Table of Contents
Introduction
The body’s immune system is vital in protecting the body from foreign invaders that can wreak havoc. The immune system has a casual relationship with different body systems like the gut, endocrine, and central nervous systems that work together to keep the body functional. When environmental or genetic factors affect the body over time, the immune system will begin to attack normal, healthy cells causing issues and becoming a risk of developing autoimmune diseases. Autoimmune diseases are when the body starts to attack itself, and if it is not managed over time, it can lead to the development of chronic disorders. Today’s article looks at one of the most common autoimmune diseases, systemic lupus erythematosus or lupus, its symptoms and factors, and how to manage lupus with available treatments. We refer patients to certified providers specializing in autoimmune therapies to help those with systemic lupus and its associated symptoms. We also guide our patients by referring to our associated medical providers based on their examination when it’s appropriate. We find that education is the solution to asking our providers insightful questions. Dr. Alex Jimenez DC provides this information as an educational service only. Disclaimer
What Is Systemic Lupus Erythematosus?
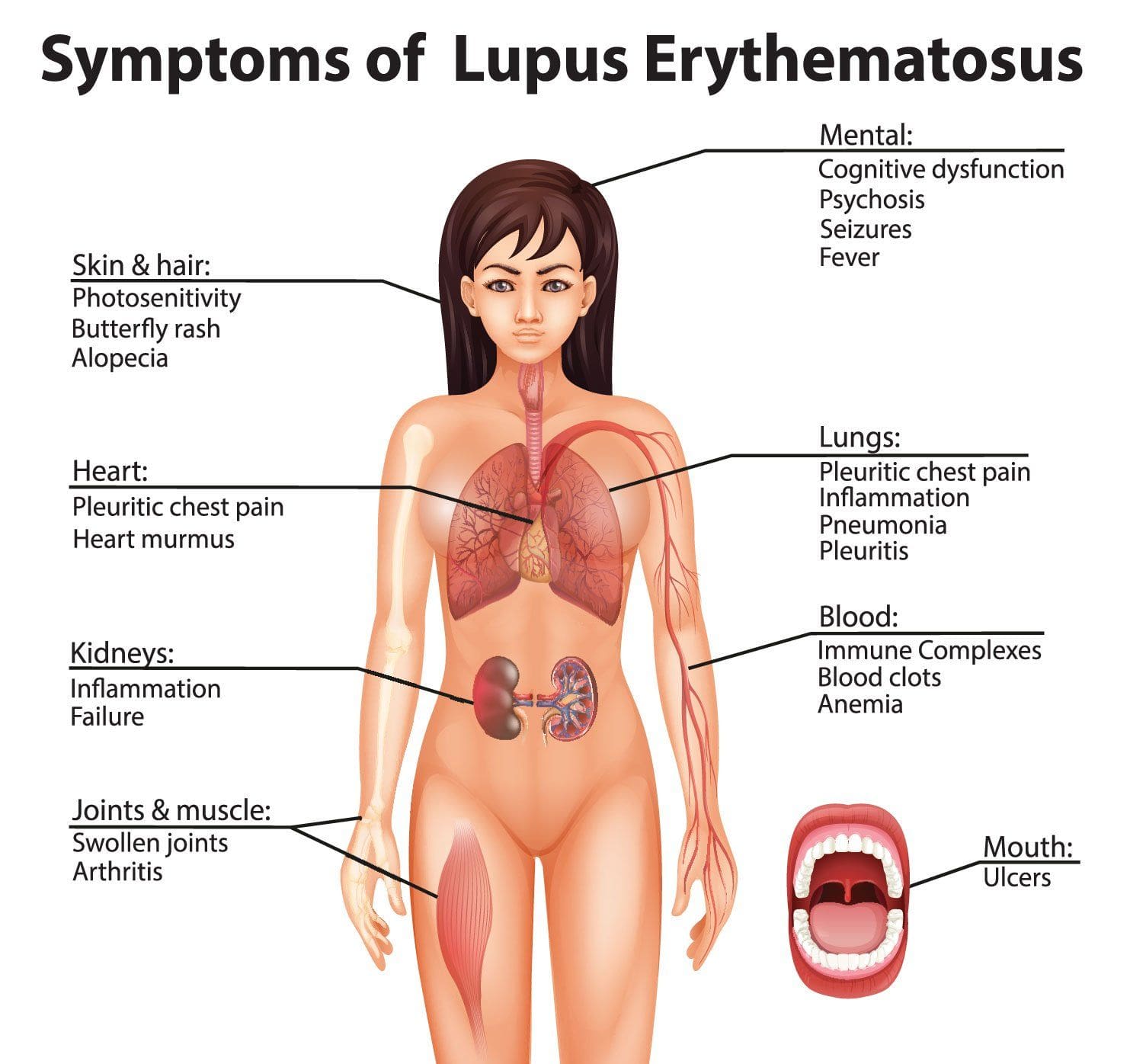
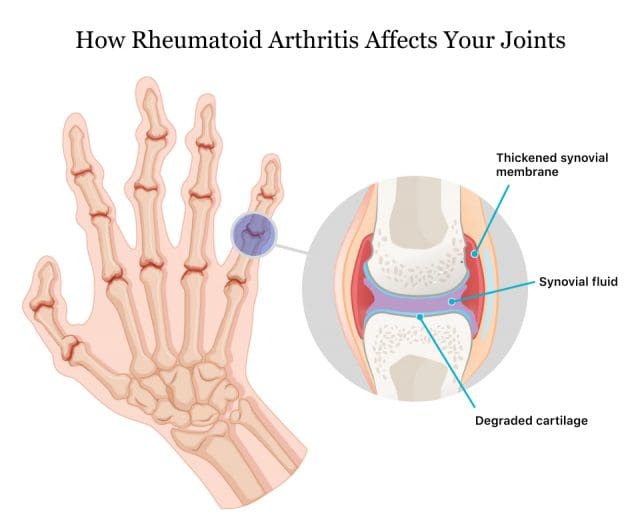
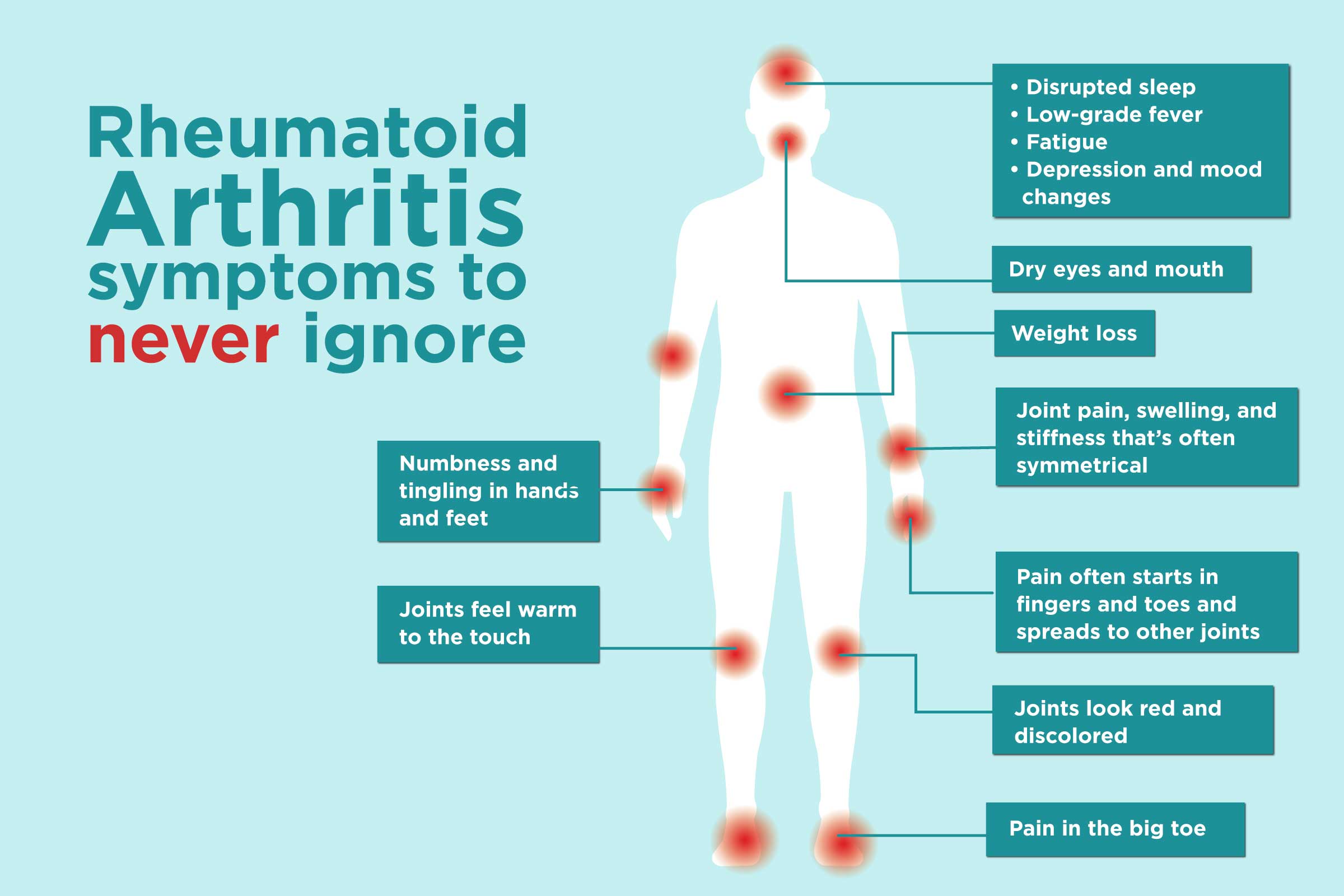
Are you experiencing fatigue? How about sharp pain located in your chest? Have you been experiencing headaches that seem to pop up for no reason? Some of these symptoms are signs that you could be at risk of developing lupus. Lupus or systemic lupus erythematosus is a systemic autoimmune disease with a multisystem involvement that occurs when an individual’s immune system starts to attack their tissue and organs. Systemic refers to multiple affected organs, lupus refers to various skin diseases, and erythematosus refers to inflamed, reddened skin. Studies reveal that lupus is a chronic inflammatory autoimmune disease affecting multiple organ systems and potentially associated with different factors. Lupus is tricky to diagnose because it often mimics other ailments like fibromyalgia, rheumatoid arthritis, and other autoimmune diseases; it can cause inflammation in the different body systems.
