Table of Contents
Introduction
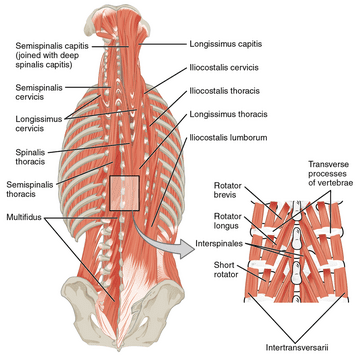
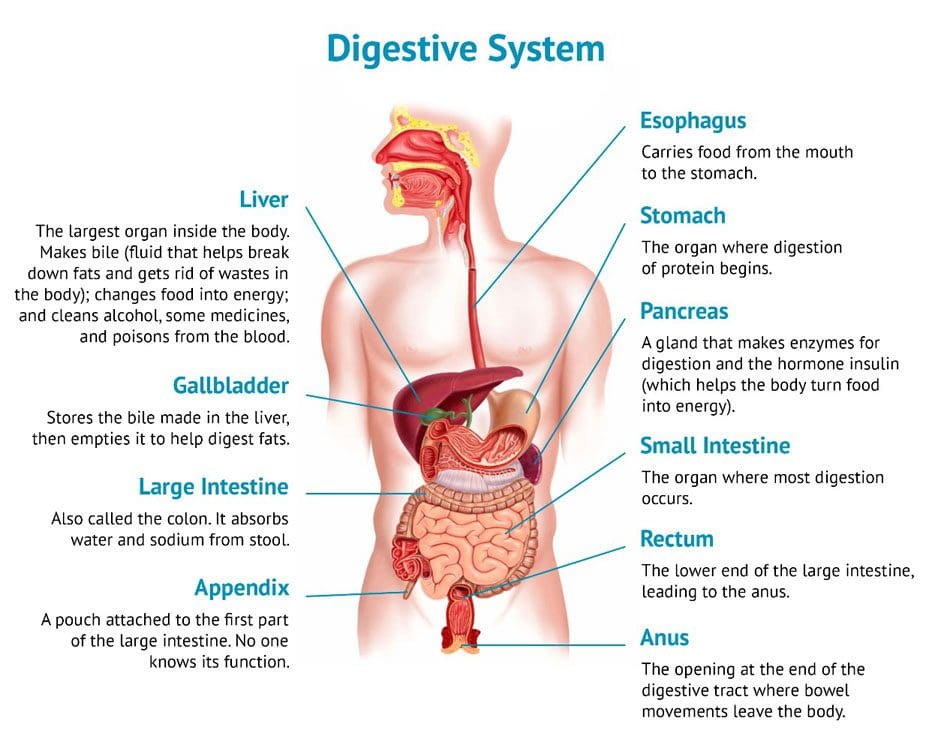
When it comes to the torso is surrounded by various muscles that help protect the vital organs known as the gut system and help with stabilizing the spinal column in the body. The abdominal muscles are essential to maintaining good posture and core support for many individuals. When normal activities or chronic issues begin to affect the body, the abdominal muscles can also be affected and can cause referred pain all around the torso area. When the abdominal muscles are dealing with referred pain, it can develop into trigger points that mask other chronic conditions affecting the torso and the thoracolumbar region. Today’s article looks at the abdominal muscles and their function, how trigger points are affecting the abdomen, and how various treatments help manage trigger points associated with abdominal pain. We refer patients to certified providers who provide different techniques in abdominal pain therapies related to trigger points to aid many suffering from pain-like symptoms along the abdominal muscles along the torso. We encourage patients by referring them to our associated