Learn the benefits of garlic as an anti-inflammatory remedy for musculoskeletal pain and enhance your wellness routine.
Table of Contents
Holistic Healing for Lower Back and Leg Pain: Chiropractic Care and Anti-Inflammatory Diets
Lower back and leg pain, often radiating from the lumbar spine through the buttocks and down to the feet, can disrupt daily life, making simple tasks like sitting, standing, or walking feel unbearable. This type of pain, commonly associated with sciatic nerve irritation, affects a large number of individuals, resulting in discomfort ranging from mild aches to sharp, electric-shock-like sensations. While medications or surgery may be considered, nonsurgical approaches like chiropractic care paired with an anti-inflammatory diet provide a natural, effective way to manage and reduce this pain. This comprehensive, SEO-optimized article explores the clinical rationale for combining chiropractic care with an anti-inflammatory diet, the role of foods like garlic in reducing inflammation and boosting immune health, and the factors contributing to lower back and leg pain. Drawing insights from clinical research and Dr. Alexander Jimenez, DC, APRN, FNP-BC, a board-certified chiropractor and family nurse practitioner in El Paso, Texas, we’ll also highlight how integrative, nonsurgical treatments promote the body’s natural healing process, prevent long-term issues, and emphasize clear patient communication.
Understanding Lower Back and Leg Pain: Causes and Contributing Factors
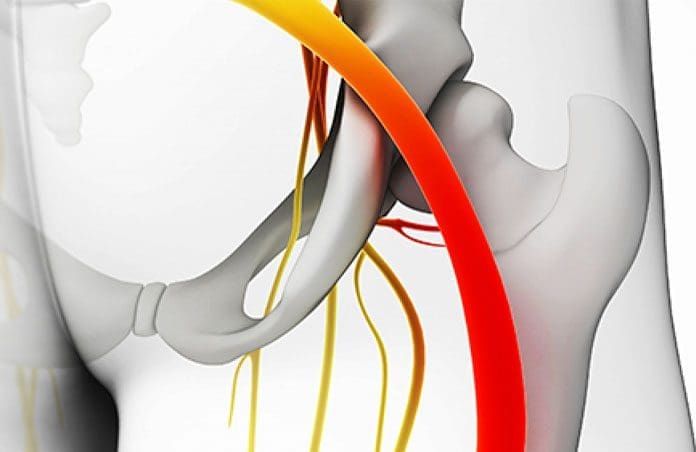
Lower back and leg pain often results from irritation or compression of the sciatic nerve, the body’s longest nerve, which originates in the lumbar spine, extends through the buttocks, and travels down the legs to the feet. Identifying the root causes and contributing factors is essential for effective treatment and prevention.
Common Causes of Lower Back and Leg Pain
- Herniated or Bulging Discs: A herniated or bulging disc in the lumbar spine can press against the sciatic nerve roots, causing pain that radiates down the leg. This is one of the most common triggers, often resulting from wear and tear, injury, or poor posture.
- Spinal Misalignments (Subluxations): Misaligned vertebrae, caused by poor posture, pregnancy, or trauma, can irritate the sciatic nerve, leading to pain, numbness, or tingling. These misalignments may develop gradually before symptoms become noticeable.
- Bone Spurs: Overgrowth of bone on the vertebrae, often due to aging or osteoarthritis, can compress the sciatic nerve, causing discomfort that extends from the lower back to the legs.
- Muscle Strain or Spasms: Overuse, repetitive motions, or sudden injuries can strain muscles in the lower back or buttocks, contributing to nerve irritation and pain.
- Trauma or Accidents: Injuries from motor vehicle accidents, falls, or sports can cause structural damage to the spine or surrounding tissues, leading to sciatic nerve compression.
- Rare Causes: In uncommon cases, tumors or conditions like diabetes can damage or compress the sciatic nerve, resulting in pain and other symptoms.
Risk Factors
Several factors increase the likelihood of developing lower back and leg pain:
- Age: Age-related changes, such as disc degeneration or bone spurs, are common causes of sciatic nerve irritation.
- Obesity: Excess body weight increases stress on the spine, contributing to conditions that trigger pain.
- Sedentary Lifestyle: Prolonged sitting or lack of physical activity weakens muscles and reduces spinal flexibility, increasing pain risk.
- Occupation: Jobs involving repetitive twisting, heavy lifting, or long periods of driving may contribute to nerve irritation, though evidence is inconclusive.
- Diabetes: This condition can damage nerves, including the sciatic nerve, heightening the risk of pain.
