Table of Contents
Introduction
Everyone has different tips and tricks for being healthy and losing weight. Many individuals incorporate other diets, eating habits, and exercise regimes to lose excess weight, have energy throughout the day and feel good. One of the other diets many people seem to lean toward when it comes to losing weight and helping the body is detox. Surprisingly, many people seem misinformed about detox and dieting being the same; however, they are not, as detoxing is a natural process of body purification while dieting incorporates healthy eating habits, exercising, and healthy life choices. For the body, the best detoxing machine is the liver. Today’s article looks at how the liver detoxes the body, how factors can cause detox imbalances in the body, and how different food helps liver detoxification. We refer patients to certified providers specializing in liver or gastrointestinal treatments to help many individuals with liver issues. We also guide our patients by referring to our associated medical providers based on their examination when it’s appropriate. We find that education is the solution to asking our providers insightful questions. Dr. Alex Jimenez DC provides this information as an educational service only. Disclaimer
The Body’s Own Detox Machine: The Liver
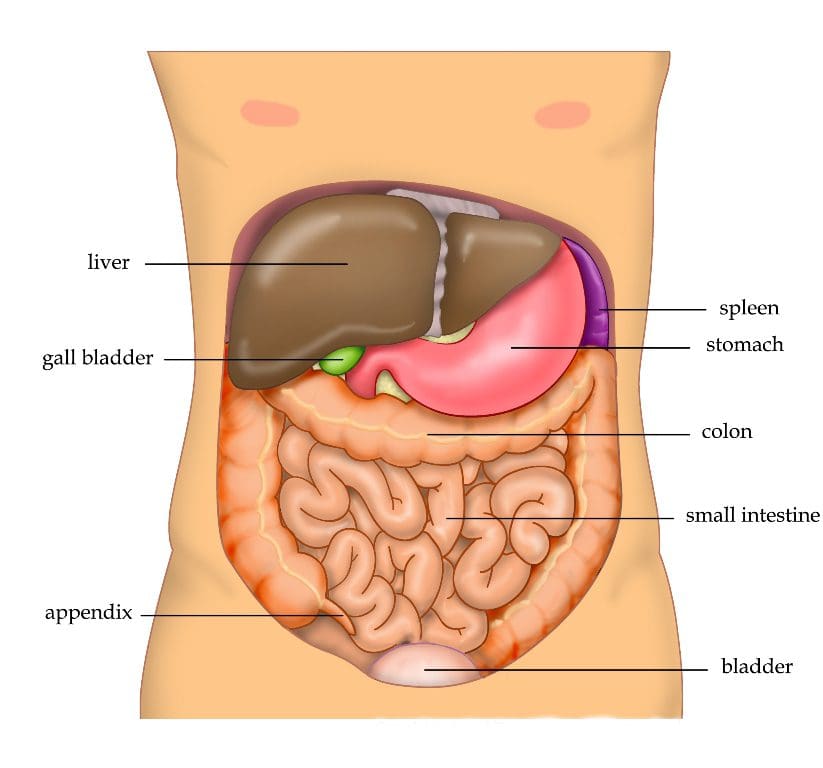
Have you been experiencing gut sensitivities from the foods you eat? How about experiencing chronic fatigue throughout the entire day? What about experiencing pain and swelling in your abdominals or legs? Some of these issues may indicate that something is wrong with your liver. The liver is the most crucial organ with a massive responsibility for the vast array of functions of the body. The liver helps support many visceral functions like maintaining the body’s metabolism, immunity, digestion, and detoxification. Detoxification is a biochemical process where non-water-soluble compounds are transformed into water-soluble compounds flushed out of the body. The benefit of detox is that it helps protect the body from adverse effects of external and internal toxins.
Since the liver is a massive organ, its essential role in the body is detoxification. Studies reveal that the detoxification process for the liver is in two phases. Phase 1 activated the enzymes in the body to prepare the substance to be removed. Phase 2 excretes the enzymes out of the body as urine, stool, and bile. These two phases help keep the body healthy and stop excessive toxins from harming the rest of the body.
The Lymphatic System
The lymphatic system is one of the central detoxification systems responsible for allowing waste products to leave and be carried away to the bloodstream, becoming one of the defense mechanisms for the body and purifying the body fluids for proper functioning. The lymphatic vasculatures also play an active role in immune regulation by impacting inflammatory and immune responses. This means that the lymphatic will produce white blood cells to attack foreign invaders entering the body.