medical providers based on their examination when it is appropriate. We designate that education is a great solution to asking our providers profound and complex questions at the patient’s request. Dr. Alex Jimenez, D.C., notes this information as an educational service only. Disclaimer
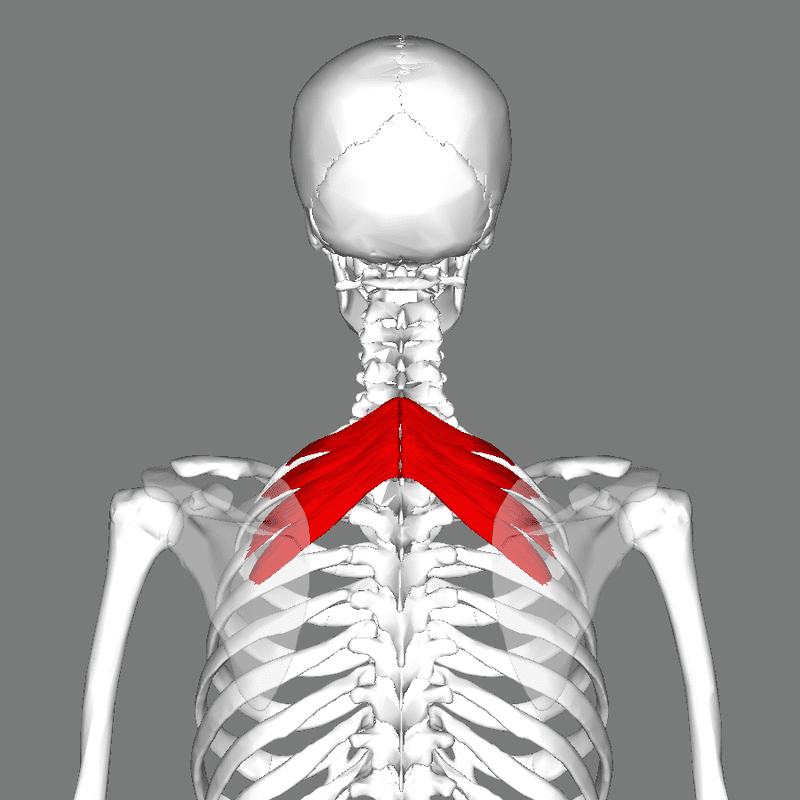
The Abdominal Muscles & Their Function
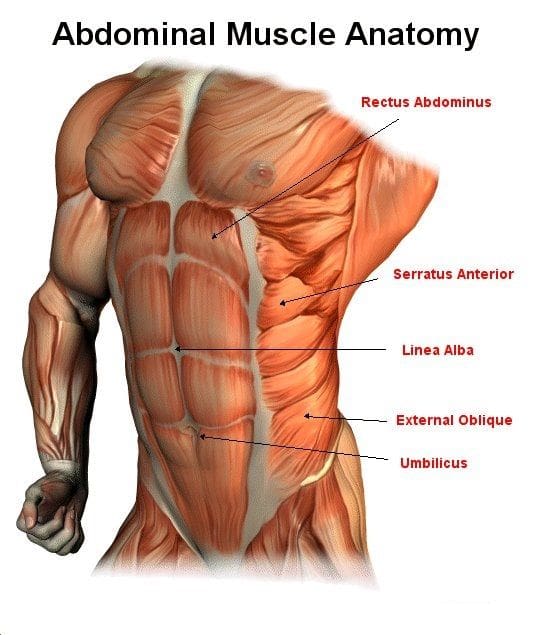
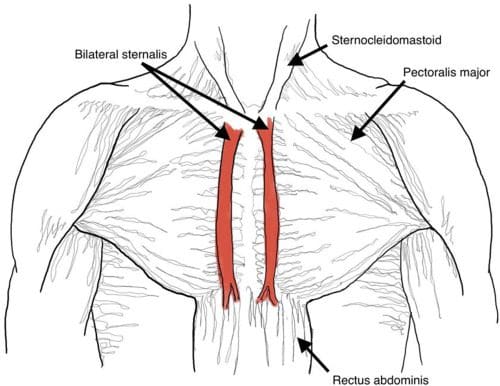
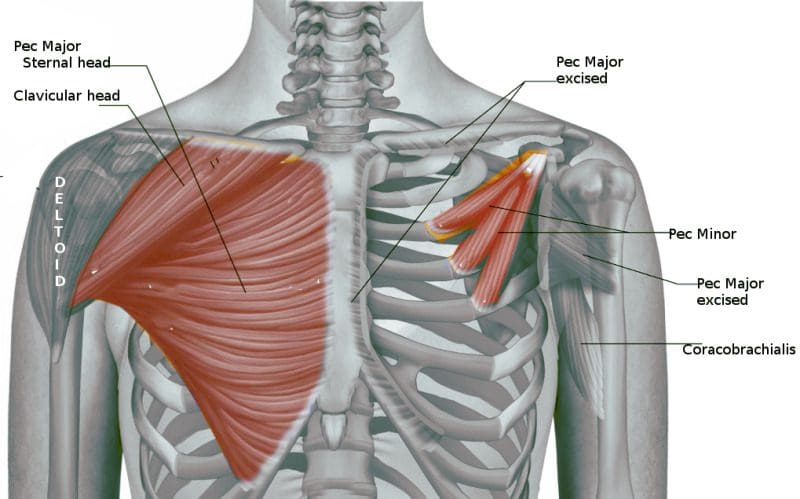
Do you have trouble moving around? Have you been dealing with muscle spasms along your abdomen? Does it hurt when you are sneezing, laughing, or coughing constantly? All these actions affecting your abdominal muscles might correlate with trigger points along the muscles and disrupt the torso area. The abdomen in the body has various muscles, a complex organ with many functions that contribute to a person’s quality of life. The abdominal muscles have many important parts, from supporting the trunk, allowing movement like twisting and turning, and holding the organs in the gut system in place through internal abdominal pressure regulation. The abdominal muscles have five main muscles that work together with the back muscles to keep body stability. They are:
