Ankylosing spondylitis/AS is a common type of arthritis that can cause damage to spinal structures, body parts, and organs. Ankylosing spondylitis causes inflammation in the spine’s ligaments and joints which can cause affected vertebrae to fuse, but other symptoms/complications are skin disorders. Ankylosing spondylitis flare-ups can present with skin disorders like rashes and the possible development of skin diseases like psoriasis.
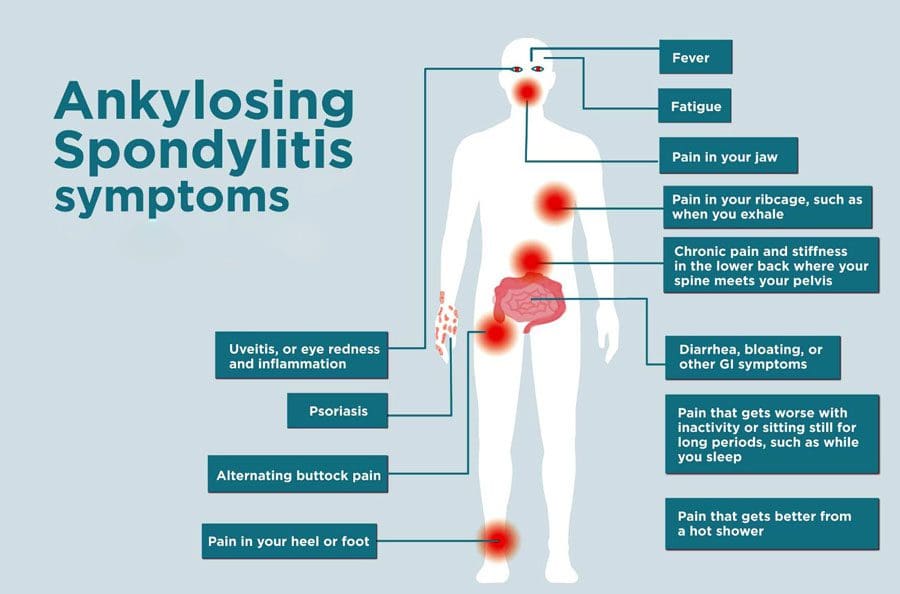
Table of Contents
Ankylosing Spondylitis
The inflammation causes back stiffness and pain that causes the spine to become inflexible and rigid. The vertebrae can fuse in extreme cases.
- It is typically seen in the early adult population as back pain and hip pain.
- Symptoms are more common in individuals between 17 and 45.
- Men are more likely to be affected than women.
- Genetics can play a role in this condition.
Doctors utilize multiple approaches to relieve symptoms and manage the condition through combined exercise, chiropractic, physical therapy, diet, and stress management to help improve quality of life.
Skin Disorders
A flare-up can present as a skin rash but can also affect the skin in other ways that include:
- Rashes brought on by medication treatments.
- Trouble healing from incisions after surgery.
Psoriasis
- Psoriasis presents as red skin patches appearing anywhere on the body.
- The most common areas are the scalp, palms, elbows, and knees.
- The affected skin can itch, become tender, and can also sting and burn.
- Some psoriasis outbreaks result in lesions or blisters.
Ankylosing Spondylitis vs. Psoriatic Arthritis
- Ankylosing spondylitis and psoriatic arthritis are related and come under spondyloarthritis/SpA rheumatic disease.
- Ankylosing spondylitis is typically localized to the spine, whereas psoriatic arthritis can affect almost any joint in the body and presents with tendinopathy.
- Some individuals with AS can begin to develop psoriasis.
Management
Doctors are currently treating psoriasis with multiple treatment options that can include:
- Topical agents such as vitamin D analogs.
- Corticosteroids can help with pain and swelling.
- Non-steroidal topical agents can be used for facial and flexible body parts like the armpits, elbows, and back of the knees.
- Light/phototherapy using narrow-band UV-B light.
- Medications can also help but can produce side effects.
Ankylosing spondylitis skin disorders present ongoing challenges. However, increasing treatment options are helping to minimize the condition’s impact on a better quality of life.
AS Causes, Symptoms, Diagnosis, Treatment
References
Meier, Katharina, et al. “Skin manifestations in spondyloarthritis.” Therapeutic advances in musculoskeletal disease vol. 12 1759720X20975915. 8 Dec. 2020, doi:10.1177/1759720X20975915
Myers, Elisha et al. “An Update on Narrowband Ultraviolet B Therapy for the Treatment of Skin Diseases.” Cureus vol. 13,11 e19182. 1 Nov. 2021, doi:10.7759/cureus.19182
National Institutes of Health. (n.d.) “Ankylosing spondylitis.” https://www.niams.nih.gov/health-topics/ankylosing-spondylitis
Ye, Chao, and Wenyuan Li. “Cutaneous vasculitis in a patient with ankylosing spondylitis: A case report.” Medicine vol. 98,3 (2019): e14121. doi:10.1097/MD.0000000000014121
Professional Scope of Practice *
The information herein on "Skin Disorders Ankylosing Spondylitis Sciatica Clinic" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card