- Poor Posture: Incorrect posture during sitting or standing can strain the spine, leading to misalignments and nerve compression.
Understanding these causes and risk factors allows for targeted interventions that address both symptoms and underlying issues, promoting lasting relief.
The Clinical Rationale for Chiropractic Care and Anti-Inflammatory Diets
Chiropractic care and anti-inflammatory diets work synergistically to address the biomechanical and inflammatory components of lower back and leg pain. Below, we explore the clinical rationale for this integrative approach, supported by research and insights from Dr. Alexander Jimenez.
Chiropractic Care: A Nonsurgical Path to Relief
Chiropractic care focuses on diagnosing and treating musculoskeletal issues, particularly spinal misalignments and joint dysfunctions that contribute to nerve irritation. Dr. Alexander Jimenez, with over 30 years of experience in El Paso, Texas, emphasizes a holistic approach that uses spinal adjustments, advanced diagnostics, and patient-centered care to alleviate pain and restore mobility (Jimenez, 2025).
How Chiropractic Care Works
Chiropractic adjustments involve gentle, precise manipulations to correct spinal misalignments and relieve pressure on the sciatic nerve. This approach can:
- Reduce Nerve Irritation: Realigning the spine alleviates pressure on the sciatic nerve, reducing pain, numbness, and tingling.
- Decrease Inflammation: By correcting misalignments, chiropractic care helps reduce tissue irritation, thereby promoting the body’s natural anti-inflammatory response.
- Restore Mobility: Adjustments improve joint function, allowing patients to move more freely without discomfort.
- Support Natural Healing: Enhanced circulation from proper alignment delivers oxygen and nutrients to affected tissues, aiding recovery.
Evidence Supporting Chiropractic Care
Research supports chiropractic care’s effectiveness for lower back and leg pain. A study in Nutrients found that chiropractic interventions, combined with dietary changes, significantly reduced chronic pain by addressing biomechanical and inflammatory factors (Dragan et al., 2020). Dr. Jimenez’s practice aligns with these findings, utilizing advanced imaging techniques such as MRI and X-rays to pinpoint the source of pain and tailor treatments to each patient’s specific needs (Jimenez, 2025). Patients often report improved overall health and reduced reliance on pain medications after chiropractic care.
Dr. Jimenez emphasizes that chiropractic care is about more than adjustments: “We assess the whole patient—biomechanics, lifestyle, and health goals—to create a personalized plan that promotes healing, not just symptom relief” (Jimenez, 2025).
The Role of Anti-Inflammatory Diets in Pain Management
An anti-inflammatory diet targets systemic inflammation, a key contributor to lower back and leg pain, by incorporating nutrient-rich foods that combat inflammation at the cellular level. This dietary approach complements chiropractic care by enhancing the body’s ability to heal.
How Anti-Inflammatory Diets Work
Chronic inflammation, often exacerbated by poor diet or stress, damages tissues and amplifies pain. Anti-inflammatory diets focus on:
- Whole Foods: Fruits, vegetables, whole grains, and lean proteins provide antioxidants and nutrients that reduce inflammation.
- Healthy Fats: Omega-3 fatty acids, found in fish, nuts, and seeds, lower inflammatory markers like C-reactive protein (CRP).
- Anti-Inflammatory Spices: Garlic, turmeric, and ginger contain bioactive compounds that inhibit inflammation.
- Avoiding Pro-Inflammatory Foods: Limiting processed foods, refined sugars, and trans fats reduces inflammation.
A pilot study in Frontiers in Nutrition showed that an anti-inflammatory Mediterranean-based diet (AnMeD-S) improved pain, stress, and sleep quality in patients with chronic pain (Sala-Climent et al., 2023). Increased intake of anti-inflammatory foods correlated with better quality of life, highlighting the diet’s role in pain management.
Synergy with Chiropractic Care
The combination of chiropractic care and an anti-inflammatory diet creates a powerful synergy:
- Chiropractic care corrects structural issues, such as spinal misalignments or disc compression, that cause nerve irritation.
- Anti-inflammatory diets reduce systemic inflammation, easing the inflammatory load on nerves and tissues, which enhances the effectiveness of adjustments.
- Together, they promote long-term healing by addressing both the mechanical and biochemical aspects of pain, thereby reducing the risk of recurrence.
Dr. Jimenez advocates for this integrative approach: “Chiropractic care restores alignment, while an anti-inflammatory diet provides the nutritional foundation for healing and resilience” (Jimenez, 2025).