- Pyramidalis
- Rectus Abdominus
- External Obliques
- Internal Obliques
- Transversus Abdominis
Studies reveal that the abdominal muscles can help increase the stability of the lumbar region of the body from the vertebral columns by tending the thoracolumbar fascia and raising the intra-abdominal pressure. This allows the abdominal muscle to bend and flex in different positions without feeling pain. However, overusing the abdominal muscles can lead to unnecessary issues that can affect not only the torso but the surrounding muscles around the torso.
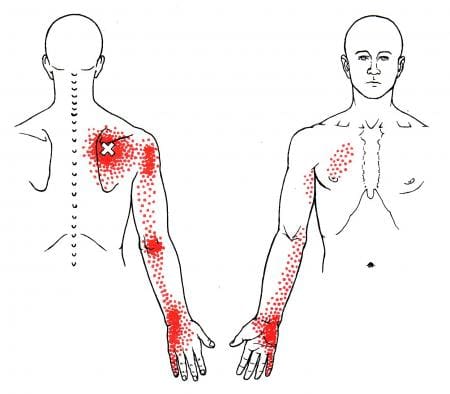
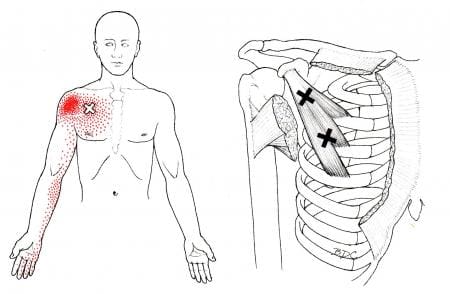
How Trigger Points Are Affecting The Abdomen
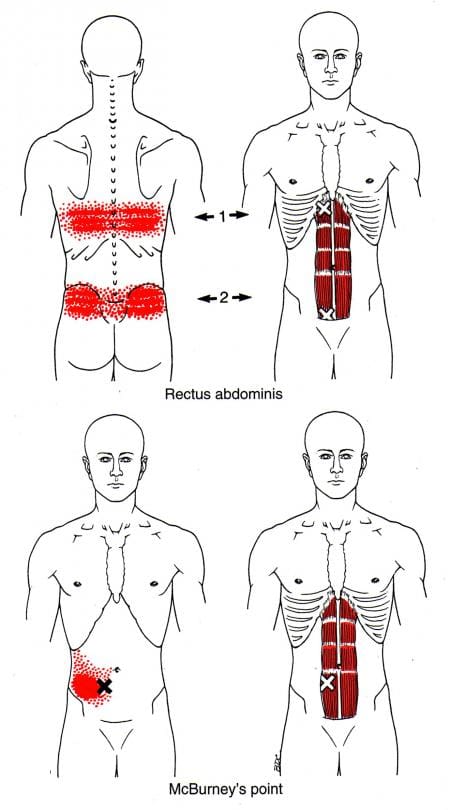
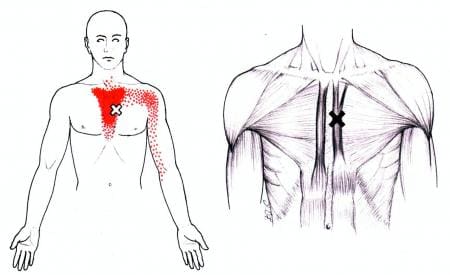
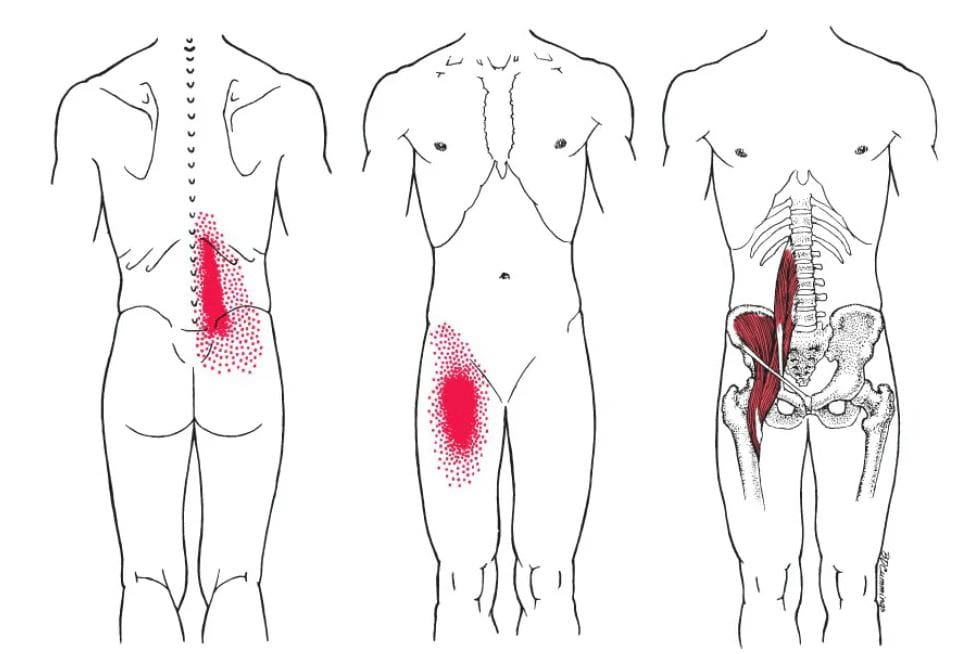
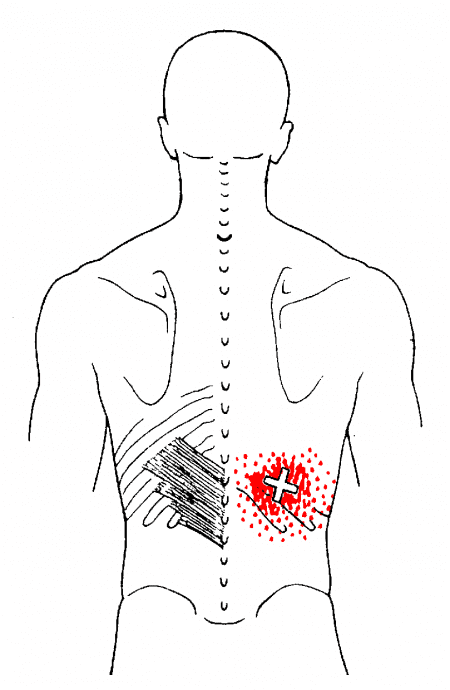
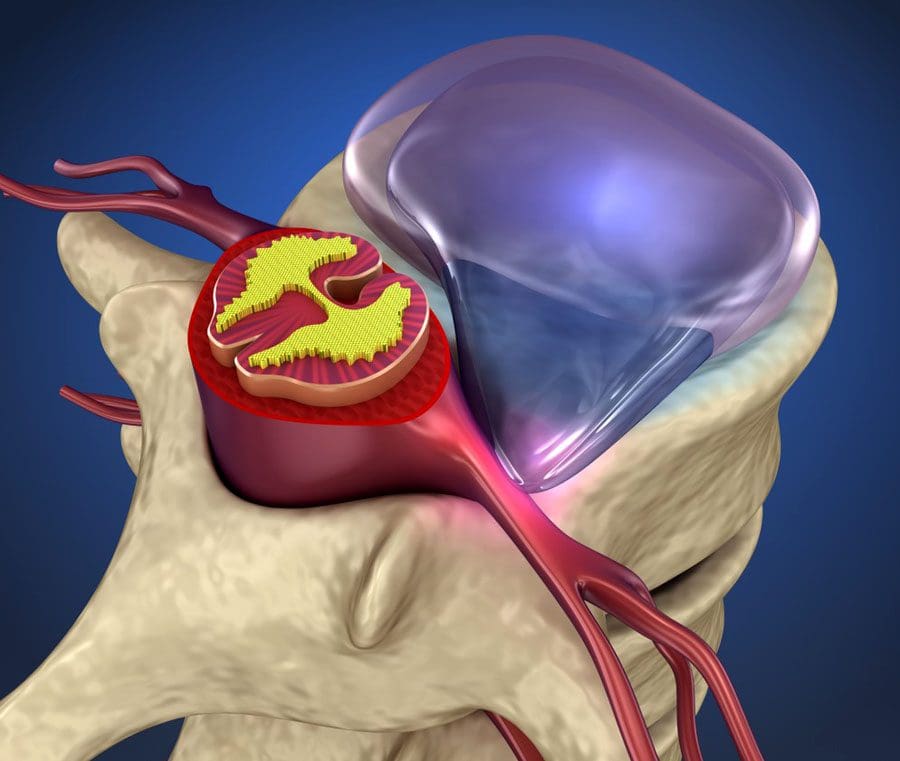
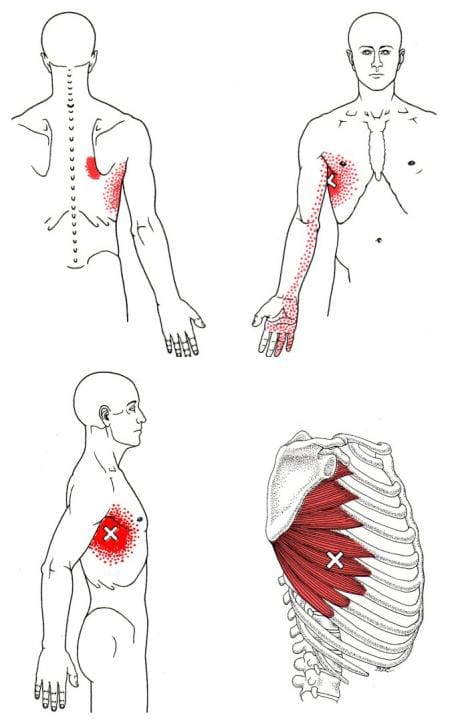
The book “Myofascial Pain and Dysfunction,” by Dr. Janet Travell, M.D., mentioned that abdominal symptoms are common and can cause diagnostic confusion for many people. Since the abdominal muscles can provide stability to the body’s trunk