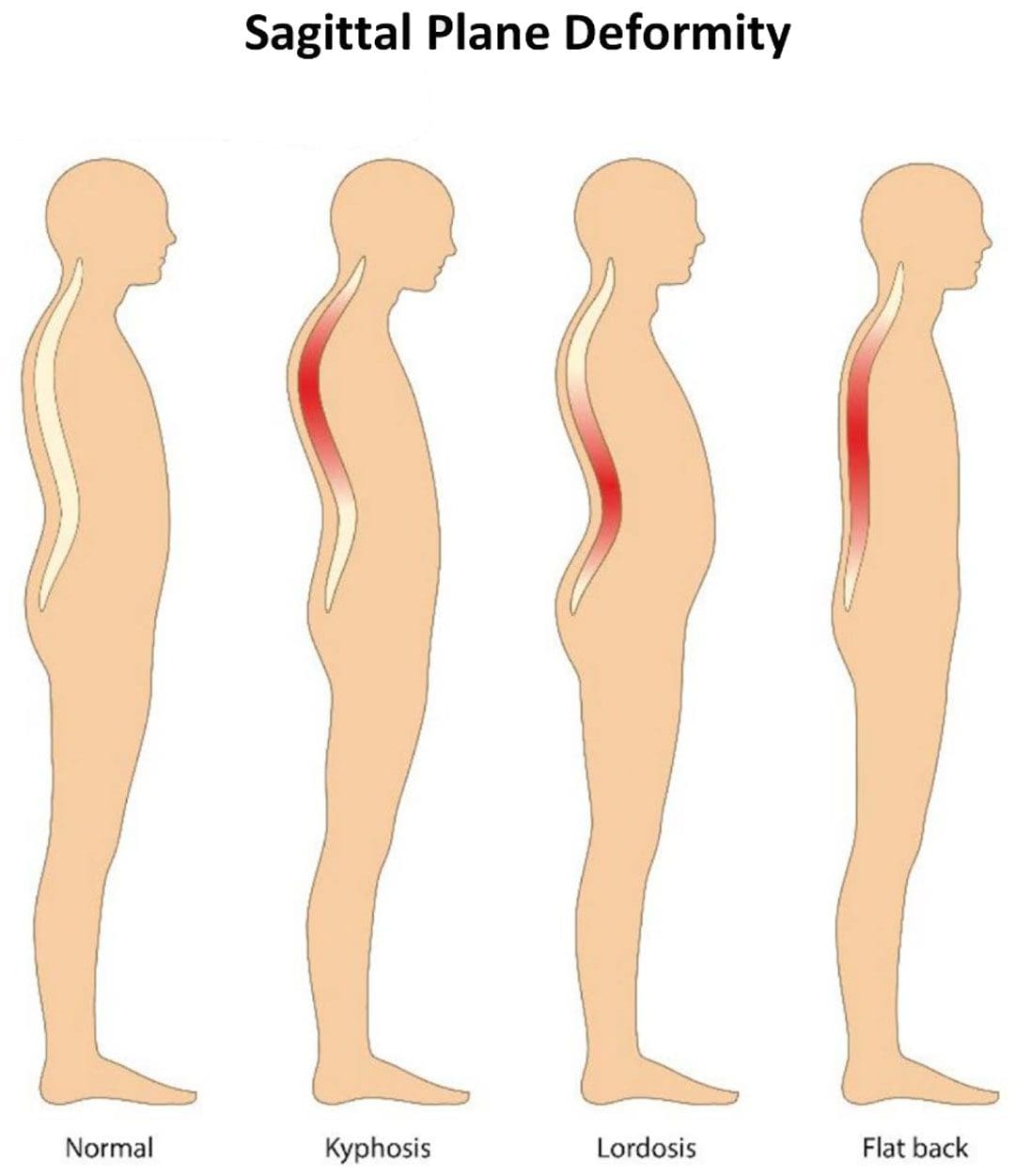
- Reduces inflammation and swelling.
