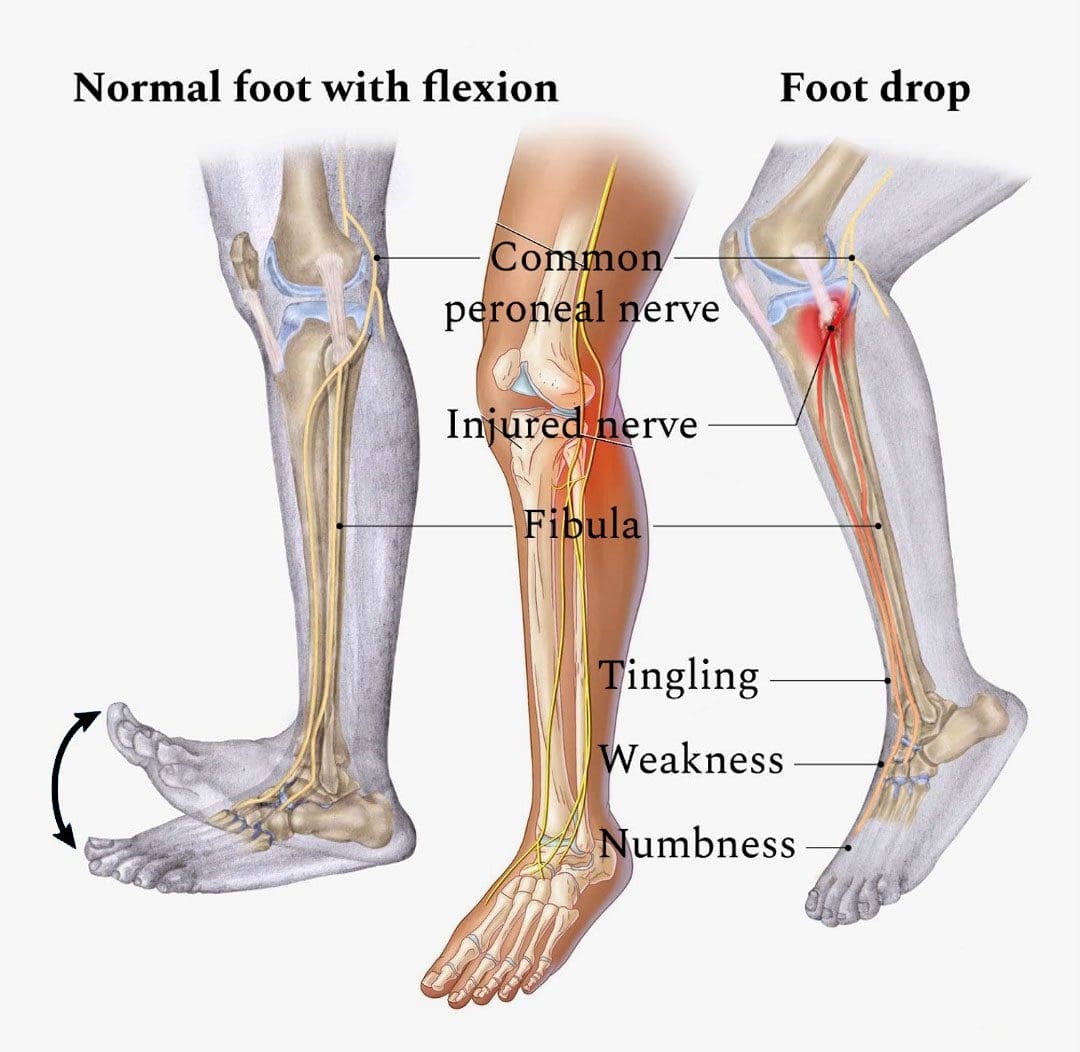
A peroneal nerve injury/peroneal neuropathy can be caused by direct trauma to the outer knee with symptoms and sensations of numbness, tingling, pins-and-needles sensations, pain, or weakness in the foot that can cause a condition known as foot drop. Chiropractic can perform spinal manipulation, realignment, and decompression to restore the nerve’s function. They can also help with walking and mobility by providing muscle strengthening and stretching exercises to correct abnormal gait caused by foot drop and increase the range of motion in the ankle.
