Table of Contents
What Happens to Your Spine During Crashes, Work Injuries, Sports, and Falls—and How Integrative Chiropractic Care Can Help

The big picture: fast forces, fragile tissues
When a car crash, work accident, sports injury, or fall occurs, your body stops suddenly—but your head and torso often continue moving for a split second. That quick hyperextension, flexion, rotation, and compression places huge stress on the neck and back. The spine’s joints, ligaments, discs, and nerves can all be injured. In severe cases, the spinal cord itself is affected, which can result in loss of movement or sensation below the injury level (Mayo Clinic, 2024; NINDS, 2025). Mayo Clinic+1
High-energy impacts also shake the brain. Even without a direct head blow, rapid acceleration and deceleration can make the brain slide and twist inside the skull. Microscopic fibers (axons) can stretch, which explains why concussions and post-concussion problems can occur with whiplash and torso impacts (Fehily & Fitzgerald, 2017; Converse et al., 2019). PMC+1
Common spinal injuries after high-impact events
Whiplash and soft-tissue sprains/strains
Sudden back-and-forth motion can overstretch the facet joint capsules, muscles, and ligaments. People often report neck pain, stiffness, headaches, and reduced range of motion. Whiplash can co-occur with concussion because the same motion rattles the brain (Cognitive FX, 2023). CognitiveFX
Herniated discs
Compression and twisting can push disc material outward, irritating nerves. Leg pain (sciatica) or arm pain, along with numbness and weakness, may follow (BBGA, 2025). Blasingame & Ashley, P.C.
Vertebral fractures (including cervical injuries)
High-energy trauma can fracture the vertebrae. Certain neck fractures—like C2 “Hangman” fractures—involve the pars interarticularis and may cause instability; urgent immobilization and specialty care are critical (LeFever & Caruso, 2023; McMordie & Piche, 2023). NCBI+1
Spinal cord injuries (SCI)
SCIs range from transient symptoms to permanent deficits. Warning signs include weakness, numbness, loss of coordination, and changes in bowel/bladder function. SCIs can also cause exaggerated reflexes and muscle tone changes over time (spasticity) (Mayo Clinic, 2024; NINDS, 2025). Mayo Clinic+1