- Improves stress levels and mood.
- Can help with weight management.
- Can help with heart health and increased blood circulation.
- Relieves aches and pains.
- Balances pH levels.
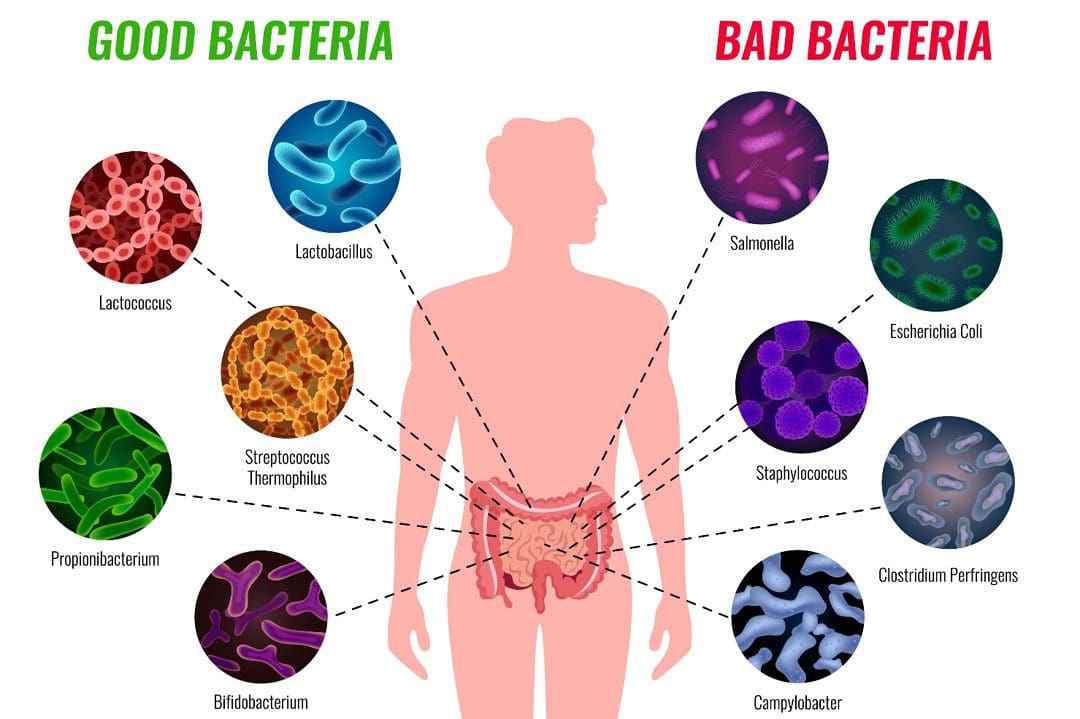
- Eliminate harmful pathogens and microorganisms.
However, most reports surrounding the benefits of foot detox are not proven by research investigating whether the health claims are scientifically accurate. One study in 2012 found that foot detoxes did not produce the intended results and could not help remove toxins from the body. (Deborah A. Kennedy, et al., 2012) Other research surrounding foot baths and massages showed that they could help reduce symptoms of mood disorders like schizophrenia because of the relaxing effect they produce. (Kazuko Kito, Keiko Suzuki. 2016)
Ways Toxins are Removed From the Body
Toxins are filtered out of the body in a variety of ways. Breathing out expels carbon dioxide from the body. Another way is through the body’s natural processes. The body has organs and other systems to filter out and release toxins.
- Specific organs, such as the liver, kidneys, and lymph nodes, filter and remove harmful and unneeded substances. (UW Integrative Health. 2021)
- The health claims surrounding toxin removal through the feet are currently insubstantial because no evidence supports the effectiveness and the anecdotal evidence is not based on science.