Table of Contents
Peroneal Nerve Injury
The peroneal nerve begins near the sciatic nerve at the glutes/hip and buttocks. It travels down the back of the thigh to the knee, which wraps around the front of the leg and extends into the feet to the toes. It provides sensory input from the lateral aspect of the lower leg and the top of the foot. It also provides motor input to the muscles responsible for lifting the foot off the ground lifting the toes and ankles and turning the foot outwards.
Causes
Structural problems in the spine or misalignment can affect the functionality of the nervous system and lead to peroneal neuropathy. Traumatic nerve injury causes include musculoskeletal injury, peroneal nerve paralysis, compression, or laceration. Injuries by trauma and nerve compression include:
- Compression of the nerve in the leg.
- Knee dislocation.
- Knee or hip replacement surgery.
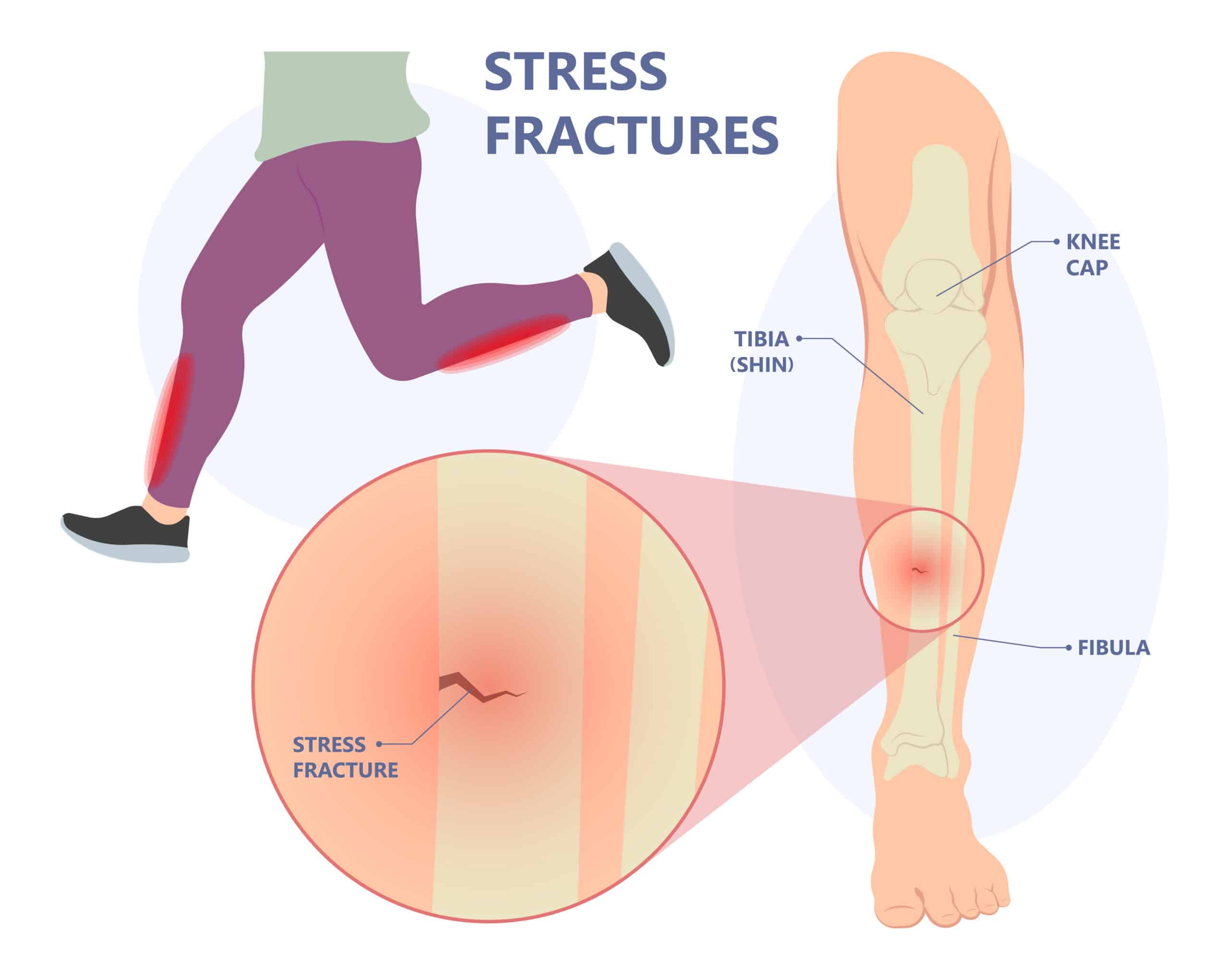
- Knee or leg fracture. Fractures of the tibia or fibula, especially in the areas closer to the knee, can injure the nerve.