Blunt cerebrovascular injury (BCVI)
A severe hit to the head/neck can injure the carotid or vertebral arteries, increasing stroke risk—especially in severe head injury. Screening protocols now recognize BCVI in up to 1–2% of hospitalized trauma patients and higher in severe head injury (Brommeland et al., 2018). BioMed Central
Key point: One event can affect multiple systems at once—joints, discs, nerves, spinal cord, blood vessels, and the brain—which is why careful, team-based evaluation matters (UT Southwestern, n.d.; Weill Cornell, n.d.). UT Southwestern Medical Center+1
How the same physics injure the brain
Rapid motion can create shear and strain inside the brain’s soft tissue. Biomechanics research indicates that deformation, strain rate, and pressure waves can alter brain function and structure, thereby helping to explain concussion symptoms and, in some cases, the mechanisms of diffuse axonal injury (Goriely et al., 2015; Freire et al., 2023; BrainandSpinalCord.org, n.d.). SpringerLink+2MDPI+2
What you might feel: headache, fogginess, balance problems, light/noise sensitivity, neck pain, and slowed thinking. These symptoms can mix with spinal pain and muscle guarding, which is why people sometimes “don’t feel right” for weeks (Cognitive FX, 2023). CognitiveFX
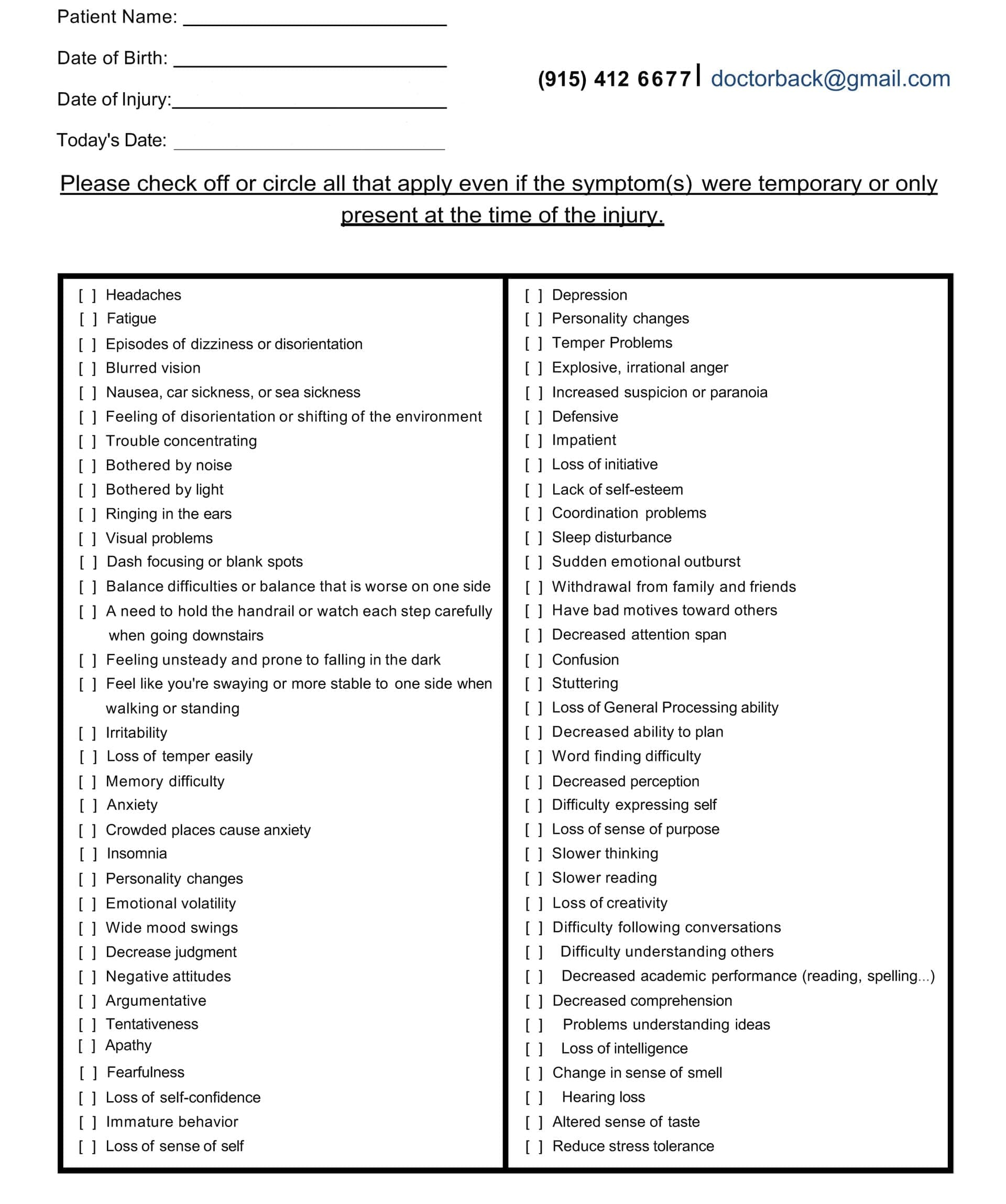
Head Injury/TBI Symptom Questionnaire:
Red flags: when to seek emergency care
Call emergency services or go to the ER if you have any of the following after a crash, fall, or sports hit:
-
Severe neck or back pain, new weakness, numbness, or trouble walking
-
Loss of bladder or bowel control
-
Breathing difficulty or chest tightness
-
Worsening severe headache, repeated vomiting, confusion, or unusual drowsiness
-
One-sided weakness or face droop (possible stroke with BCVI)
These red flags align with major guidelines for SCI and TBI (Mayo Clinic, 2024; NINDS, 2025; Brommeland et al., 2018). Mayo Clinic+2NINDS+2
How clinicians figure out what’s wrong
-
History and exam. Providers assess neck/back range of motion, neurologic function, balance, eye tracking, and signs of concussion.
