Maintaining a healthy and well-balanced nutritional plan is recommended for overall health. When the body is nourished healthily, it will perform optimally. Stress is part of daily life, and certain foods can enhance the body’s ability to handle stress, help target physical and emotional states, and protect the brain. The Injury Medical Chiropractic and Functional Medicine Clinic Team can provide therapeutic massage to increase circulation, and relax the mind and body, adjustments to restore any misalignments, and nutritional support and health coaching for total wellness.
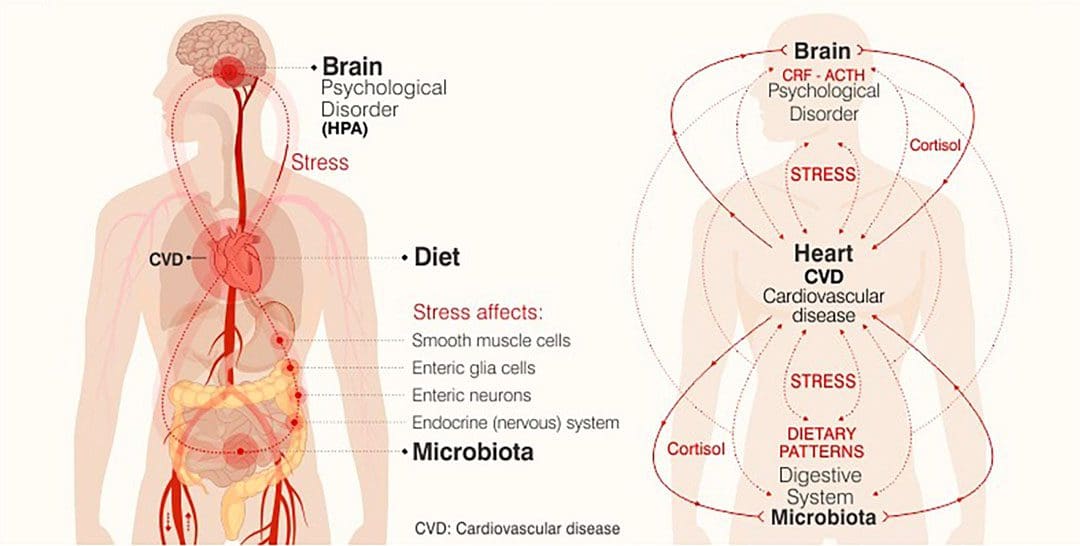
Table of Contents
Foods For Stress
Anxiety is a widespread condition affecting millions of individuals. Trying to lower stress levels includes self-care, sleep management, physical activity, and incorporating foods to reduce cortisol levels, the primary hormone responsible for stress.
Cortisol
Cortisol has a variety of functions that include:
- Manages how the body uses carbohydrates, fats, and proteins.
