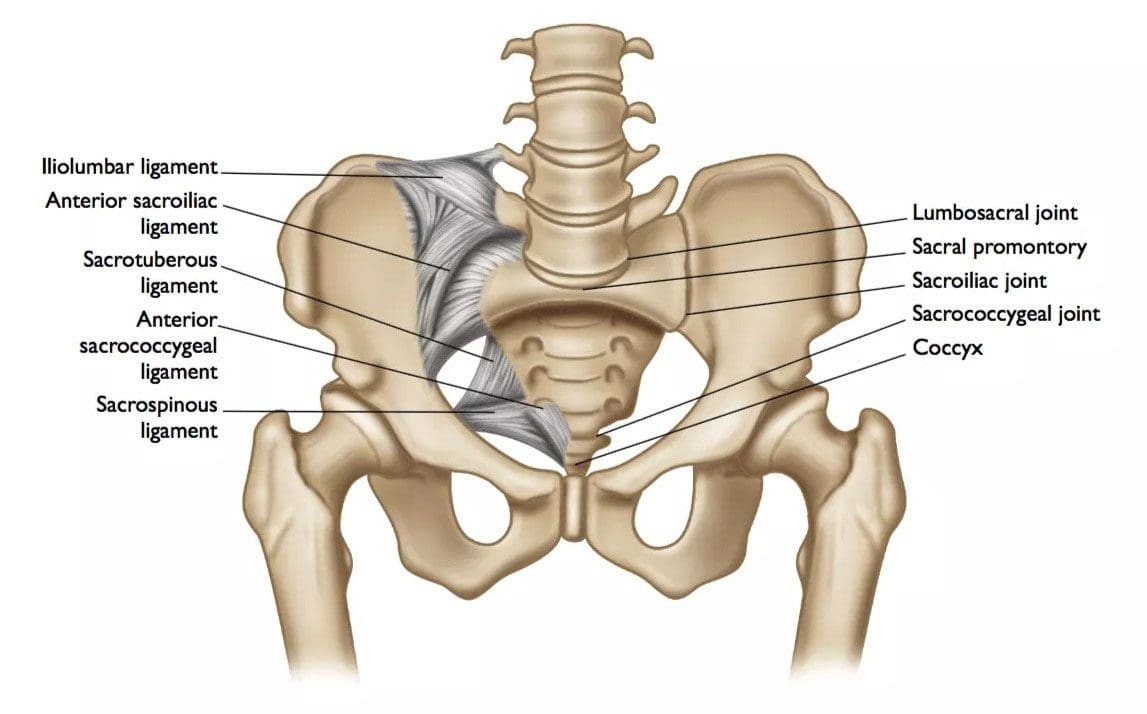
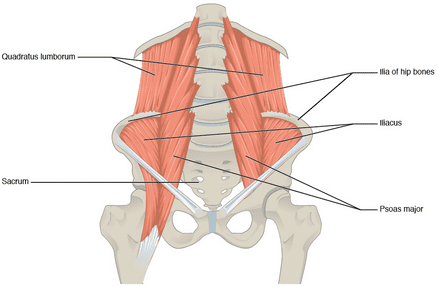
The function of the SI joints is to allow torsional or twisting movements when moving the legs that act as levers. Without the sacroiliac joints and the pubic symphysis at the front of the pelvis, which allow these precision movements, the pelvis would be at higher risk of a fracture. The sacroiliac joints transmit body weight and all the physical forces down through the sacrum to the hips and legs. Individuals, especially athletes with pain in the lower back, hip, groin, or leg, could be experiencing SIJ/sacroiliac joint dysfunction. A physician or surgeon could recommend sacroiliac joint surgery for severe SI joint dysfunction and pain that has not resolved with conservative treatment.