The Symptoms and Factors
Even though lupus is difficult to diagnose, the signs and symptoms vary for individuals who might be at risk of developing lupus. Some signs may suddenly appear or evolve, ranging from mild to severe depending on the factors. Some of the factors that are associated with lupus include:
- Sun exposure
- Lifestyle habits (stress, smoking, diet, physical inactivity)
- Toxins
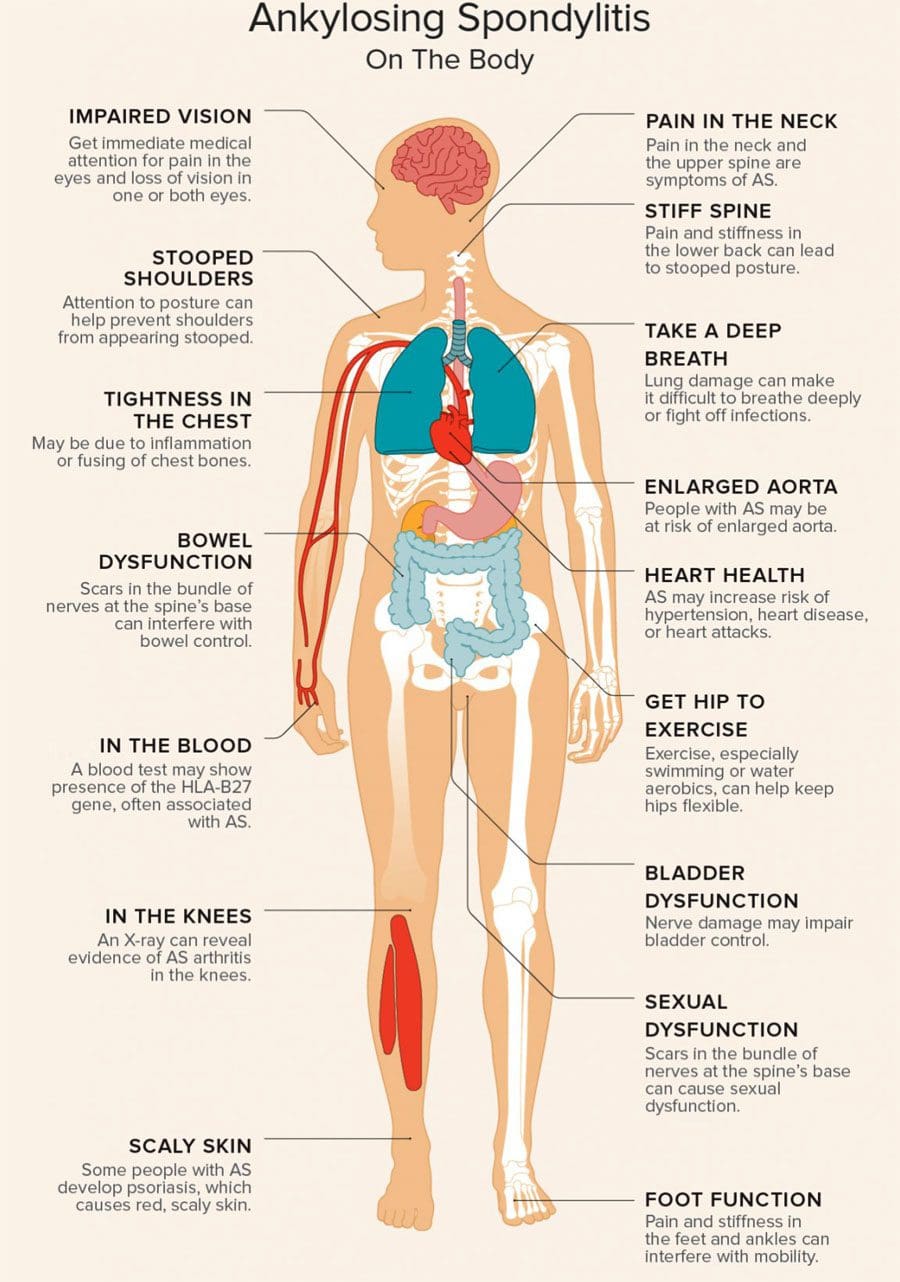
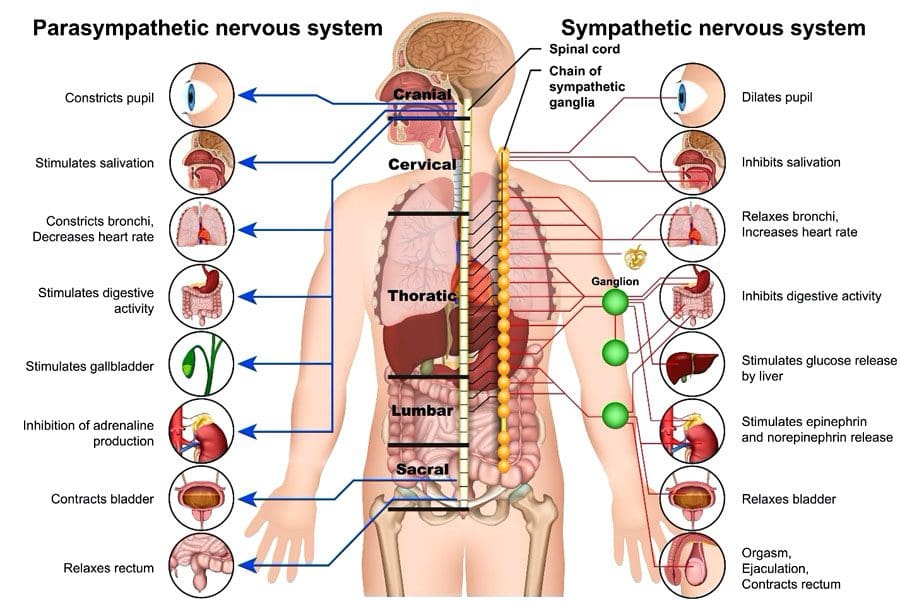
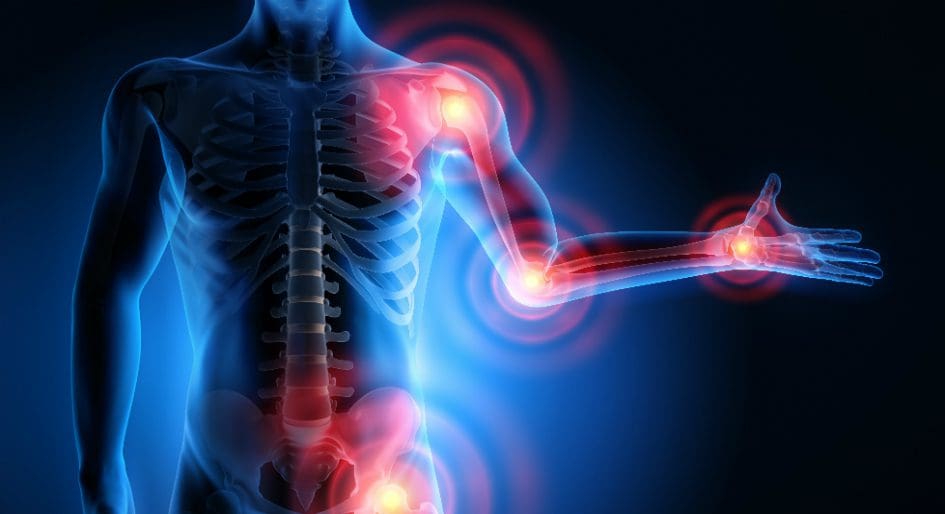
- Genetic (Family history)
Many of these factors contribute to the development of lupus and are closely associated with other autoimmune diseases like diabetes, RA (rheumatoid arthritis), and fibromyalgia. So how do these autoimmune diseases correlate with lupus? Since lupus can mimic other autoimmune disorders, some symptoms overlap, affecting the different body systems like the joints, skin, kidneys, blood cells, brain, heart, and lungs. For example, many autoimmune diseases are closely associated with inflammation, which could potentially be involved with the gut. Some of the symptoms that are associated with lupus include:
- Fatigue