Fighting Inflammation Naturally- Video

Garlic: A Potent Anti-Inflammatory Ally
Garlic (Allium sativum) is a standout ingredient in anti-inflammatory diets due to its bioactive compounds, affordability, and versatility. Dr. Jimenez highlights garlic’s potential in his wellness blog, noting its role in reducing inflammation and supporting overall health (El Paso Back Clinic, 2025).
Nutritional Facts and Benefits of Garlic
A single clove (approximately 3 grams) of raw garlic contains:
- Calories: 4.5 kcal
- Carbohydrates: 1 gram
- Protein: 0.2 grams
- Fiber: 0.1 grams
- Vitamins and Minerals: Vitamin C, vitamin B6, manganese, and calcium
- Bioactive Compounds: Allicin, diallyl disulfide, and S-allyl cysteine, which drive garlic’s medicinal properties
Key Health Benefits
- Anti-Inflammatory Effects: Garlic’s organosulfur compounds, like allicin, inhibit pro-inflammatory pathways, reducing markers like CRP. A systematic review in Critical Reviews in Food Science and Nutrition found that garlic supplementation improved cardiovascular parameters and reduced inflammation, which can alleviate pain (Imaizumi et al., 2023).
- Antioxidant Properties: Garlic neutralizes free radicals, reducing oxidative stress that contributes to tissue damage and pain (Quesada et al., 2020).
- Immune System Support: Garlic enhances immune cell activity, helping the body combat inflammation and infections that exacerbate pain (Tattelman, 2005).
- Cardiovascular Health: By lowering blood pressure and cholesterol, garlic reduces stress on the musculoskeletal system, particularly in weight-bearing areas (Imaizumi et al., 2023).
- Metabolic Benefits: Garlic may improve insulin sensitivity and reduce body fat, addressing risk factors like obesity and diabetes that contribute to nerve pain (Liu et al., 2007; Pérez-Rubio et al., 2022).
Garlic and Lower Back and Leg Pain
Garlic’s anti-inflammatory and immune-boosting properties make it a valuable tool for managing lower back and leg pain. It can:
- Reduce Nerve Inflammation: Lowering inflammation around the sciatic nerve alleviates pain and discomfort.
- Support Muscle Recovery: Garlic’s antioxidants reduce muscle soreness and tension, which often accompany nerve irritation.
- Enhance Joint Health: By reducing inflammatory markers, garlic supports conditions like osteoarthritis that may contribute to spinal pain.
Dr. Jimenez shares his experience: “I incorporate a clove of garlic daily—chopped, rested to activate allicin, and swallowed with water. It’s a simple, cost-effective way to boost my health and energy” (El Paso Back Clinic, 2025).
Preparation Tips for Maximum Benefits
- Rest After Chopping: Let chopped or crushed garlic sit for 5–10 minutes to activate allicin, its key anti-inflammatory compound.
- Minimize Overheating: Add garlic late in cooking to preserve its bioactive properties.
- Use Regularly: Incorporate garlic into meals like soups, stir-fries, or sauces for consistent benefits.
Dr. Jimenez’s “Spaghetti, Oil, and Garlic” recipe combines garlic with olive oil, another anti-inflammatory ingredient, to create a flavorful, health-supporting dish (El Paso Back Clinic, 2025).
Nonsurgical Treatments: A Comprehensive Approach
In addition to chiropractic care and dietary interventions, other nonsurgical therapies enhance pain relief and promote healing. These integrative approaches address both physical and biochemical aspects of lower back and leg pain.
Targeted Exercises
Exercise is vital for managing nerve-related pain. Specific exercises can:
- Strengthen Core Muscles: Strong abdominal and lower back muscles support the spine, reducing nerve pressure.
- Improve Flexibility: Stretching enhances range of motion, preventing stiffness and further irritation.
- Reduce Inflammation: Low-impact activities like walking or yoga improve circulation, lowering inflammatory markers.
Dr. Jimenez tailors exercise plans to each patient’s condition, noting, “Exercise restores balance and function, not just strength, to help patients move pain-free” (Jimenez, 2025).
Massage Therapy
Massage therapy relieves muscle tension, improves blood flow, and reduces stress, all of which alleviate nerve pain. A study in Nutrients found that massage, combined with dietary interventions, improved outcomes in chronic pain patients (Dragan et al., 2020).
Acupuncture
Acupuncture uses thin needles to stimulate specific points, balancing energy flow and reducing pain. Research suggests it can modulate pain signals and reduce inflammation, complementing chiropractic care (Sala-Climent et al., 2023).
Integrative Medicine
Integrative medicine combines conventional and complementary therapies to treat the whole person. Key components include:
- Patient Education: Clear communication empowers patients to understand their condition and treatment plan.