- Sleep cycle regulation.
- Blood pressure regulation.
- Increases blood sugar.
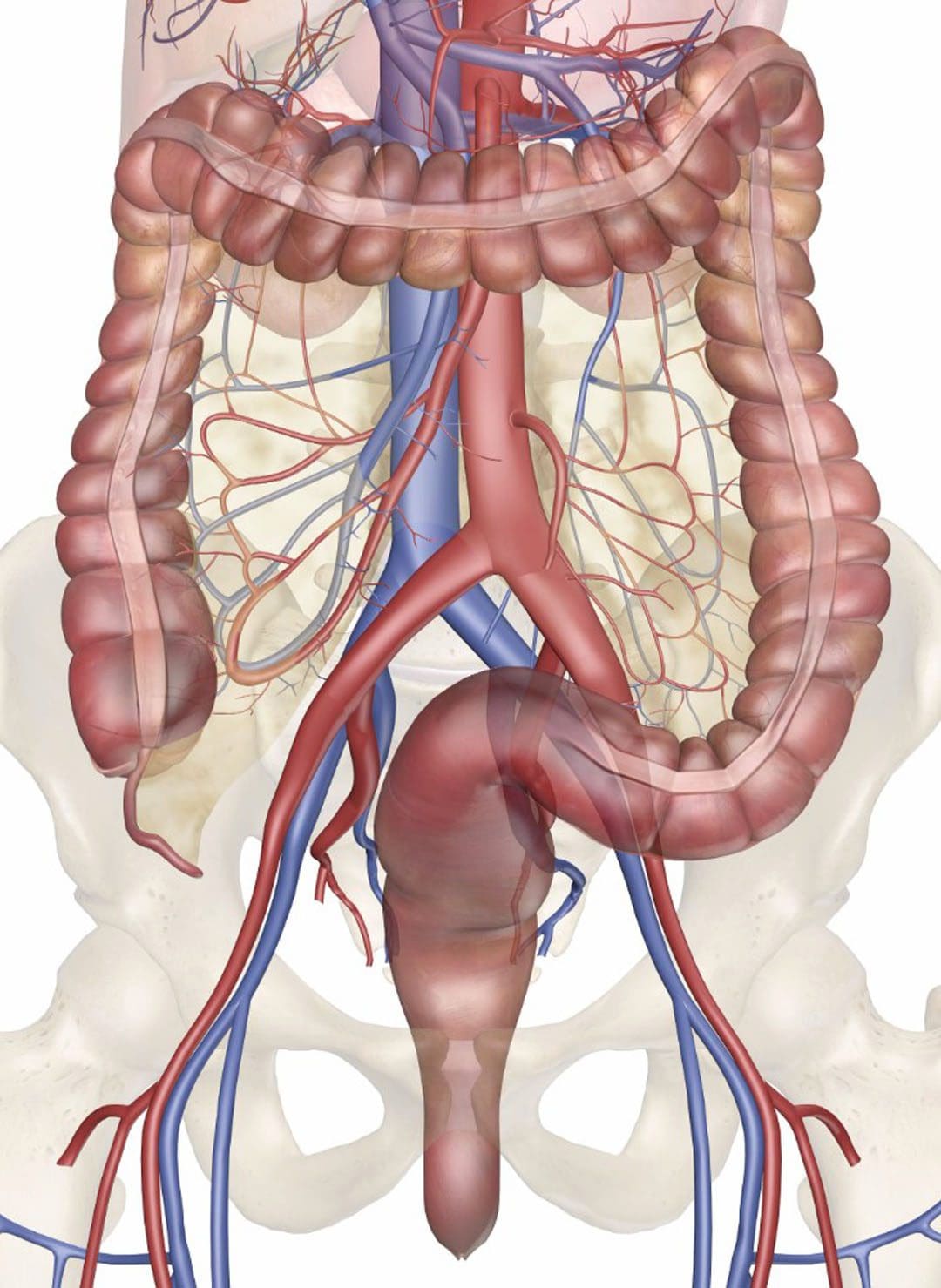
- Decreases inflammation.
Cortisol is sometimes known as the stress hormone because the adrenal gland releases it when experiencing stress or when the body is under physical stress/inflammation. It is the key to managing the fight-or-flight instinct and is healthy for a short period as a protective mechanism providing the energy needed to respond to short-term stress. However, the long-term release of cortisol generates tension in the body, leading to chronic inflammation and raised blood pressure. Learning how to manage stress is necessary for lowering cortisol levels.
Symptoms
Symptoms vary and are different for everybody.
Physical
- Exhaustion.
- Sleep problems.
- Headaches.
- Muscle tension.
- Jaw clenching.
- Aches and pains.
- Chronic illness from a weakened immune system.
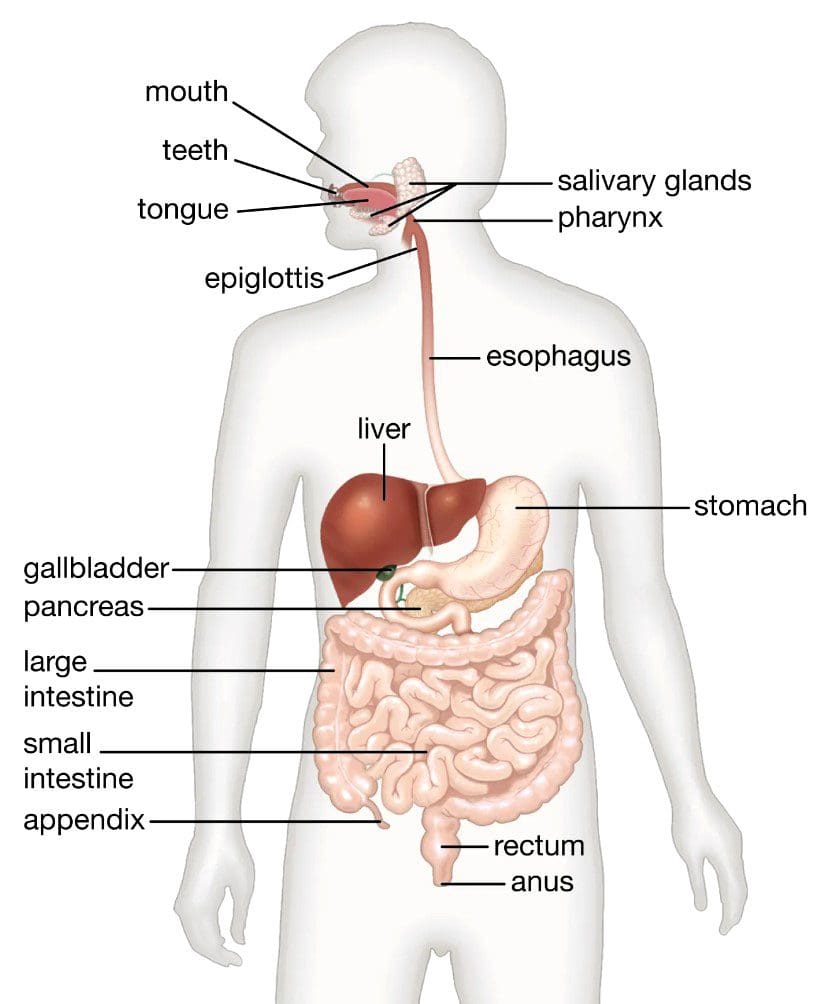
- Stomach or digestive problems.