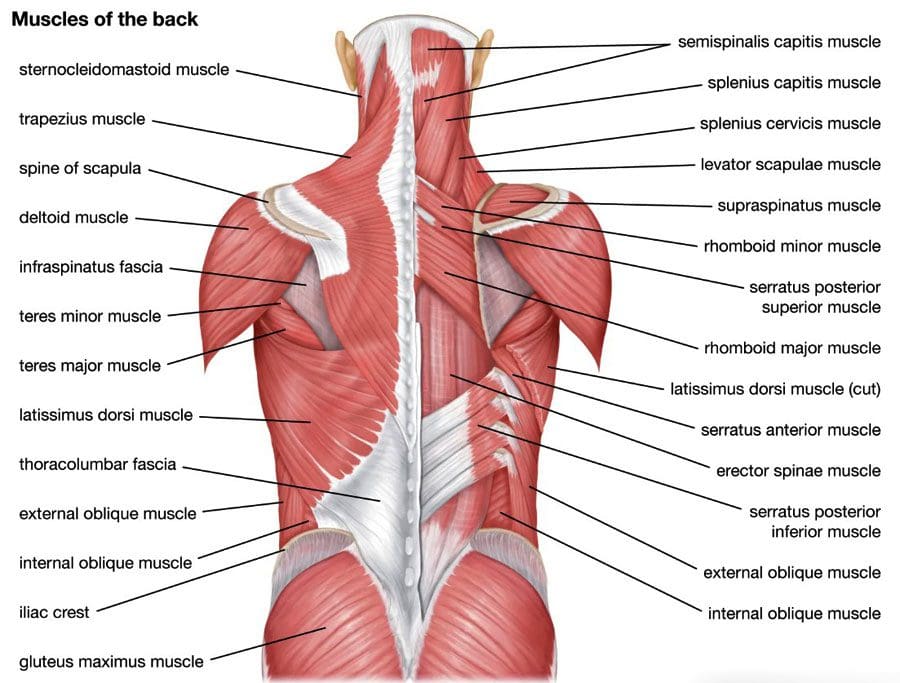
- Joint and muscle pain
- Headaches
- Butterfly rash
- Headaches
- Skin legions
- Stomach issues
Systemic Lupus Erythematosus Overview-Video

Have you been experiencing issues with your gut? How about joint stiffness and swelling? Or are you constantly feeling the effects of fatigue? Many of these symptoms are associated with lupus, and the video above explains what systemic lupus erythematosus is and how it affects the body. Lupus is an autoimmune disease that is difficult for physicians to diagnose since it mimics other issues that a person may be experiencing. An example would be fibromyalgia associated with lupus. Studies reveal that the presence of fibromyalgia could be a separate diagnosis or potentially be involved with lupus as a confounder. In fibromyalgia and lupus, somatic symptoms like fatigue, aching, and pain may overlap and affect the surrounding muscles and organs. This is known as somato-visceral pain. Fortunately, there are ways to manage autoimmune diseases like lupus.
Treatments To Manage Lupus
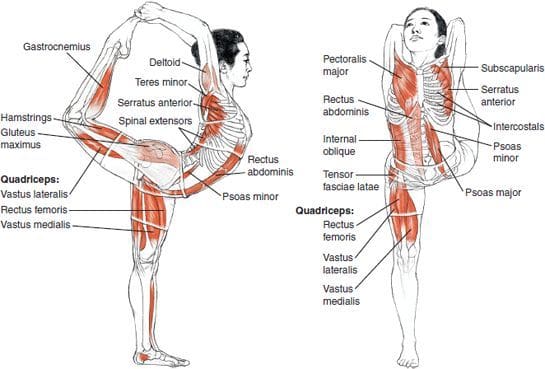