-
Imaging when indicated. Depending on symptoms and trauma mechanism, teams may order X-rays, CT, and/or MRI for the spine and brain (UT Southwestern, n.d.). UT Southwestern Medical Center
-
Vascular screening. In high-risk patterns (e.g., high cervical fracture, severe head injury), protocols recommend screening for BCVI, often with CT angiography (Brommeland et al., 2018; NCBI Bookshelf, 2013). BioMed Central+1
What different injuries feel like
-
Whiplash/strains: stiff, achy neck; headaches at the base of the skull; pain that worsens with movement. Often linked to dizziness or mild cognitive complaints when a concussion is also present (Cognitive FX, 2023). CognitiveFX
-
Herniated disc: shooting arm or leg pain, numbness/tingling, weakness, worse with coughing/sneezing (BBGA, 2025). Blasingame & Ashley, P.C.
-
Facet joint irritation: sharp, localized neck or back pain with extension/rotation.
-
SCI: weakness or loss of sensation below the injury; spasticity; autonomic symptoms such as sweating or blood pressure swings in some cases (Mayo Clinic, 2024; NINDS, 2025). Mayo Clinic+1
Sports and youth considerations
Sports also put a strain on the neck and back through tackling, falls, collisions, and high-velocity rotations. Pediatric and adolescent athletes can sustain cervical fractures, dislocations, or neurologic deficits; careful rule-out is essential when symptoms or mechanisms are concerning (Lu et al., 2024). MDPI
Why integrative chiropractic care?
Integrative chiropractic care employs a noninvasive, whole-person approach that combines manual therapies, graded exercise, posture and movement retraining, and collaborative teamwork with medical professionals, including primary care, neurology, physical medicine and rehabilitation (PM&R), pain medicine, and, when necessary, surgery. The goal is to relieve pain, restore motion, retrain the nervous system, and support a safe return to activity.
Dr. Alexander Jimenez, DC, APRN, FNP-BC, in El Paso, emphasizes dual-scope care—combining chiropractic assessment and treatment with nurse practitioner training to coordinate imaging, referrals, and integrative plans. His clinic specializes in co-management for auto injuries, work-related injuries, and sports-related trauma, focusing on biomechanics, symptom control, and progressive rehabilitation (Jimenez, 2023; Jimenez, 2025). El Paso, TX Doctor Of Chiropractic+1
What “integrative” looks like in practice
-
Assessment: rule out red flags; screen for concussion; test balance, eye movements, and cervical joint function; review work/sport demands (Jimenez, 2023; Sports Head Injuries overview, 2025). El Paso, TX Doctor Of Chiropractic+1
-
Manual therapy: gentle, evidence-informed spinal mobilization/adjustments when appropriate to improve joint motion and decrease pain and muscle guarding.
-
Soft-tissue care: myofascial release, stretching, and graded loading for injured tissues.
-
Movement rehab: progressive mobility/strength, deep-neck flexor and scapular training, hip-core integration, and return-to-work/return-to-play progressions.
-
Neurologic support: cervical proprioception drills, vestibular/oculomotor exercises for post-whiplash concussion symptoms, coordinated with medical providers.
-
Care coordination: imaging, specialist referral (neurosurgery, orthopedics, neurology, pain), and vascular screening if indicated (UTSW; BCVI guidelines). UT Southwestern Medical Center+1
Reality check: When there’s spinal cord damage, unstable fractures, or vascular injury, conservative care alone is not enough. Emergency stabilization and specialist management come first (Mayo Clinic, 2024; NINDS, 2025). Mayo Clinic+1
Step-by-step care plan after a crash, work injury, sports hit, or fall
This is a general roadmap. Your personal plan depends on your exam, imaging, and goals.
Step 1: Protect and assess (first 24–72 hours)
-
Stop risky activity, protect the neck/back; consider a soft collar briefly only if prescribed.
-
Medical evaluation to screen red flags (weakness, numbness, concussion symptoms, vascular concerns).
-
Imaging when indicated (X-ray/CT/MRI). (UT Southwestern, n.d.; Mayo Clinic, 2024). UT Southwestern Medical Center+1
Step 2: Calm the acute phase (days 2–14)
-
Relative rest + gradual activity, avoiding complete bed rest.