 Sacroiliac Joint Surgery
Sacroiliac Joint Surgery
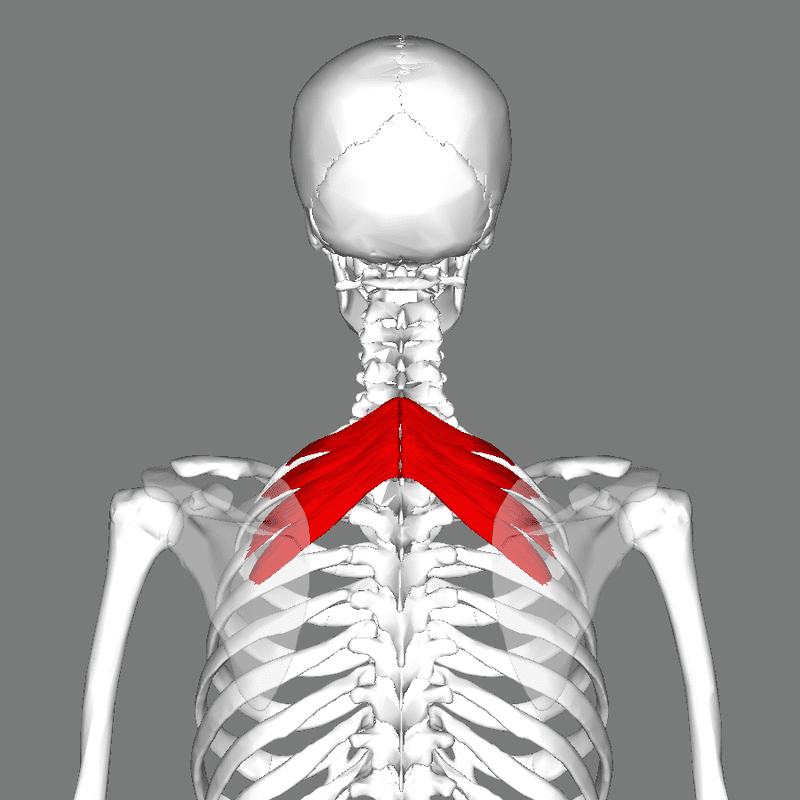
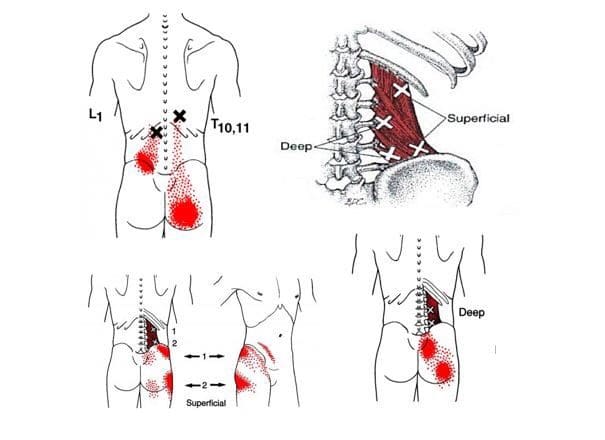
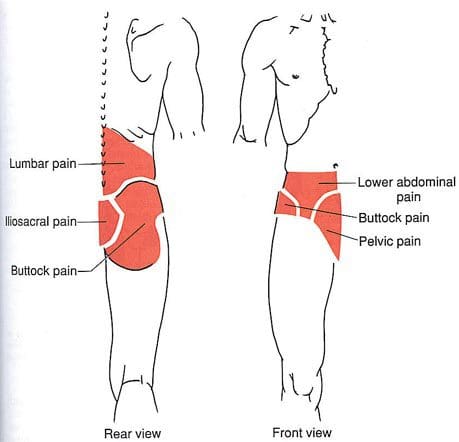
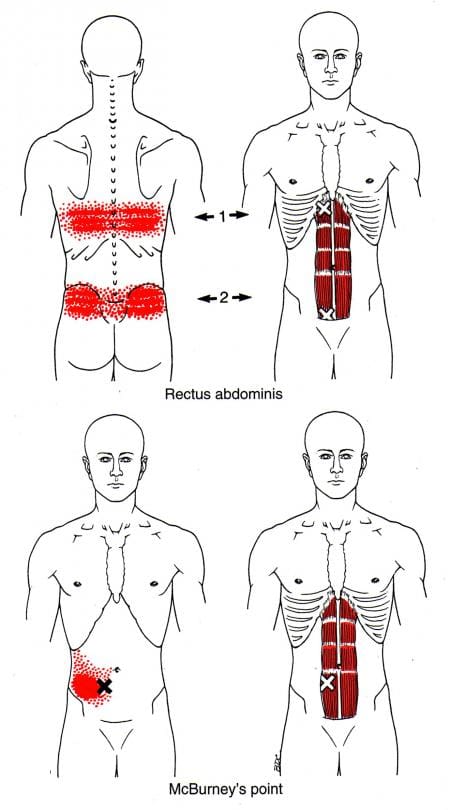
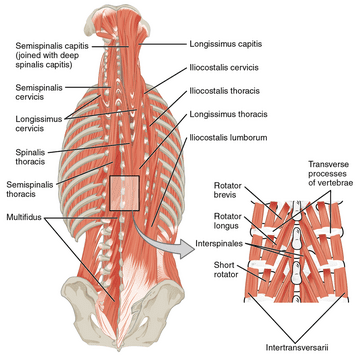
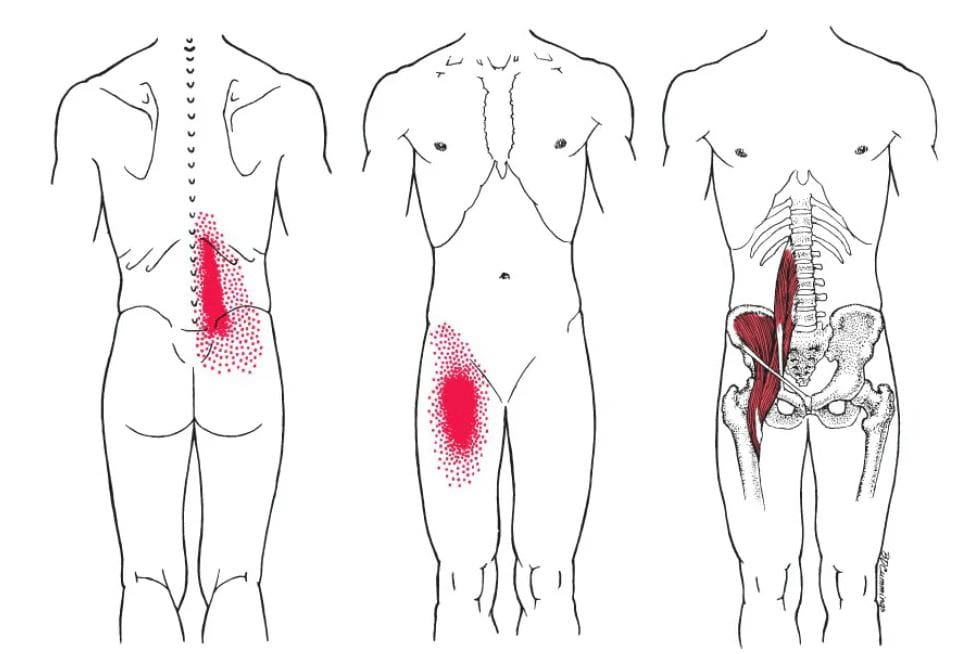
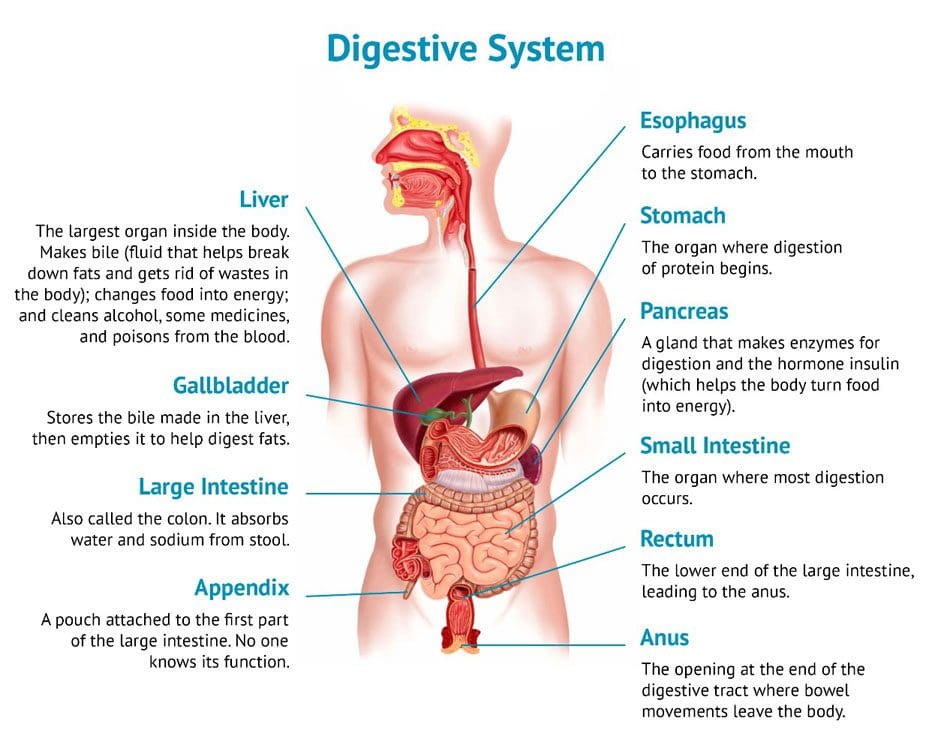
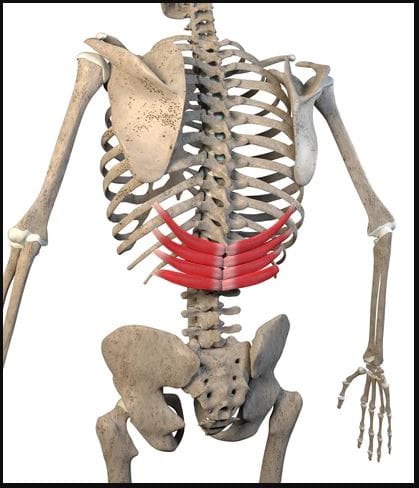
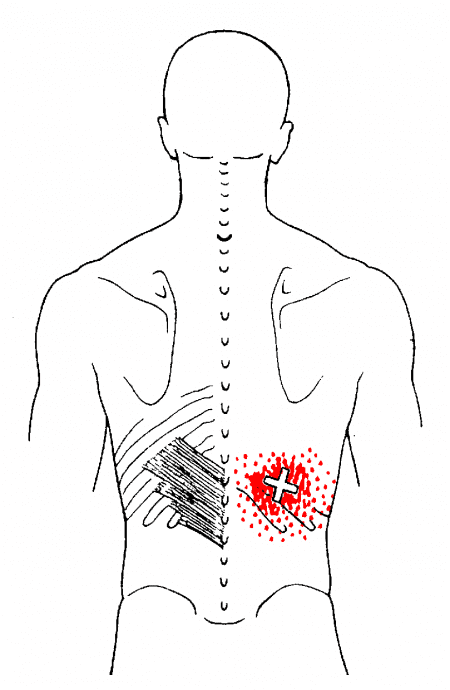
There are two sacroiliac joints. They connect the large iliac bones that make up the sides of the pelvis