when a person overuses the abdominal muscles through various activities like quick and violent twisting of the mid-section, lifting heavy objects with the core instead of the legs, overdoing exercise regimes, or having a persistent cough, these various activities could potentially lead to the development of trigger points in the abdominal muscles causing pain in the abdomen and causing referred pain to the lower back. Studies reveal that trigger points along the abdominal muscles are developed through aggravating factors like prolonged sitting or standing can cause the abdominal muscles to become extremely tender and hyperirritable along the taut muscle bands. When trigger points affect the abdominal muscles, they can produce referred abdominal pain and visceral disorders (somato-visceral effects) that work closely together to mimic visceral diseases. This pertains to many individuals thinking something is wrong in their gut system, but their abdominal muscles are causing issues in their bodies.
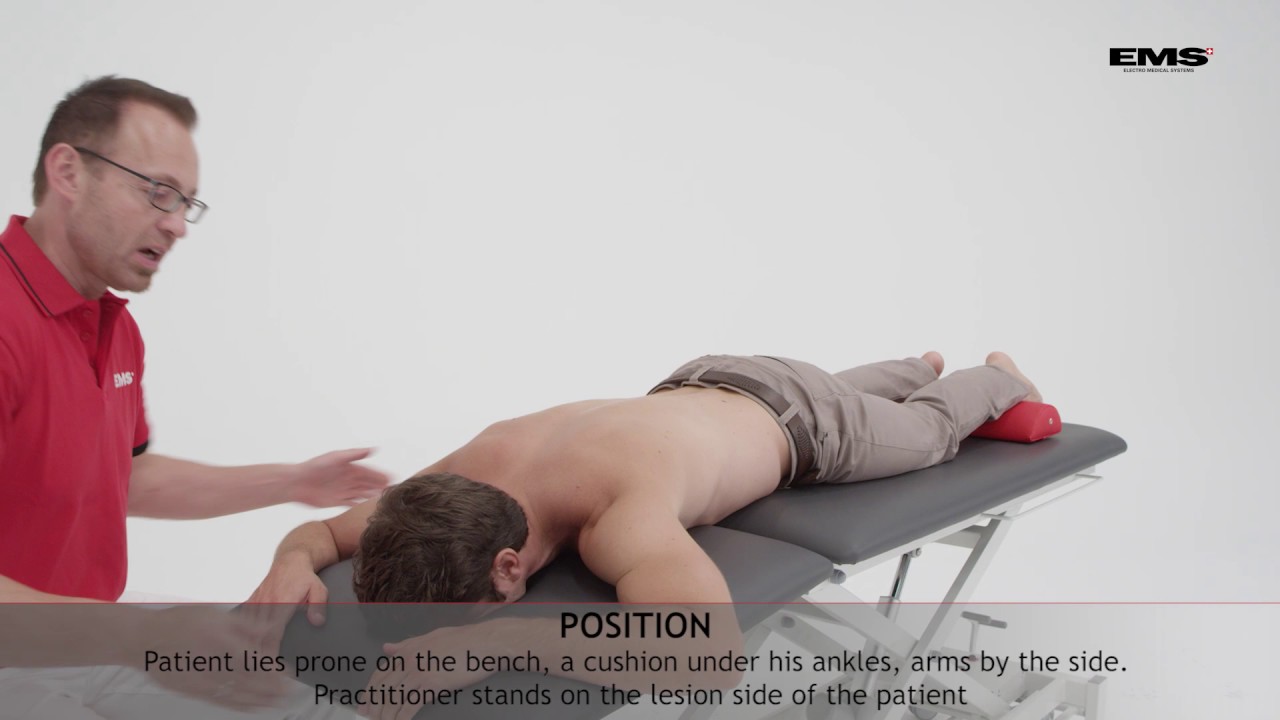
Releasing Trigger Points In The Abdominal Muscles-Video

