Table of Contents
Introduction
The central nervous system transmits information between the brain, muscles, and organs through 31 nerve roots from the spinal cord. These nerve roots are interconnected with the body’s muscles and organs, ensuring each body section is connected to the upper and lower extremities. The neuron signals transmitted through these nerve roots provide sympathetic and parasympathetic signaling, allowing the body and its systems to function correctly. However, injuries and pathogens affecting the nerve roots can cause the neuron signals to become unstable, involving the muscles, tissues, and vital organs and leading to chronic conditions and pain-like symptoms. Fortunately, small changes in diet and supplements can help reduce nerve pain and improve a person’s quality of life. This article will discuss nerve pain and its symptoms, how nutrients and supplements can help reduce it, and non-surgical treatments that can help restore the body from nerve pain. We work with certified medical providers who use our patients’ valuable information to provide non-surgical treatments for nerve pain combined with nutrients and supplements from reoccurring. We encourage patients to ask essential questions and seek education from our associated medical providers about their condition. Dr. Jimenez, D.C., provides this information as an educational service. Disclaimer
How Does Nerve Pain Occur In The Body?
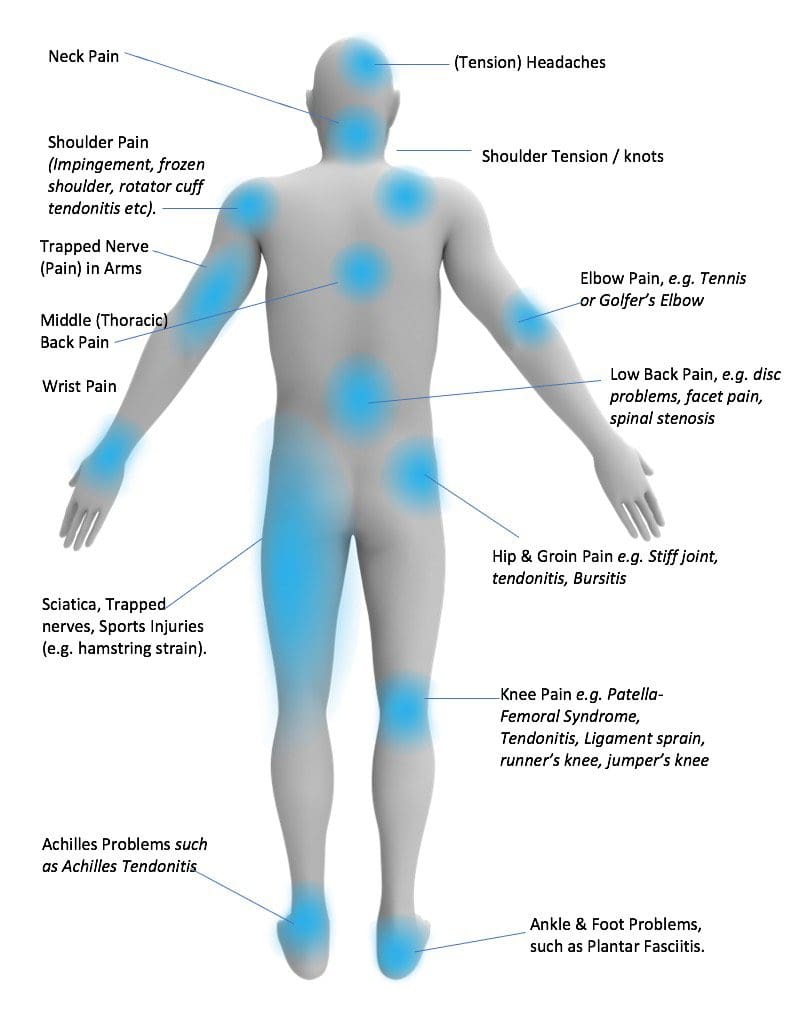
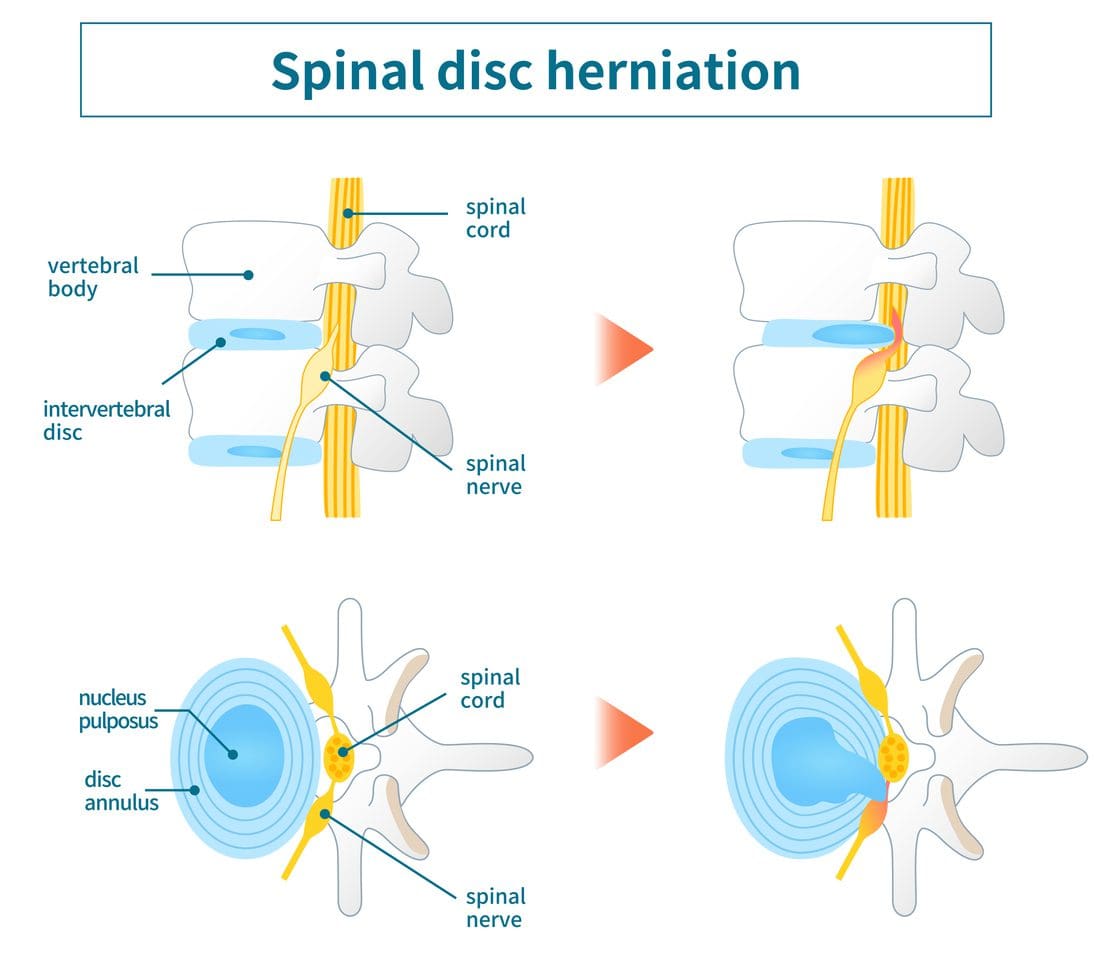
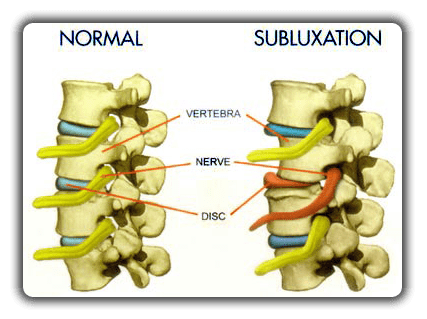
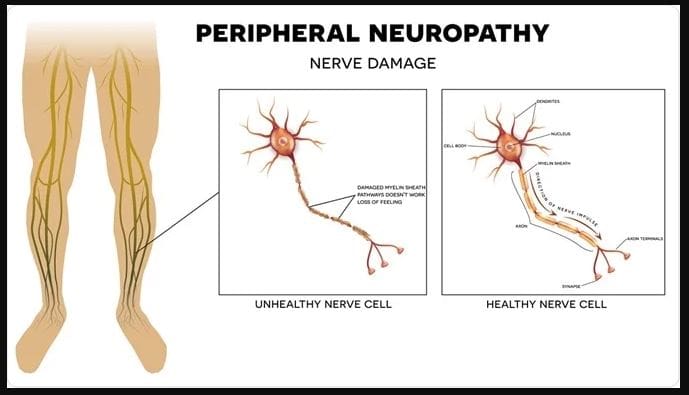
Have you been experiencing pins and needles in your hands or feet or constant muscle twitches? Maybe you’re feeling pain in your upper or lower extremities. If you’ve had these sensations all over your body, it could be due to nerve pain affecting your musculoskeletal system. Research studies have shown nerve pain is often caused by a lesion or disease that is affecting the brain’s somatosensory system. This can cause an imbalance in neuron signaling and disrupt information traveling to the brain. The somatosensory system is responsible for our ability to feel, touch, and experience pressure and pain. When it’s affected by injuries or pathogens, information can be disrupted in the spinal cord and brain. Additional research studies revealed that nerve pain could be caused by compressed nerve roots, leading to ongoing or intermittent pain that may spread to different areas and cause structural changes involving peripheral and central sensitization. This can lead to associated symptoms that can disrupt normal body functions.
