Table of Contents
Introduction
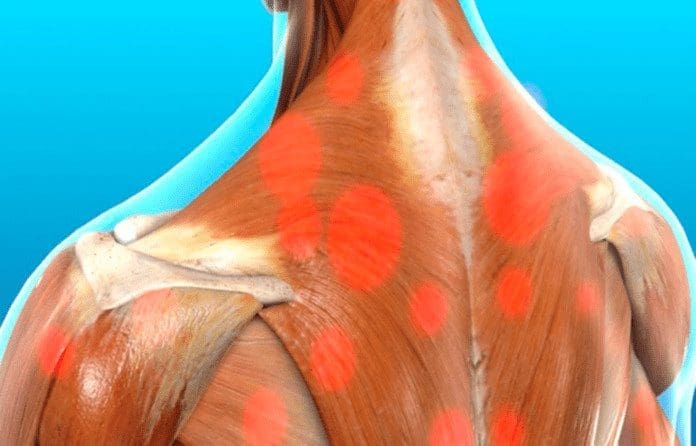
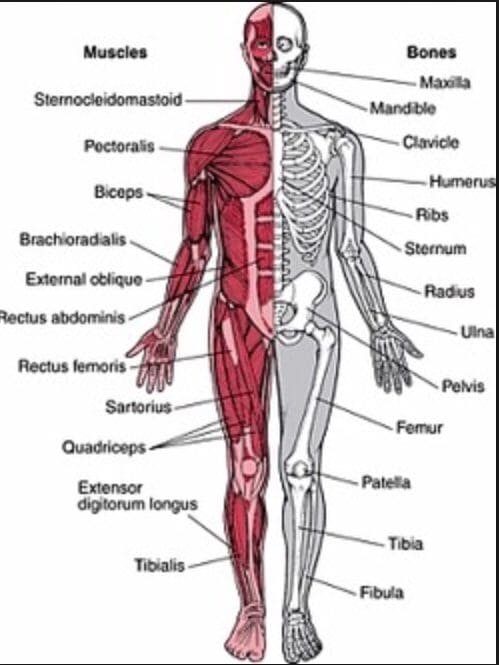
The body incorporates different muscles that have specific jobs to help mobilize the skeletal joints while providing function to the arms, neck, legs, and back. Many individuals use their muscles for everyday uses like lifting and carrying objects, moving from one place to another, and protecting vital organs from damage. To that point, issues like traumatic events, injuries, and environmental factors can affect the body and cause damage to the muscles. When the muscles are affected by these factors, tiny knots can form along the taut muscle band that can cause painful symptoms that affect specific areas in the body. One of the muscles affected by pain is the trapezius muscle, known as the “coat hanger” muscle, which can be associated with chronic symptoms of myofascial pain syndrome. Today’s article examines the trapezius muscle, how myofascial pain affects the trapezius muscle, and how to manage myofascial trapezius pain. We refer patients to certified providers specializing in musculoskeletal treatments to aid individuals suffering from trapezius muscle pain associated with myofascial pain. We also guide our patients by referring them to our associated medical providers based on their examination when it’s appropriate. We find that education is the solution to asking our providers insightful questions. Dr. Jimenez DC provides this information as an educational service only. Disclaimer
What Is The Trapezius Muscle?
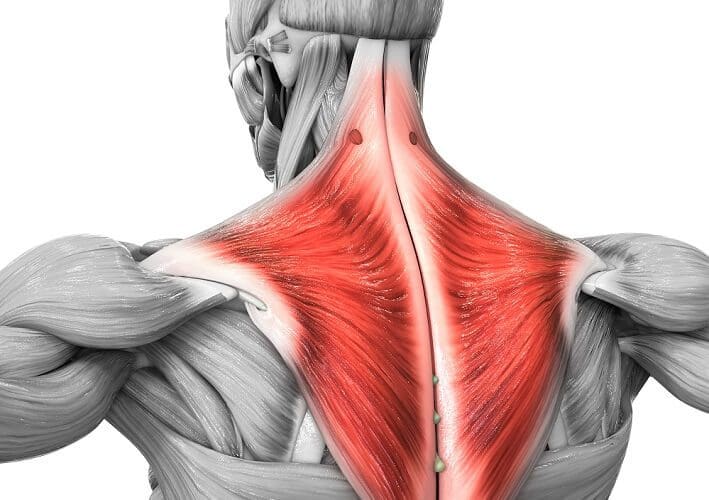
Have you experienced pain in your neck, shoulders, or mid-upper back? Do you feel headaches occurring near your temples? What about tenderness in certain areas of your body? Some of these symptoms may appear in your trapezius muscles. The trapezius muscle is located across the back that looks like a simple trapezoid with upper, middle, and lower muscle fibers that have different functions for the upper-middle back, shoulders, and neck. While the entire trapezius muscle helps rotates, elevate, and retract the scapula while extending the head and neck, and turning the chin by itself. At the same time, the entire muscle can help with assisting the extension of the cervical and thoracic spine.