- Water tested after foot detoxes did not detect any toxins. (Deborah A. Kennedy, et al., 2012)
Types
Foot detoxes can be an enjoyable experience that can help relieve sore feet, relax the body, and offer relief for certain foot ailments. They could be an excellent addition to a self-care routine. Some of the most commonly used natural foot detoxes include the following.
Epsom Salt Foot Bath
- Combining Epsom salts with warm water and soaking the feet for 20–30 minutes can help promote relaxation.
- Research has shown that Epsom salts may help reduce pain associated with diabetic neuropathy and fatigue associated with chemotherapy. (Ferda Akyuz Ozdemir, Gulbeyaz Can. 2021) (Seyed Reza Vakilinia, et al., 2020)
Apple Cider Vinegar
- Apple cider vinegar foot baths are made by diluting 1 cup of vinegar in warm water and soaking the feet for 20–30 minutes.
- There is limited research available to confirm the health claims.
- The studies that have been done have found the reverse effect, that bathing the feet in apple cider vinegar and water can irritate the skin. (Lydia A Luu, et al., 2021)
Baking Soda and Sea Salt
Sea salt combined with baking soda dissolved in a bath and soak the feet for up to 30 minutes. While research is limited, some evidence supports the health benefits associated with sea salt that include: (Ehrhardt Proksch, et al., 2005)
- Enhances skin hydration.
- Improve skin barrier function. (Kanwar A. J. 2018)
- Reduces inflammation in skin conditions, like atopic dermatitis.
Foot baths should be avoided for the following:
- There are open sores on the feet that could be irritated by salt and other foot bath ingredients.
- Individuals with a pacemaker or any electrical body implant.
- Pregnant women.
- Consult a healthcare provider before trying any new health protocols.
Foot Orthotics Benefits
References
Kennedy, D. A., Cooley, K., Einarson, T. R., & Seely, D. (2012). Objective assessment of an ionic footbath (IonCleanse): testing its ability to remove potentially toxic elements from the body. Journal of environmental and public health, 2012, 258968. https://doi.org/10.1155/2012/258968
Kito, K., & Suzuki, K. (2016). Research on the Effect of the Foot Bath and Foot Massage on Residual Schizophrenia Patients. Archives of psychiatric nursing, 30(3), 375–381. https://doi.org/10.1016/j.apnu.2016.01.002
UW Integrative Health. Improving your health by removing toxins from your body.
Akyuz Ozdemir, F., & Can, G. (2021). The effect of warm salt water foot bath on the management of chemotherapy-induced fatigue. European journal of oncology nursing: the official journal of European Oncology Nursing Society, 52, 101954. https://doi.org/10.1016/j.ejon.2021.101954
Vakilinia, S. R., Vaghasloo, M. A., Aliasl, F., Mohammadbeigi, A., Bitarafan, B., Etripoor, G., & Asghari, M. (2020). Evaluation of the efficacy of warm salt water foot-bath on patients with painful diabetic peripheral neuropathy: A randomized clinical trial. Complementary therapies in medicine, 49, 102325. https://doi.org/10.1016/j.ctim.2020.102325
Luu, L. A., Flowers, R. H., Gao, Y., Wu, M., Gasperino, S., Kellams, A. L., Preston, D. C., Zlotoff, B. J., Wisniewski, J. A., & Zeichner, S. L. (2021). Apple cider vinegar soaks do not alter the skin bacterial microbiome in atopic dermatitis. PloS one, 16(6), e0252272. https://doi.org/10.1371/journal.pone.0252272
Proksch, E., Nissen, H. P., Bremgartner, M., & Urquhart, C. (2005). Bathing in a magnesium-rich Dead Sea salt solution improves skin barrier function, enhances skin hydration, and reduces inflammation in atopic dry skin. International journal of dermatology, 44(2), 151–157. https://doi.org/10.1111/j.1365-4632.2005.02079.x
Kanwar A. J. (2018). Skin barrier function. The Indian Journal of Medical Research, 147(1), 117–118. https://doi.org/10.4103/0971-5916.232013