Nerve Pain Symptoms
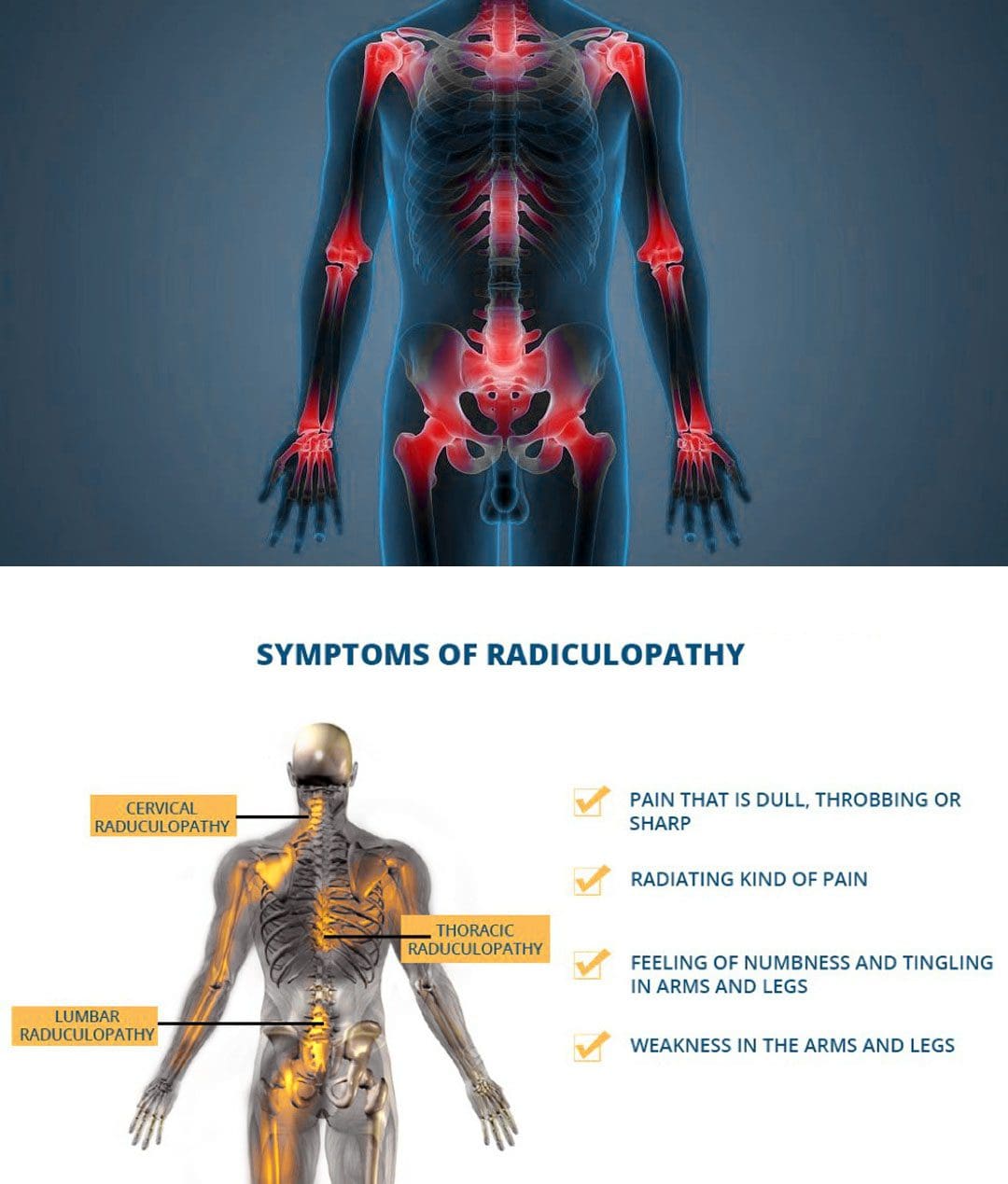
It might be nerve pain if you are feeling pain in your upper or lower extremities. Research studies revealed that this type of pain can cause symptoms that feel like pain in your muscles or organs, but neurological disorders may cause it. The severity and specific symptoms can vary from person to person. Some common symptoms of nerve pain include:
- Referred pain
- Numbness
- Tingling
- Cognitive deficits
- Loss of sensory and motor function
- Inflammation
- Pain to light touches
Nerve pain is a common issue for those with chronic conditions, and research shows that nociceptive and neuropathic pain mechanisms are interconnected. For instance, back pain and radiculopathy are often linked, causing referred pain. This means that the pain receptors are in a different location from where the pain originated. However, there are ways to alleviate nerve pain symptoms and address underlying factors contributing to this discomfort.
The Functional Medicine Approach- Video
Suppose you suffer from nerve pain and seek to alleviate the symptoms and restore your body’s natural state. While making small changes can help, they may not provide quick results. However, functional medicine and non-surgical treatments can help with nerve pain and associated symptoms. The video above explains how functional medicine is safe and personalized and can be combined with other therapies to strengthen surrounding muscles and ligaments. By being more mindful of your body’s needs, you can find relief from nerve pain and improve your overall health.
Nutrients For Nerve Pain
Dr. Eric Kaplan, D.C., FIAMA, and Dr. Perry Bard, D.C., wrote “The Ultimate Spinal Decompression” and explained that our body’s nerves require constant nutrients for maintenance and repair. It’s crucial to incorporate various nutrients and supplements to reduce nerve pain and its symptoms. Here are some essential body nutrients that can help alleviate nerve pain.
Nitric Oxide
The body produces a vital nitric oxide nutrient, which can help alleviate nerve pain. Insufficient nitric oxide production can result in health issues such as high blood pressure, erectile dysfunction, and respiratory and cardiovascular problems. Nitric oxide works as a vasodilator, relaxing the blood vessels in the inner muscles, promoting increased blood flow, and reducing elevated blood pressure levels. Nitric oxide is crucial in supporting the nervous and cardiovascular systems, ensuring that neuron signals in nerve roots remain stable. Research studies indicate that taking nitric oxide supplements can enhance exercise performance.