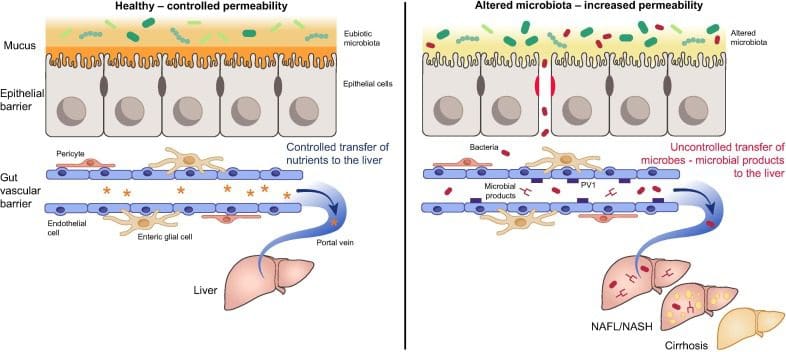
The Gut-Liver Axis
Since the liver is the master organ for detoxification, what is its relationship with the gut? Well, studies reveal that the gut microbiota forms a complex microbial community that significantly impacts human health. The gut microbiota can indirectly modulate the functionality of the extra-intestinal organs, which involves the liver. The gut connects to the liver with the intestines through bile acid metabolism. When there is a decrease in bile acid in the gut, it could trigger hepatic inflammation via inflammasomes. Inflammasomes are an essential component of innate immune response while being critical for the clearance of pathogens or damaged cells. When the inflammasomes start becoming mediators for hepatic inflammation, they could potentially be involved with detoxification imbalances in the body.
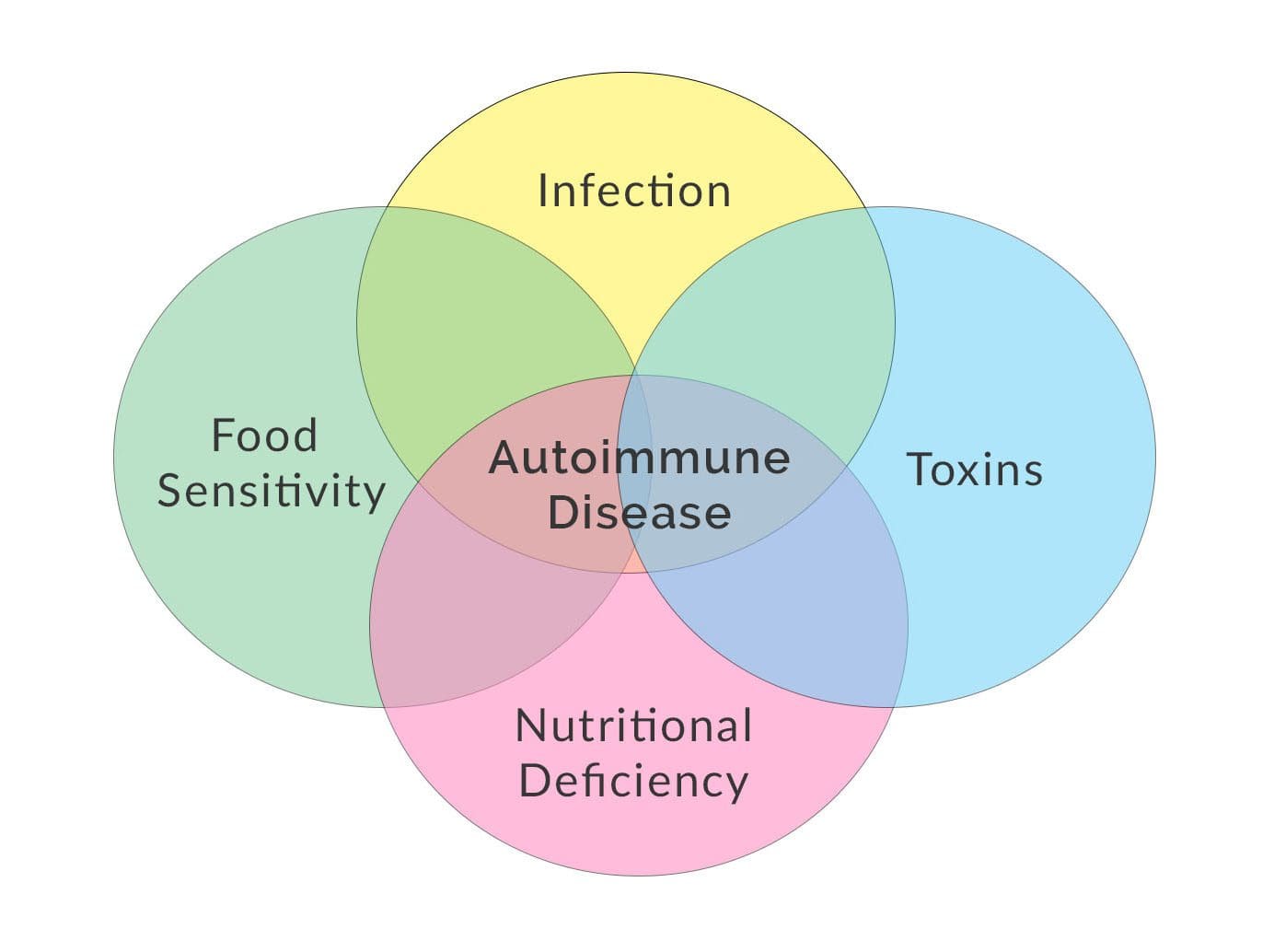
Detoxification Imbalances
When there are decreased bile acids in the gut, the body could be at risk of developing intestinal dysbiosis. This causes impaired intestinal barrier function, which overlaps to leaky gut and aggravates hepatic inflammation in the liver. When this happens, toxins in the body become excessive and may cause immune and nervous system abnormalities while triggering imbalanced detoxification symptoms that correspond to issues similar to chronic conditions. Some of these detoxification imbalances include:
- Fatigue
- Allergies/intolerances
- Sluggish metabolism
- Weight gain easily
- Intolerance to fats
- Puffy – excess fluid
- Body odor, bad breath, metallic taste
- Profuse sweating even in cool weather
Naturally Detoxing Your Body-Video

Have you been dealing with allergies or food intolerances affecting your abdominals? Have you been feeling sluggish? What about feeling chronic fatigue throughout the entire day? Some of these symptoms are signs that your liver could suffer from some issues. The liver’s primary function in the body is to detoxify the body. The video above explains how the liver detoxifies the body and how drinks to cleanse the body don’t add additional benefits. The best way for a healthy liver to be functional and detox the body naturally is by eating the right foods that help support the liver, exercising regularly, drinking plenty of water to flush out the system, and getting adequate sleep.
Foods That Support Liver Detoxification