- Holistic Care: Addressing diet, stress, and sleep enhances outcomes.
- Prevention: Targeting underlying causes reduces the risk of chronic pain or disability.
Dr. Jimenez’s practice exemplifies this approach, blending chiropractic care, nutritional counseling, and lifestyle interventions to optimize recovery (Jimenez, 2025).
Preventing Long-Term Complications
Nonsurgical treatments focus on preventing chronic pain and long-term issues by addressing root causes. Benefits include:
- Reduced Medication Use: Natural approaches minimize reliance on pain medications, avoiding side effects like dependency.
- Preventing Chronicity: Early intervention stops acute pain from becoming chronic.
- Improved Quality of Life: Reduced pain and improved mobility allow patients to enjoy daily activities.
Research in the Journal of Medicinal Food highlights that dietary interventions, including garlic, can prevent metabolic diseases that contribute to nerve pain (Pérez-Rubio et al., 2022). Chiropractic care further supports prevention by maintaining spinal health (Jimenez, 2025).
The Power of Clear Communication
Effective communication between providers and patients is crucial for successful outcomes. Dr. Jimenez emphasizes building trust: “We explain how chiropractic care, diet, and lifestyle changes work together to relieve pain and promote healing, empowering patients to take charge of their recovery” (Jimenez, 2025).
Conclusion
Lower back and leg pain, often linked to sciatic nerve irritation, can significantly impact daily life. Combining chiropractic care with an anti-inflammatory diet offers a natural, effective solution by addressing biomechanical and inflammatory causes. Chiropractic adjustments restore alignment, while foods like garlic reduce inflammation and support immune health. Complementary therapies, such as exercise, massage, and acupuncture, further enhance recovery. By focusing on prevention and clear communication, this integrative approach promotes lasting relief and improved well-being.
For expert care, Dr. Alexander Jimenez, DC, APRN, FNP-BC, offers personalized treatment plans at his El Paso clinic, blending chiropractic expertise with nutritional and lifestyle guidance. Learn more at dralexjimenez.com or connect on LinkedIn.
References
- Dragan, S., Șerban, M. C., Damian, G., Buleu, F., Valcovici, M., & Christodorescu, R. (2020). Dietary patterns and interventions to alleviate chronic pain. Nutrients, 12(9), 2510. https://doi.org/10.3390/nu12092510
- El Paso Back Clinic. (2025). Garlic for back pain: Does it work? http://elpasobackclinic.com/garlic-for-back-pain-does-it-work/
- Imaizumi, V. M., Fontes, A. M. M., & Guizellini, G. M. (2023). Garlic: A systematic review of the effects on cardiovascular diseases. Critical Reviews in Food Science and Nutrition, 63(24), 6797–6819. https://doi.org/10.1080/10408398.2022.2043821
- Jimenez, A. (2025). El Paso Back Clinic: Wellness blog. Retrieved from https://dralexjimenez.com/
- Liu, C. T., Hse, H., Lii, C. K., Chen, P. S., & Sheen, L. Y. (2007). Does garlic have a role as an antidiabetic agent? Molecular Nutrition & Food Research, 51(11), 1353–1364. https://doi.org/10.1002/mnfr.200700082
- Pérez-Rubio, K. G., Méndez-Montoya, J. A., & Ortiz-Muñoz, E. (2022). The Role of Garlic in Metabolic Diseases: A Review. Journal of Medicinal Food, 25(7), 683–694. https://doi.org/10.1089/jmf.2021.0146
- Quesada, I., de Paola, M., & Álvarez-Cilleros, D. (2020). Effect of garlic’s active constituents in inflammation, obesity, and cardiovascular disease. Current Hypertension Reports, 22(1), 6. https://doi.org/10.1007/s11906-019-1009-9
- Rawson, E. S., Miles, M. P., & Larson-Meyer, D. E. (2018). Dietary supplements for health, adaptation, and recovery in athletes. International Journal of Sport Nutrition and Exercise Metabolism, 28(2), 188–199. https://doi.org/10.1123/ijsnem.2017-0340
- Sala-Climent, M., López-Gil, L. F., & Pleguezuelos, E. (2023). The effect of an anti-inflammatory diet on chronic pain: A pilot study. Frontiers in Nutrition, 10, 1205526. https://doi.org/10.3389/fnut.2023.1205526
- Tattelman, E. (2005). Health effects of garlic. American Family Physician, 72(1), 103–106. https://pubmed.ncbi.nlm.nih.gov/16035690/