-
Pain management: use ice/heat as directed; take short-term medications as prescribed by your PCP; receive gentle manual therapy if cleared.
-
Begin with isometrics and breathing drills, followed by short, frequent walks.
-
Concussion support: light cognitive load; adequate sleep, hydration, and nutrition (Freire et al., 2023). MDPI
Step 3: Restore motion and control (weeks 2–6)
-
Spinal mobilization/adjustments (if appropriate) to reduce stiffness and improve joint mechanics.
-
Targeted strength and endurance for deep-neck flexors, scapular stabilizers, and core/hip.
-
Vestibular/oculomotor rehab if dizzy, foggy, or visually sensitive (Cognitive FX, 2023; Jimenez, 2025). CognitiveFX+1
Step 4: Load and integrate (weeks 4–12)
-
Work- or sport-specific patterns: lifting mechanics, anti-rotation core work, landings, cutting, and deceleration.
-
Aerobic training: improves circulation and brain recovery.
-
Ergonomics and micro-breaks for desk or tool-based jobs.
Step 5: Return to performance + prevention (months 2–6)
-
Graded return-to-play/return-to-work with measurable criteria (pain-free ROM, strength symmetry, functional tests).
-
Education: sleep, anti-inflammatory eating, and stress management to reduce recurrence (Jimenez, 2023; UTSW, n.d.). El Paso, TX Doctor Of Chiropractic+1
Special situations you should know about
Cervical fractures and instability
Certain C2 injuries (e.g., dens, pars) require immobilization or surgery; unstable cases should not be manipulated until cleared by a spine specialist (LeFever & Caruso, 2023; McMordie & Piche, 2023). NCBI+1
Spinal cord injury and long-term changes
SCI can lead to lasting weakness/sensory loss, spasticity, and autonomic issues. Rehab focuses on preserving function and preventing complications (Mayo Clinic, 2024; NINDS, 2025). Mayo Clinic+1
Blunt cerebrovascular injury (BCVI)
High-risk trauma patterns should trigger screening to prevent stroke. Teams use CT angiography and follow evidence-based pathways (Brommeland et al., 2018). BioMed Central
What to expect from an integrative chiropractic visit
-
History & red-flag screen (neurologic, vascular, concussion).
-
Exam (spine, nerves, balance, eye tracking).
-
Decision on imaging/referrals (coordinated with your PCP or specialists).
-
Care plan with staged goals: pain reduction → motion → control → load → performance.
-
Education & self-care: sleep, hydration, anti-inflammatory nutrition, and stress regulation.
-
Follow-ups to progress exercise and reduce relapse risk.
Dr. Jimenez’s dual-scope background (chiropractor and board-certified family nurse practitioner) supports this coordination, especially after auto and work injuries, where medical documentation and team care are crucial (Jimenez, 2023; Jimenez, 2024–2025). El Paso, TX Doctor Of Chiropractic+1
Frequently asked questions
Q: Can a rear-end crash hurt both the neck and the brain?
A: Yes. The same acceleration that strains the neck can also move the brain inside the skull, leading to concussion-type symptoms. That’s why neck care and concussion care often happen together (Cognitive FX, 2023). CognitiveFX
Q: Do all whiplash patients need imaging?
A: No. Imaging depends on red flags, age, and exam rules. Your clinician will determine whether an X-ray, CT scan, or MRI is appropriate (UT Southwestern, n.d.). UT Southwestern Medical Center
Q: Are spinal cord injuries always permanent?
A: Some deficits can improve with time and rehabilitation, but severe SCIs may cause lasting changes. New therapies are being studied (Mayo Clinic, 2024). Mayo Clinic
Q: Is chiropractic safe after a concussion?
A: With proper screening and when medically appropriate, gentle cervical care plus vestibular/oculomotor rehab can help neck-related headaches, balance, and movement control—as part of a team plan (Jimenez, 2025). El Paso, TX Doctor Of Chiropractic
A simple self-care checklist (not a substitute for medical care)
-
Move early but smart: short, frequent walks; avoid heavy lifting or high-risk moves at first.
-
Neck basics: chin tucks, gentle rotations as tolerated; stop if dizzy or symptomatic.