and the sacrum or triangle-shaped vertebrae between the iliac bones at the base of the spine. Pain in this area can come from sacroiliitis or inflammation of an SI joint, and referred pain may present. A doctor will consider causes such as:
- Trauma
- Sports
- Biomechanical abnormalities
- Wear and tear from weight-bearing stress
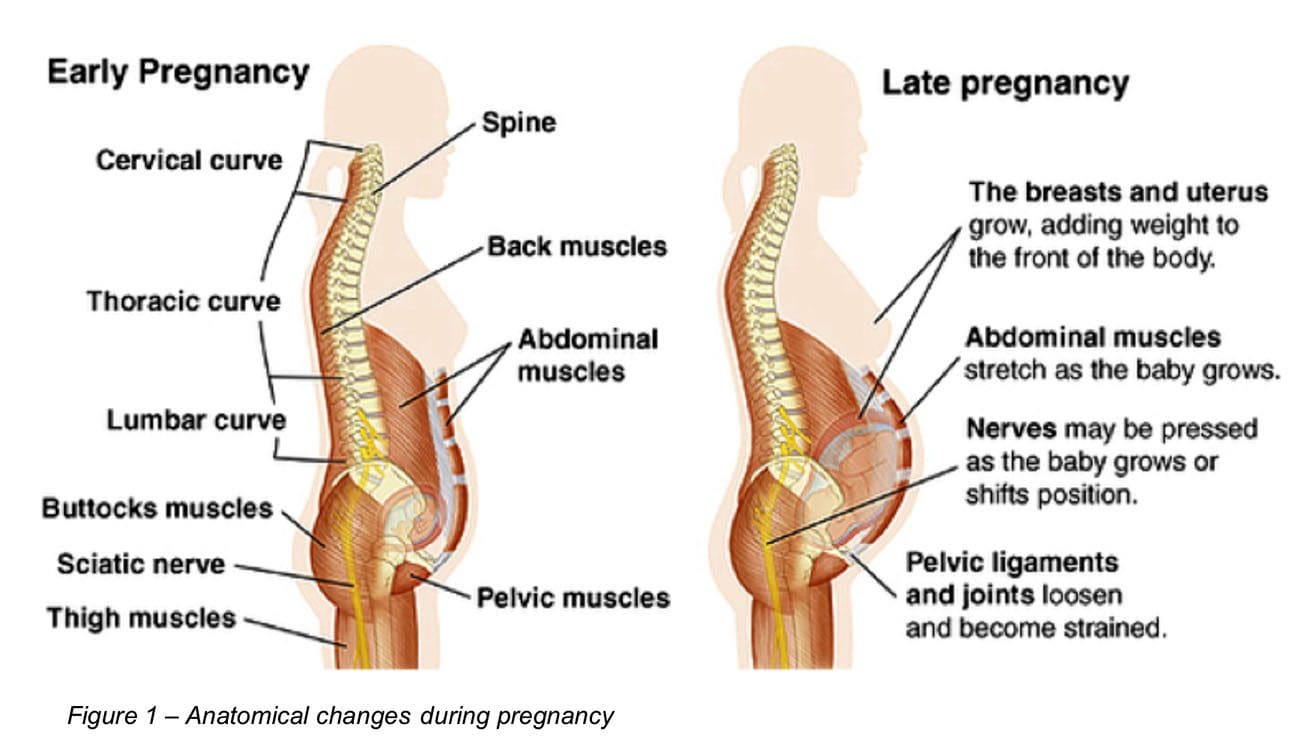
- Pregnancy
- Leg length discrepancy
- Hypermobility
- Systemic inflammatory conditions
- Degenerative joint disease
- Scoliosis
- Infection, but this is rare.