When it comes to supporting the liver, eating the right foods can provide energy and reduce inflammatory effects on the body. Studies reveal that eating various wild and semidomestic food plants can provide various components to liver function. Plants like dandelions contain taxasterols, which have antioxidant and anti-inflammatory properties that allow the liver to increase bile secretion. Other foods that help with liver functionality associated with other body functions include:
- Berries (blueberries & cranberries)
- Grapefruit
- Prickly pear
- Cruciferous vegetables
- Garlic
- Carrots
- Beets
- Olive oil
- Nuts
Incorporating these healthy foods can not only be beneficial to the liver but can help the major organs and body to receive the nutrients that the body deserves.
Conclusion
The liver is a massive organ that helps the body to function correctly by harmful detoxifying pathogens through excretion. As a natural detoxifying machine, the liver has a casual relationship with the gut system by filtering the nutrients and transporting them out to different body areas. Harmful pathogens enter the body and disrupt the liver can lead to dysbiosis and liver dysfunction. Fortunately, there are nutritious foods that can help support the liver and even help flush out the toxins over time so the body can begin its healing process naturally.
References
Grant, D M. “Detoxification Pathways in the Liver.” Journal of Inherited Metabolic Disease, U.S. National Library of Medicine, 1991, https://pubmed.ncbi.nlm.nih.gov/1749210/.
Guan, Yong-Song, and Qing He. “Plants Consumption and Liver Health.” Evidence-Based Complementary and Alternative Medicine : ECAM, Hindawi Publishing Corporation, 2015, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4499388/.
Karla, Arjun, et al. “Physiology, Liver – Statpearls – NCBI Bookshelf.” In: StatPearls [Internet]. Treasure Island (FL), StatPearls Publishing, 8 May 2022, https://www.ncbi.nlm.nih.gov/books/NBK535438/.
Konturek, Peter Christopher, et al. “Gut⁻Liver Axis: How Do Gut Bacteria Influence the Liver?” Medical Sciences (Basel, Switzerland), MDPI, 17 Sept. 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6165386/.
Sharma, Deepika, and Thirumala-Devi Kanneganti. “The Cell Biology of Inflammasomes: Mechanisms of Inflammasome Activation and Regulation.” The Journal of Cell Biology, The Rockefeller University Press, 20 June 2016, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4915194/.