- Ankle fracture.
- Blood clot.
- Compression by a nerve sheath tumor or cyst.
Certain underlying medical conditions can cause symptoms of peroneal nerve injury. It is recommended to be evaluated by a medical professional who can diagnose and offer appropriate treatment options. Neurologic disorders that can cause similar symptoms:
- Herniated lumbar disc
- Multiple sclerosis
- Parkinson’s disease
- Amyotrophic lateral sclerosis – ALS or Lou Gehrig’s disease.
- Metabolic syndromes – diabetes, alcohol abuse, exposure to toxins.
Symptoms
Nerve injury symptoms include:
- Numbness, tingling, or loss of sensation in the top of the foot or outer part of the lower leg.
- Inability to flex toes or ankles upward/dorsiflexion.
- Inability to flex the ankle to take a step forward.
- Inability to move the foot.
- Weakness in foot eversion/rotating outward.
- Flopping or slapping sounds when walking.
- Gait changes – dragging the toes or lifting the knee higher than the other to raise the foot off the ground.
- Tripping often.
- Pain in the foot or lower leg.
Diagnosis
In diagnosing a peroneal nerve injury, a healthcare provider examines the leg and analyzes symptoms. Tests can include:
- Imaging tests – CT scan, ultrasound, or MRI.
- Magnetic resonance – MR – neurography is a specialized high-resolution MRI of the nerves.
- An electromyogram measures how muscles react to nerve stimulation.
- Nerve conduction studies measure how electrical impulses run through the nerves.
Treatment
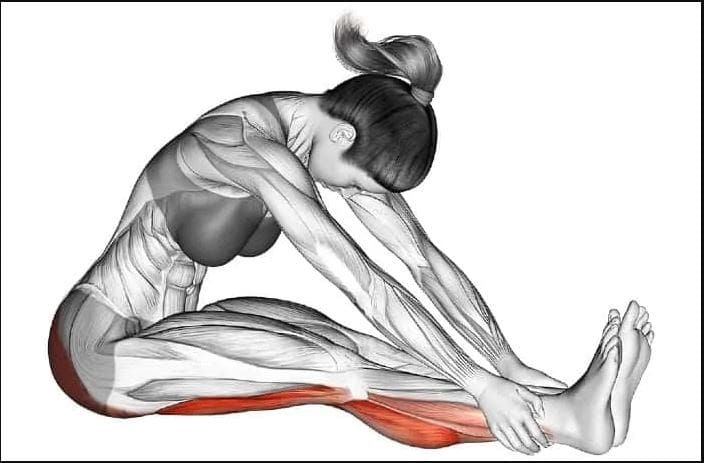
Treatment for a peroneal nerve injury depends on the severity and can be surgical or non-surgical. Non-surgical options include orthotic footwear, chiropractic care, and physical therapy. A physical therapy program could consist of the following:
- Icing
- Massage
- Manual manipulation
- Stretching
- Strengthening exercises
- Mobilization exercises
- Balancing exercises
- Ankle bracing
- Ankle taping
- Shoe inserts – splints, braces, or orthotics can improve gait.
- Gait training to walk without the drop.
Ankle Sprain Chiropractor
References
Longo, Diego, et al. “The Muscle Shortening Maneuver: a noninvasive approach to treating peroneal nerve injury. A case report.” Physiotherapy theory and practice, 1-8. 31 Jul. 2022, doi:10.1080/09593985.2022.2106915
Milenković, S S, and M M Mitković. “Common peroneal nerve schwannoma.” Hippokratia vol. 22,2 (2018): 91.
Radić, Borislav et al. “PERIPHERAL NERVE INJURY IN SPORTS.” Acta clinica Croatica vol. 57,3 (2018): 561-569. doi:10.20471/acc.2018.57.03.20
Thatte H et al. (2022). Electrodiagnostic evaluation of peroneal neuropathy. ncbi.nlm.nih.gov/books/NBK563251/
T Francio, Vinicius. “Chiropractic care for foot drop due to peroneal nerve neuropathy.” Journal of bodywork and movement therapies vol. 18,2 (2014): 200-3. doi:10.1016/j.jbmt.2013.08.004


















 Cross Training
Cross Training