-
Hydrate and consume protein-rich meals to support tissue repair; prioritize quality sleep.
-
Track symptoms, such as headaches, dizziness, numbness, and weakness—share updates with your clinician.
-
Return gradually: progress activity with clear milestones; don’t rush.
How this helps at work and in sports
-
Work: ergonomics, micro-breaks, and graded duty can protect healing tissues.
-
Sports: a return-to-play progression protects the neck, spine, and brain while restoring timing, reaction, and confidence (Jimenez, 2025). El Paso, TX Doctor Of Chiropractic
When surgery or specialty care is needed
-
Unstable fractures, progressive neurologic loss, spinal cord compression, infections, tumors, or failed conservative care typically require spine surgery/neurology input (UT Southwestern; Mayo Clinic). UT Southwestern Medical Center+1
Take-home message
High-impact events can injure the spine and the brain at the same time. Symptoms may range from neck/back pain to nerve symptoms, balance problems, and cognitive complaints. Integrative chiropractic care, coordinated with medical providers, can help reduce pain, restore movement, retrain the nervous system, and guide safe return to work and sport—while recognizing when urgent specialty care is needed (Mayo Clinic, 2024; NINDS, 2025; UTSW, n.d.; Jimenez, 2023–2025). El Paso, TX Doctor Of Chiropractic+3Mayo Clinic+3NINDS+3

References
-
Brommeland, T., Helseth, E., Aarhus, M., Moen, K. G., Dyrskog, S. E., Rydning, P. N., & Aarhus, M. (2018). Best practice guidelines for blunt cerebrovascular injury (BCVI). Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. BioMed Central
-
Cognitive FX. (2023, July 21). The long-term effects of whiplash: Causes & treatment. CognitiveFX
-
Converse, M. I., et al. (2019). Cerebral blood vessel damage in traumatic brain injury. CDC. CDC Stacks
-
Fehily, B., & Fitzgerald, M. (2017). Repeated mild traumatic brain injury. Frontiers in Neurology. PMC
-
Freire, M. A. M., et al. (2023). Cellular and molecular pathophysiology of traumatic brain injury. Biology. MDPI
-
Goriely, A., et al. (2015). Mechanics of the brain: Perspectives, challenges, and opportunities. Biomechanics and Modeling in Mechanobiology. SpringerLink
-
Jimenez, A. (2023). Chiropractic care after accidents and injuries | El Paso, TX. dralexjimenez.com. El Paso, TX Doctor Of Chiropractic
-
Jimenez, A. (2025). Sports head injuries: Chiropractic’s role. dralexjimenez.com. El Paso, TX Doctor Of Chiropractic
-
LeFever, D., & Caruso, R. (2023). Hangman’s fractures. StatPearls (NCBI Bookshelf). NCBI
-
Mayo Clinic. (2024, Aug 17). Spinal cord injury—Symptoms & causes. Mayo Clinic
-
Mayo Clinic. (2024, Aug 17). Spinal cord injury—Diagnosis & treatment. Mayo Clinic
-
McMordie, J. H., & Piche, J. (2023). Cervical spine fractures overview. StatPearls (NCBI Bookshelf). NCBI
-
NINDS. (2025, Apr 7). Spinal cord injury. NINDS
-
UT Southwestern. (n.d.). Brain and spine trauma. UT Southwestern Medical Center
-
UT Southwestern. (n.d.). Spine disorders and spine surgery. UT Southwestern Medical Center
-
Weill Cornell Medicine—Neurological Surgery. (n.d.). About brain and spine injuries. Weill Cornell Neurosurgery
-
BBGA. (2025). 10 common spinal injuries from car accidents. Blasingame & Ashley, P.C.
Author & clinical context
This article incorporates the integrative, team-based chiropractic perspective of Dr. Alexander Jimenez, DC, APRN, FNP-BC, who blends chiropractic care with nurse practitioner training for injury evaluation and rehabilitation in El Paso, Texas (Jimenez, 2023; Jimenez, 2025). El Paso, TX Doctor Of Chiropractic+1
Professional Scope of Practice *
The information herein on "Spine Injuries High Impact Accidents and Chiropractic Care" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card