Have you been experiencing abdominal issues around your torso? Does it hurt when you laugh, cough, or sneeze? Do you feel muscle stiffness or tenderness along your abdominals? If you have been dealing with these symptoms throughout your life, you could be experiencing abdominal pain associated with trigger points in your torso. Abdominal pain is common for many individuals and can vary from gut issues or muscle issues that various factors can cause in the torso. Abdominal issues can even cause confusion to doctors when they are diagnosing the issues that are affecting their patients. When various actions cause pain to the abdominals, it can develop referred pain associated with trigger points. Trigger points develop when the muscle has been overused, creating tiny nodules in the taut band. Trigger points can be tricky to pinpoint but are treatable. The video above shows where the trigger points are located in the abdominal muscles and how to release them from the affected abdominal muscles to provide relief and reduce the mimic effects of visceral-somatic pain.
Managing Trigger Points Associated With Abdominal Pain Through Various Treatments

When abdominal pain affects the muscles, the symptoms can develop trigger points. When this happens, it can lead to confusion and often misdiagnosed. All is not lost; there are ways to manage trigger points associated with abdominal pain through various treatments. Studies reveal that various therapies like dry needling combined with palpations can reduce trigger points from causing more referred pain issues in the abdomen. Other ways to prevent trigger points from developing in the future are through exercises that can help strengthen the abdominal muscles. Exercises like abdominal breathing, pelvic tilts, sit-ups, and even laughter can help strengthen weak abdominal muscles and positively affect the body.
Conclusion
The torso has various muscles, known as abdominal muscles, that help protect the vital organs in the gut system, help stabilize the spinal column, and maintain good posture for many individuals. Various factors affecting the abdominal muscles can lead to a confusing diagnosis, as it could be an internal or external issue. When the abdominal muscles are affected by being overused through various activities, it can develop into trigger points in the muscles, causing visceral referred pain to the torso and cause muscle weakness. Luckily multiple treatments can help reduce the effects of trigger points associated with abdominal pain and can help strengthen the core of the body. This allows the individual to feel better and consider what not to do to their abdominals.