- Upper Trapezius muscles: allow the shoulders to rise, bend the head and neck, and help support the weight of the upper extremities of the body, including the arms.
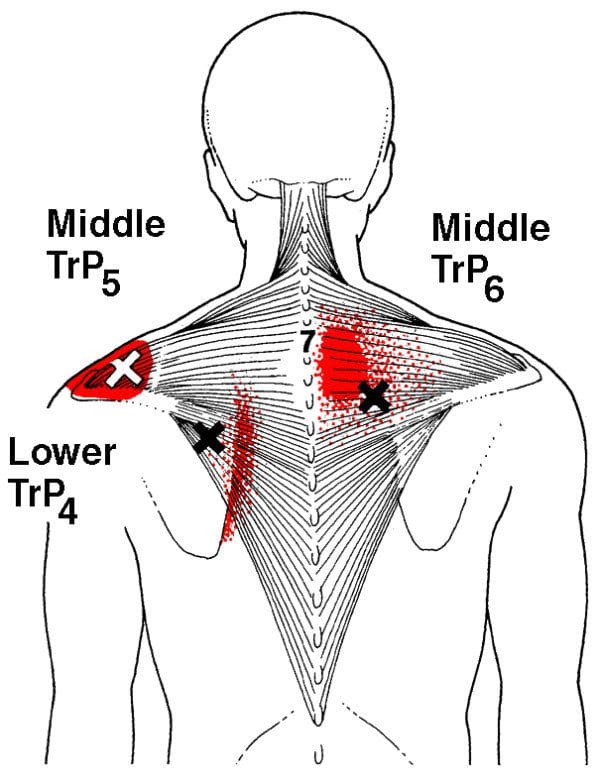
- Middle Trapezius muscles: assist with flexion and abduction of the arms around the shoulders at a nearly full range.
- Lower Trapezius muscles: Helps retract the scapula while rotating the glenoid fossa upwards by decompressing the vertebral borders of the scapula. These fibers help assist the flexion and abduction of the arms.
When traumatic forces or injuries affect the trapezius muscles, painful symptoms begin to affect the muscles, causing them to be tender to the touch and affecting different areas in the body.
How Does Myofascial Pain Affect The Trapezius Muscle?
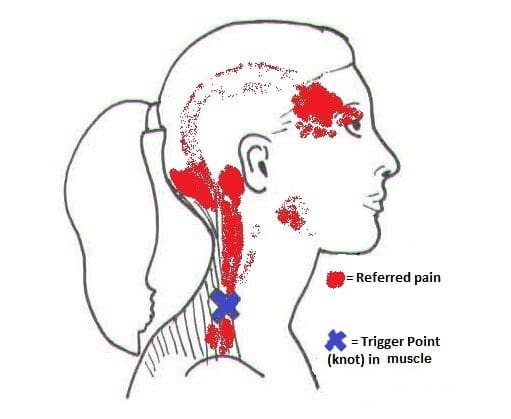
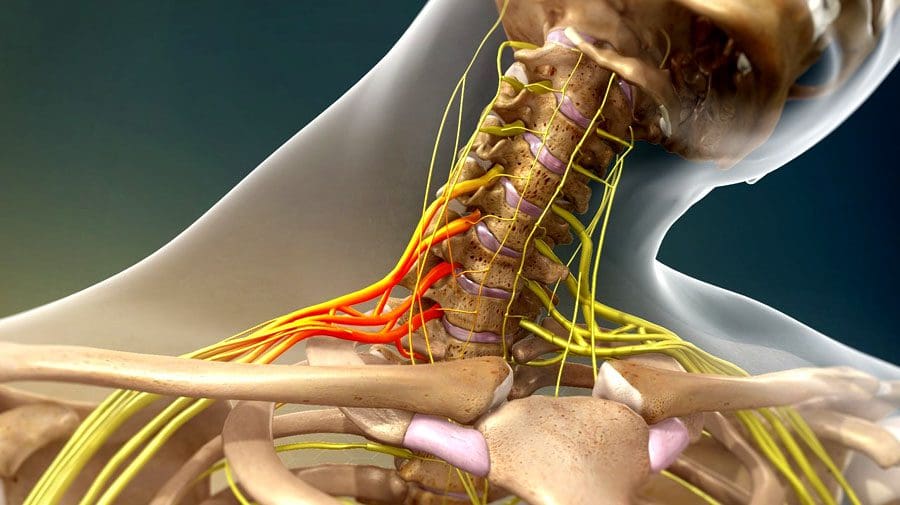
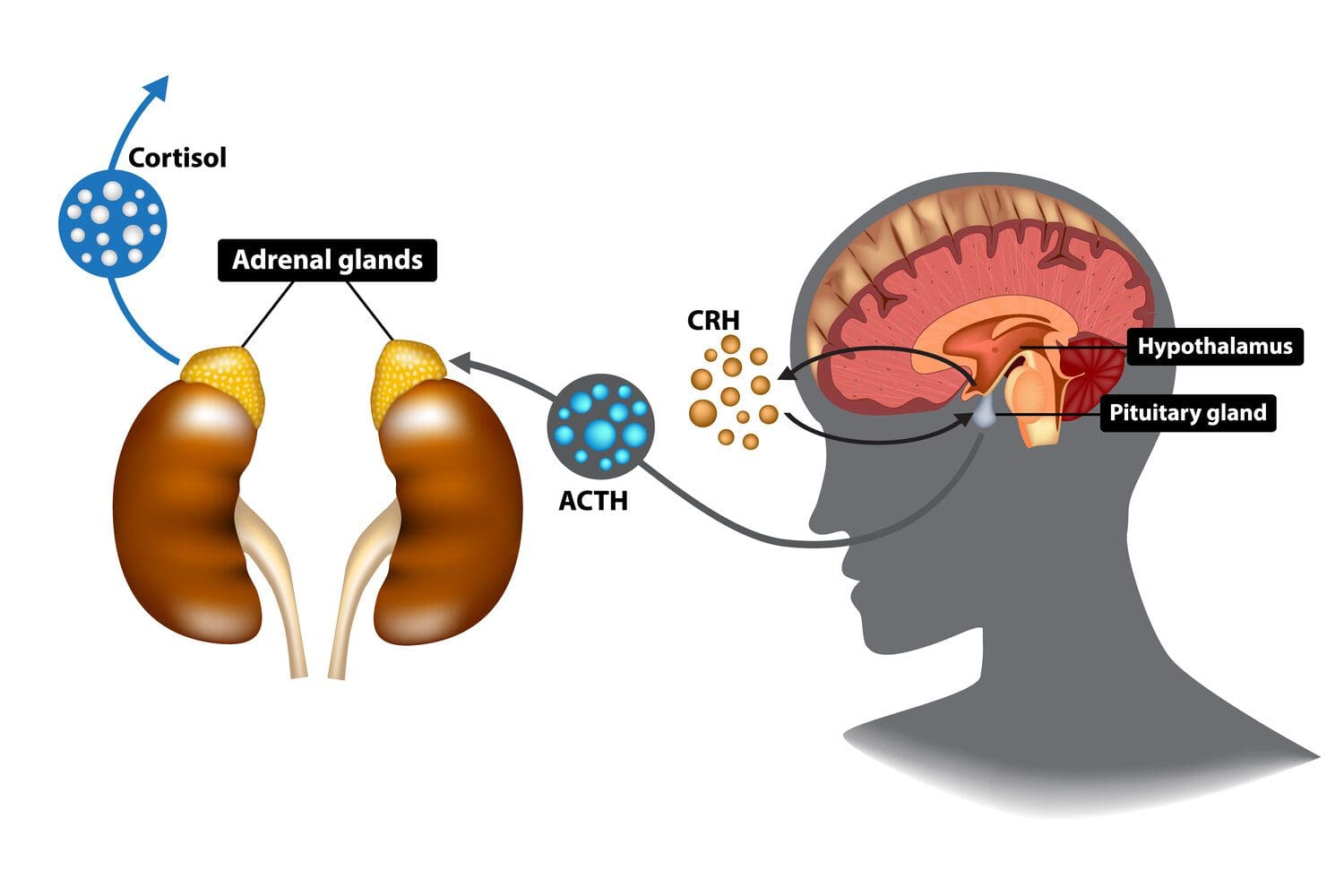
When traumatic forces or injuries affect the trapezius muscles, certain parts of the shoulders, neck, and upper-mid back will experience pain-related symptoms. When people experience headaches and shoulder and neck pain in their bodies while feeling tenderness in their trapezius muscles, this is known as referred pain associated with myofascial pain. Myofascial pain is when tiny knots along the taut muscle bands begin to make the muscle area tender to the touch. Individuals who suffer from myofascial pain in their trapezius muscles might experience hyperirritable spots that inflict pain and motor dysfunction. Studies reveal that individuals who work in food services may have symptoms of shoulder pain associated with myofascial pain due to repetitive motions on the upper trapezius muscles affecting their upper bodies. Myofascial trigger pain is a bit challenging to diagnose since the pain can be in different locations and mimic various ailments in the body. To that point, when the trapezius muscles are affected by trigger pain may potentially be involved with cervical myofascial pain. Cervical myofascial pain is a disorder that causes pain from muscle overuse or trauma in the neck. When the pain affects the neck muscles, it can travel down to the trapezius muscles causing tenderness and sensitivity in the affected muscle area. Stress, postural mechanics, or repetitive movements can develop myofascial pain syndrome and affect the surrounding muscles.