Sports
There is a pathology of sacroiliac joint dysfunction in athletes. Sports that require repetitive and/or asymmetric loading that includes:
- Kicking
- Swinging
- Throwing
- Single-leg stance
Any athlete can develop sacroiliac joint dysfunction, but the highest prevalence activities include:
- Soccer
- Football
- Basketball
- Gymnastics
- Golfing
- Powerlifting
- Cross-country skiing
- Step aerobics
- Stair stepper machines
- Elliptical machines
Fusion Surgery
Surgery is not for patients with less than six months of confirmed localized pain or impairment with other causes ruled out. Surgery is the last option for SI joint pain unless it is an emergency. Doctors and surgeons will recommend non-invasive treatment methods before recommending surgery. Surgery recommendations come when the pain has become intolerable, and the individual can no longer move or operate.
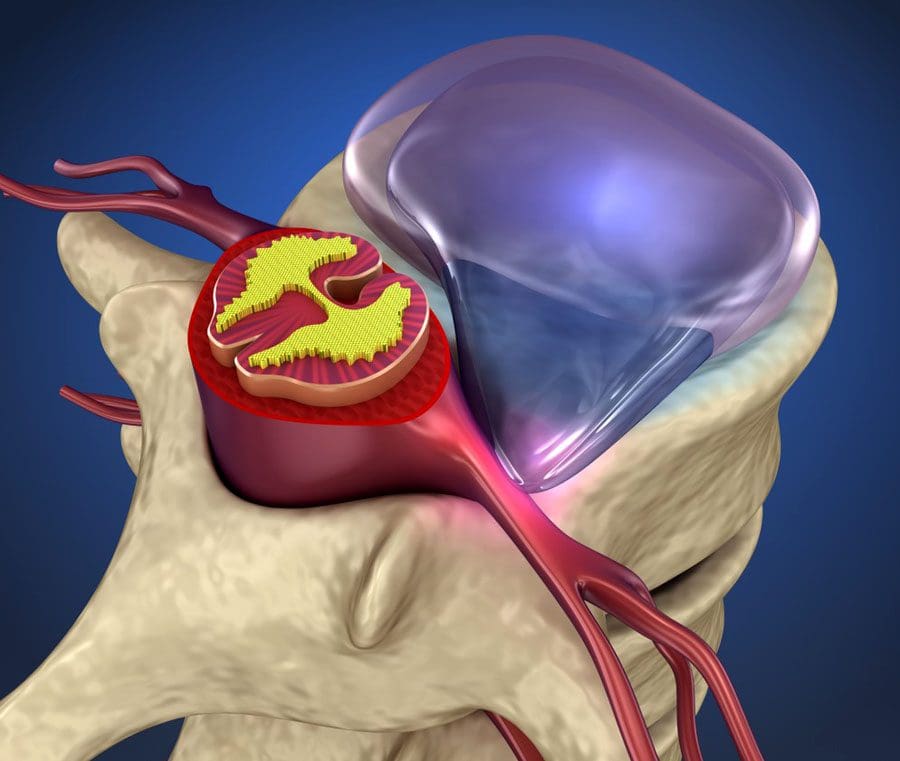
- Sacroiliac joint fusion is a minimally invasive procedure involving a small incision less than two inches long.