References
Balyan, Rohit, et al. “Abdominal Wall Myofascial Pain: Still an Unrecognized Clinical Entity.” The Korean Journal of Pain, The Korean Pain Society, Oct. 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5665744/.
Rajkannan, Pandurangan, and Rajagopalan Vijayaraghavan. “Dry Needling in Chronic Abdominal Wall Pain of Uncertain Origin.” Journal of Bodywork and Movement Therapies, U.S. National Library of Medicine, Jan. 2019, https://pubmed.ncbi.nlm.nih.gov/30691770/.
Seeras, Kevin, et al. “Anatomy, Abdomen and Pelvis, Anterolateral Abdominal Wall.” In: StatPearls [Internet]. Treasure Island (FL), StatPearls Publishing, 25 July 2022, https://www.ncbi.nlm.nih.gov/books/NBK525975/.
Tesh, K M, et al. “The Abdominal Muscles and Vertebral Stability.” Spine, U.S. National Library of Medicine, June 1987, https://pubmed.ncbi.nlm.nih.gov/2957802/.
Travell, J. G., et al. Myofascial Pain and Dysfunction: The Trigger Point Manual: Vol. 1:Upper Half of Body. Williams & Wilkins, 1999.

















 Neuropathy Therapeutic Massage
Neuropathy Therapeutic Massage