Trapezius Trigger Points- Video

Have you felt sore around your shoulders, neck, and upper-mid back? What about muscle tenderness in certain areas of your body? Do you feel tension along your neck or near the temples of your head? If you have been dealing with any of these symptoms, then you might be experiencing myofascial trapezius pain. The video above explains how trigger points from traumatic events can affect the trapezius muscle and cause referred pain that overlaps other conditions that may affect the body. Studies reveal that trigger points in the head and neck muscles of many suffering individuals have tension-type headaches. Tension-type headaches are one of the symptoms associated with myofascial trapezius pain. Some of the other symptoms related to myofascial pain affecting the trapezius muscle include:
- Deep aching pain
- Stiffness
- Muscle spasms
- Tightness around the shoulder and neck
- Tenderness along the shoulders, neck, and upper back
- Occipital headaches
How To Manage Myofascial Trapezius Pain
When many individuals suffer from myofascial trapezius pain, many would go to their primary doctor and explain to them that they are experiencing tension headaches constantly. Since myofascial pain is associated with the trapezius muscle is a bit complex and challenging for doctors to diagnose since every person’s pain is different. Many doctors will refer their patients to associated specialists like physical therapists, massage therapists, or chiropractors to determine where the pain is located along the trapezius muscle. Different treatments can help alleviate stiff muscles, and studies reveal that spinal manipulative therapy can help manage chronic pain from myofascial origins. Spinal subluxations or misalignment could potentially involve the corresponding spinal nerve root causing antinociceptive effects to the tender muscle, thus causing pain to the trapezius muscle. Utilizing various treatments to treat myofascial trapezius pain can provide individuals with beneficial relief from their pain along with managing their associated symptoms.
Conclusion
The trapezius muscle is a large superficial trapezoid-shaped muscle located in the back. The upper, middle, and lower muscle fibers have different functions in the head, neck, shoulders, and arms. The trapezius muscle also helps with assisting the extension of the cervical and thoracic spine. When traumatic events or injuries affect the trapezius muscle, it can be developed over time to create trigger points along the taut muscle band of the trapezius muscle and cause referred pain to the upper extremities of the body. Luckily various treatments can help manage the associated pain symptoms from myofascial trapezius pain and can help many individuals get back on their health and wellness journey.
References
Fernández-de-Las-Peñas, César, et al. “Myofascial Trigger Points and Their Relationship to Headache Clinical Parameters in Chronic Tension-Type Headache.” Headache, U.S. National Library of Medicine, Sept. 2006, https://pubmed.ncbi.nlm.nih.gov/16942471/.
Hwang, Ui-Jae, et al. “Predictors of Upper Trapezius Pain with Myofascial Trigger Points in Food Service Workers: The Strobe Study.” Medicine, Wolters Kluwer Health, June 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5500039.
Laframboise, Michelle A, et al. “Effect of Two Consecutive Spinal Manipulations in a Single Session on Myofascial Pain Pressure Sensitivity: A Randomized Controlled Trial.” The Journal of the Canadian Chiropractic Association, Canadian Chiropractic Association, June 2016, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4915475/.
Ourieff, Jared, et al. “Anatomy, Back, Trapezius – StatPearls – NCBI Bookshelf.” In: StatPearls [Internet]. Treasure Island (FL), StatPearls Publishing, 26 July 2021, https://www.ncbi.nlm.nih.gov/books/NBK518994/.
Touma, Jeffrey, et al. “Cervical Myofascial Pain – Statpearls – NCBI Bookshelf.” In: StatPearls [Internet]. Treasure Island (FL), StatPearls Publishing, 4 July 2022, https://www.ncbi.nlm.nih.gov/books/NBK507825/.