When a person is dealing with an autoimmune disease like lupus, it may feel like it is the end of the world to them. While there is no cure for lupus, there are ways to manage this autoimmune disease from progressing further to causing more damage to the body. Making small changes in food intake, adding more supplements to boost the immune system like vitamin D, exercising, and chiropractic care work together to manage autoimmunity in the body. So how do all these things work together? Well eating anti-inflammatory foods filled with antioxidants to dampen inflammatory effects. Supplements like vitamin D can help improve and maintain a healthy immune system. Chiropractic care not only focuses on the musculoskeletal system but can help the immune system to its total capacity by correcting any subluxations or spinal misalignments in the body.
Conclusion
The immune system helps the body by attacking foreign invaders that wreak havoc inside while having a casual relationship with different body systems. When environmental or genetic factors affect the body over time, the immune system mistakenly attacks normal, healthy cells thinking they are foreign invaders. This is known as autoimmune disease and, if not managed over time, can lead to the development of chronic disorders. Lupus is an autoimmune disease that can mimic other chronic conditions, making it tricky to diagnose. Some of the overlapping symptoms associated with lupus can vary in severity. While there is no cure for lupus, available treatments can help manage the symptoms and associated conditions. Combining healthy eating habits, exercise, vitamin intake, and chiropractic care can help improve a person’s health and wellness.
References
Justiz Vaillant, Angel A, et al. “Systemic Lupus Erythematosus – Statpearls – NCBI Bookshelf.” In: StatPearls [Internet]. Treasure Island (FL), StatPearls Publishing, 15 Mar. 2022, https://www.ncbi.nlm.nih.gov/books/NBK535405/.
Maidhof, William, and Olga Hilas. “Lupus: An Overview of the Disease and Management Options.” P & T : a Peer-Reviewed Journal for Formulary Management, MediMedia USA, Inc., Apr. 2012, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3351863/.
Wolfe, Frederick, et al. “Fibromyalgia, Systemic Lupus Erythematosus (SLE), and Evaluation of SLE Activity.” The Journal of Rheumatology, U.S. National Library of Medicine, Jan. 2009, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2944223/.