ATP
ATP is a crucial nutrient that the human body naturally produces. Its primary role is to store and generate energy within the cells. ATP plays a significant role in the proper functioning of various organs and muscles in the body. The body’s metabolic pathway, cellular respiration, creates ATP, one of the most efficient processes. We use ATP in our daily lives by consuming food and drinks, and the air we breathe helps break down ATP, thus producing water in the body. Additionally, when the body is in motion, ATP works with nitric oxide to produce energy output in the nerves, muscles, and organs.
Supplements For Nerve Pain
The body requires supplements in addition to nutrients to alleviate symptoms of fatigue, inflammation, and pain caused by nerve pain. Nerve pain can affect the parasympathetic and sympathetic nerves, leading to disrupted neuron signals, resulting in the brain sending the immune system to attack healthy cellular structures as if they were foreign invaders. However, research has shown that incorporating supplements can help reduce the inflammatory effects of nerve pain, improve neural regeneration, reduce oxidative stress, and enhance motor and functional recovery from injured nerves.
Treatments For Nerve Pain
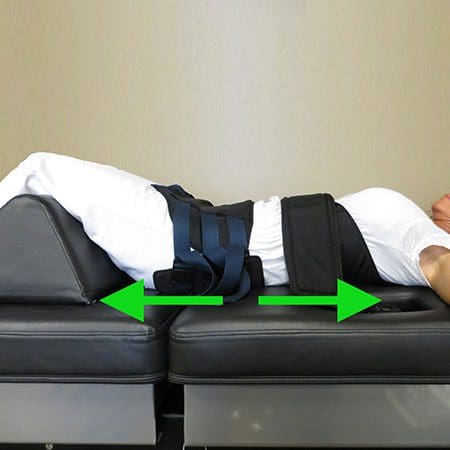
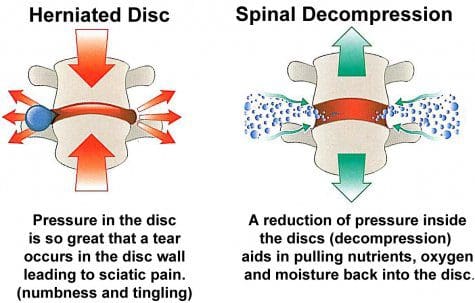
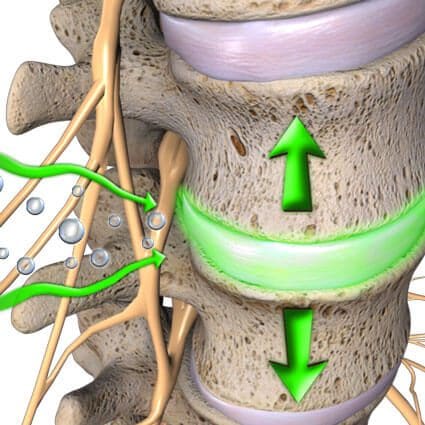
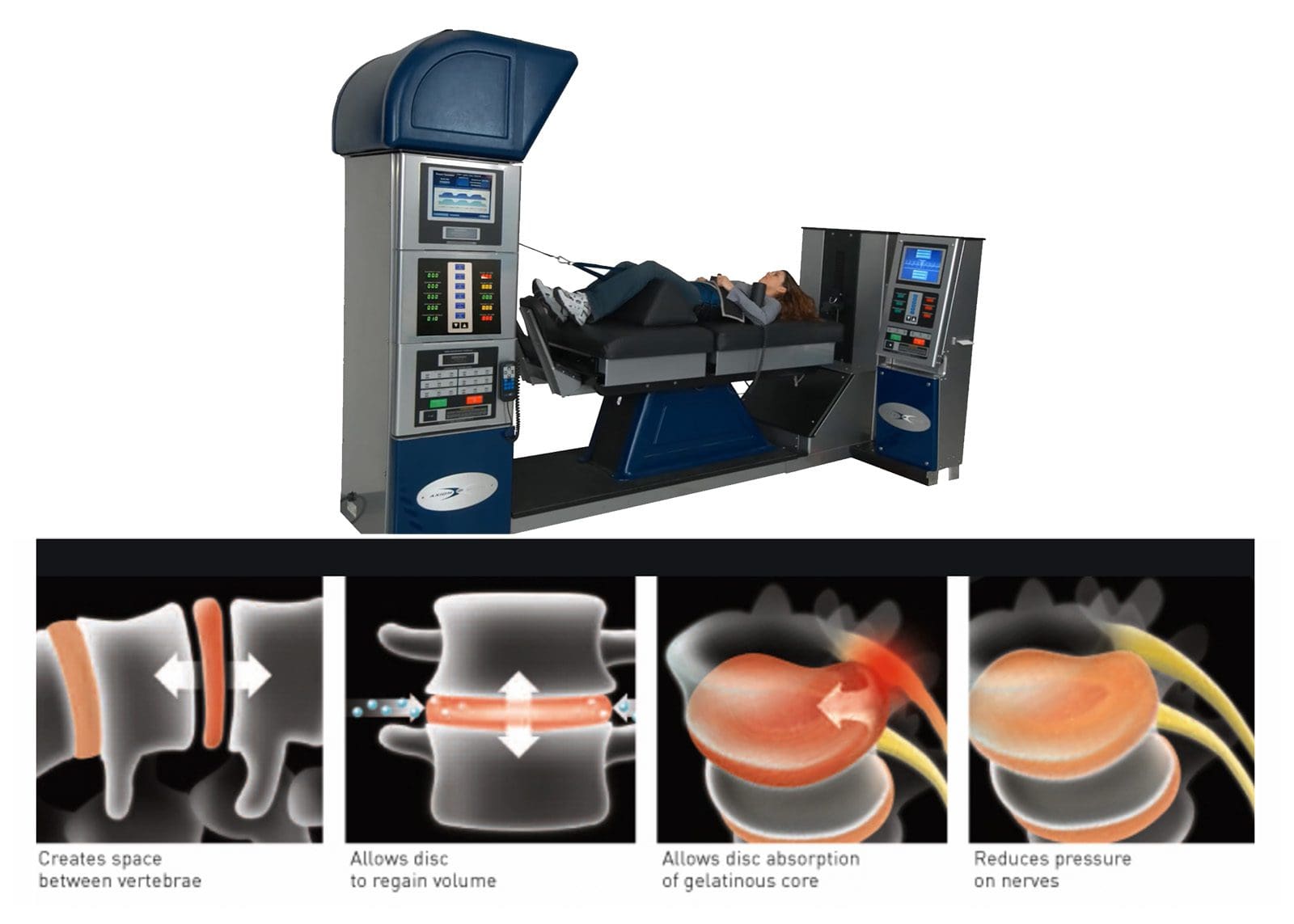
To effectively reduce the impact of nerve pain, individuals often consult with their primary doctor to develop a personalized treatment plan. Nutrients and supplements are only half of the recovery process. Non-surgical treatments such as chiropractic care, physical therapy, and spinal decompression can significantly lower chronic conditions associated with nerve pain. Studies have shown that compressed nerve roots caused by pathological factors can lead to overlapping risk profiles that affect the body. Spinal decompression is a treatment that relieves compressed nerves through gentle traction on the spinal disc. Spinal decompression, combined with a healthy diet, exercise, and other therapies, can educate people on preventing nerve pain from returning.
Conclusion
Nerve pain can severely impact a person’s life, causing disability and reduced quality of life due to its potential risks to muscles, organs, and tissues. However, incorporating a variety of nutrients and supplements into the body can help reduce the effects of nerve pain. By combining these methods with non-surgical treatments, individuals can better understand what’s happening to their bodies and work to restore them to normal. A personalized plan for health and wellness that includes these techniques can alleviate nerve pain and its symptoms and promote natural healing.
References
Kaplan, E., & Bard, P. (2023). The Ultimate Spinal Decompression. JETLAUNCH.
















 Athletic Running Shoes
Athletic Running Shoes