- Under image guidance, titanium implants are inserted across the sacroiliac joint to provide stability.
- Holes in the hardware allow for adding bone or for the bone to grow naturally across or onto the area to maintain stability.
- This surgery can be either outpatient or overnight, depending on surgeon preference and the type of support available.
Surgery Recovery Time
For most individuals, recovery time is around three weeks on crutches.
- Pain management depends on whether screws or bolts are involved; bolts tend to be more uncomfortable.
- Post-op pain dissipates in a few days or a couple of weeks.
- Fusion itself takes six or more months to complete.
Conservative Treatment Options
Conservative treatment modalities to reduce the inflammation can include:
- Chiropractic
- Physical therapy
- Nonsurgical spinal decompression
- Medications
- Injections
Rest
- Staying off your feet for a few days can help decrease pressure on the SI joint.
- Using an ice or heating pad on the lower back and/or buttocks.
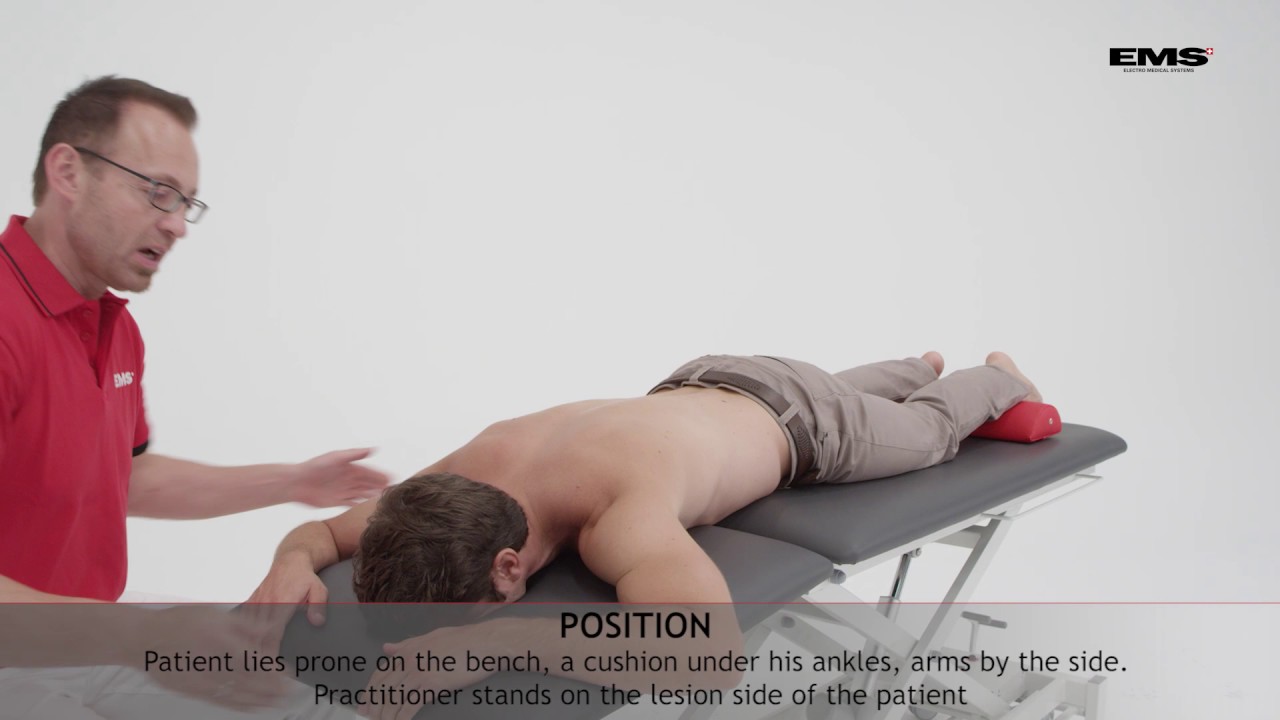
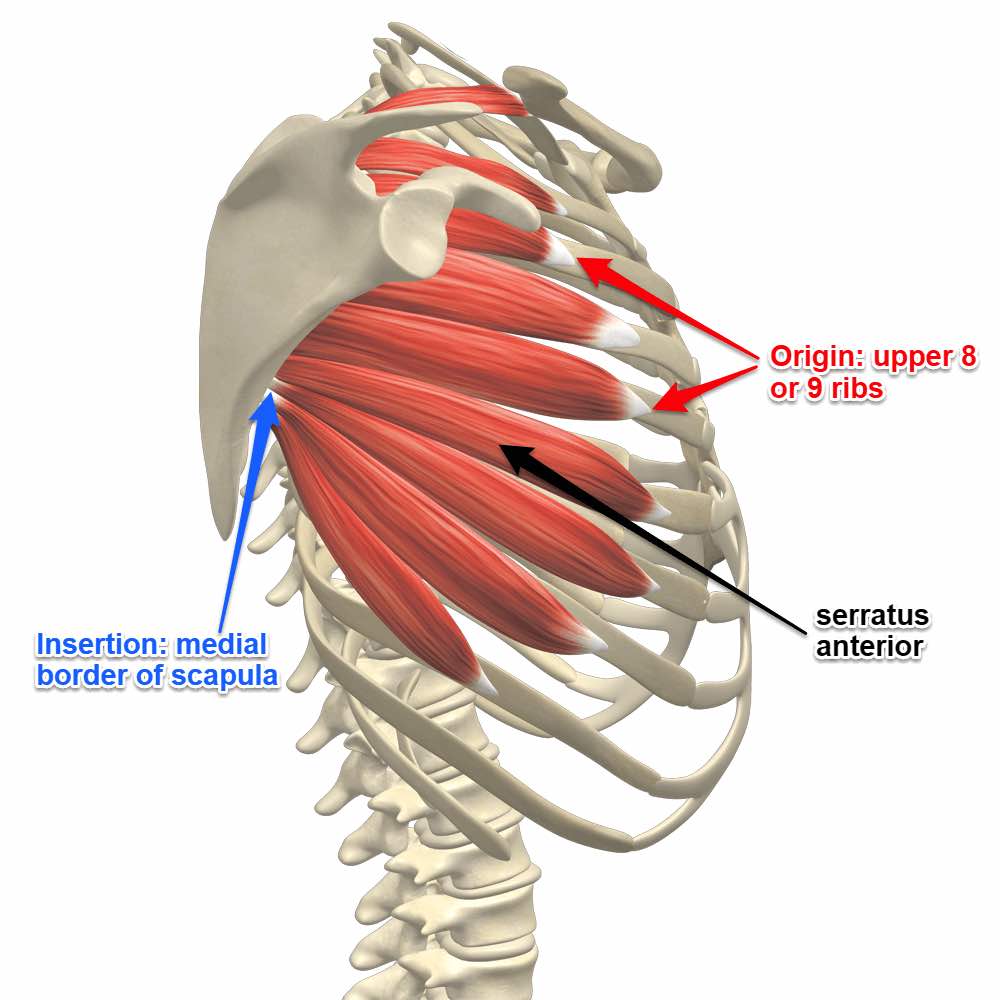
- Massaging the surrounding muscles may help if the apparent cause is an injury.
- A doctor could suggest using a cane, walker, or crutches under medical supervision.
Medications
- Medications include anti-inflammatories such as ibuprofen, naproxen, or prescription alternatives.
- Acetaminophen helps with pain but not inflammation.
Corticosteroids
- Steroids are the most powerful anti-inflammatory.
- A common nonsurgical treatment is cortisol steroids, injected under X-ray guidance.
- Injections go directly to the source.
- Oral steroids spread throughout the body but can cause undesirable side effects.
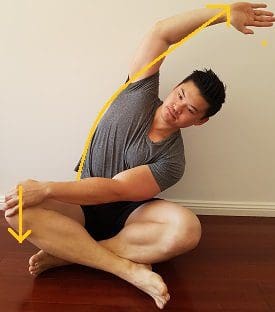
Chiropractic and Physical Therapy
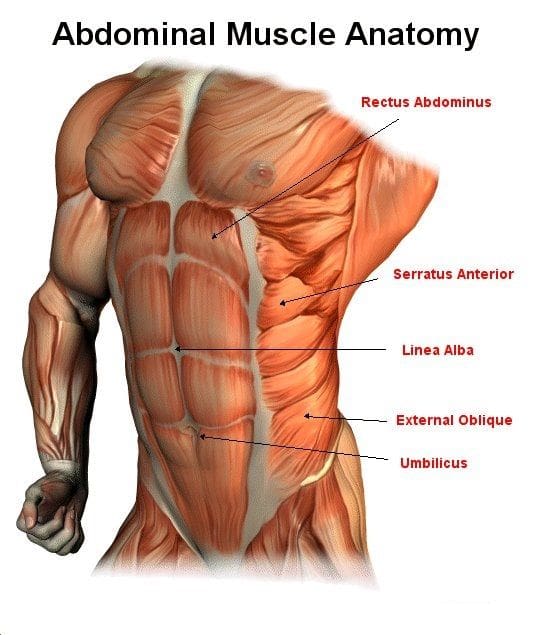
- Depending on the severity of the condition, chiropractic and physical therapy may be able to strengthen the muscles around the area and realign the joint.
- A chiropractor will level the pelvis through sacroiliac joint manipulation and mobilization.
Sacroiliac Support Belt
- Wearing a sacroiliac support belt may help remove the joint’s strain and relieve symptoms.
- It works by applying compression around the hip and across the joint.
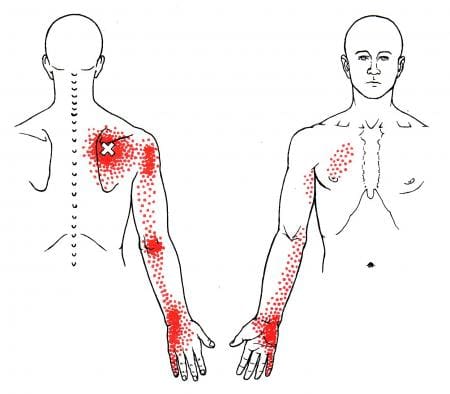
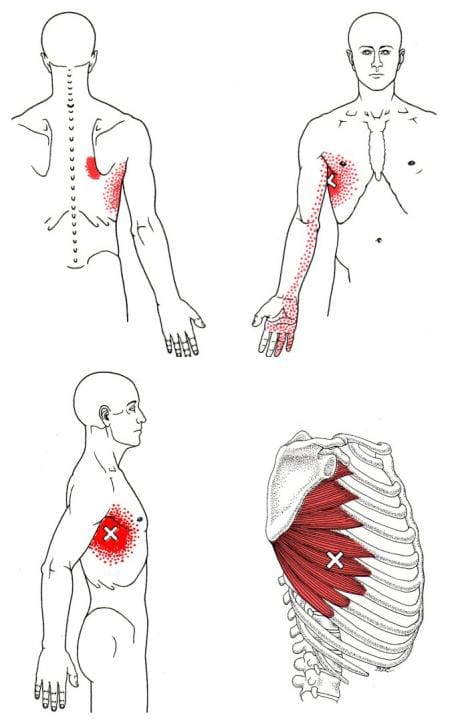
Back, Hip, and Radiating Pain
References
Brolinson, P Gunnar, et al. “Sacroiliac joint dysfunction in athletes.” Current sports medicine reports vol. 2,1 (2003): 47-56. doi:10.1249/00149619-200302000-00009
Heil, Jessica. “Load-Induced Changes of Inter-Limb Asymmetries in Dynamic Postural Control in Healthy Subjects.” Frontiers in human neuroscience vol. 16 824730. 11 Mar. 2022, doi:10.3389/fnhum.2022.824730
International Journal of Spine Surgery. (2020*) “International Society for the Advancement of Spine Surgery Policy 2020 Update—Minimally Invasive Surgical Sacroiliac Joint Fusion (for Chronic Sacroiliac joint Pain): Coverage Indications, Limitations, and Medical Necessity.” https://doi.org/10.14444/7156
Peebles, Rebecca DO1; Jonas, Christopher E. DO, FAAFP2. Sacroiliac Joint Dysfunction in the Athlete: Diagnosis and Management. Current Sports Medicine Reports: 9/10 2017 – Volume 16 – Issue 5 – p 336-342
doi: 10.1249/JSR.0000000000000410


























 Neuropathy Therapeutic Massage
Neuropathy Therapeutic Massage