- High blood pressure.
- Chest pain or a feeling like the heart is racing.
- Dizziness.
- Shaking.
Emotional and mental
- Irritability and or anxiousness.
- Sadness.
- Depression.
- Panic attacks.
Foods
The objective is to reduce inflammation, thus reducing cortisol levels. Recommended foods for stress include foods high in magnesium, vitamin B, Omega-3 fatty acids, protein, and foods that benefit the gut. Here are a few.
Magnesium
Magnesium is highly beneficial in reducing inflammation, metabolizing cortisol, and relaxing the mind and body.
- Dark chocolate.
- Bananas.
- Broccoli.
- Spinach.
- Avocados.
- Pumpkin seeds.
Vitamin B
Vitamin B12 can help with the metabolism of cortisol.
- Eggs.
- Fortified cereal.
- Chicken.
- Beef.
- Nutritional yeast.
- Organ meats.
Omega-3 Fatty Acid
These foods reduce inflammation.
- Olive oil.
- Avocados.
- Tuna.
- Sardines.
- Mackerel.
- Salmon
- Anchovies.
- Oysters.
- Walnuts.
- Chia seeds.
- Flax seeds.
Protein
These foods promote balanced blood sugar levels.
- Eggs.
- Peanuts.
- Almonds.
- Chicken breast.
- Turkey breast.
- Lean beef.
- Tuna.
- Shrimp.
- Salmon.
- Lentils.
- Quinoa.
Probiotic and Fermented
The immune system relies on the gut for immunity. Probiotics and fermented foods can help balance blood sugar and reduce cholesterol.
- Sauerkraut.
- Kombucha.
- Greek yogurt.
- Kefir.
- Kimchi.
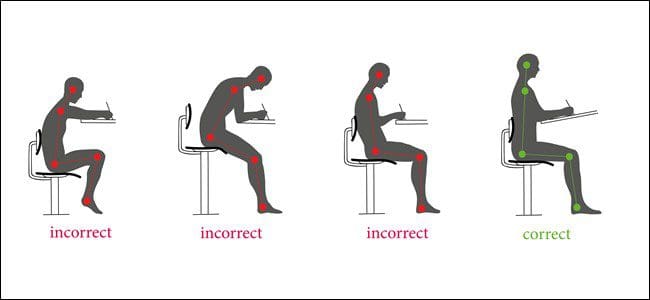
The key to lowering stress is a whole-body approach that includes exercise, proper sleep, and managing chronic diseases like diabetes, hypertension, and obesity, all of which can put the body in a prolonged state of inflammation. Incorporating these foods into a nutritional plan can help relieve stress naturally.
Impact of Stress
References
Aucoin, Monique, and Sukriti Bhardwaj. “Generalized Anxiety Disorder and Hypoglycemia Symptoms Improved with Diet Modification.” Case reports in psychiatry vol. 2016 (2016): 7165425. doi:10.1155/2016/7165425
Errisuriz, Vanessa L et al. “Perceived stress and dietary choices: The moderating role of stress management.” Eating behaviors vol. 22 (2016): 211-216. doi:10.1016/j.eatbeh.2016.06.008
Norwitz, Nicholas G, and Uma Naidoo. “Nutrition as Metabolic Treatment for Anxiety.” Frontiers in psychiatry vol. 12 598119. 12 Feb. 2021, doi:10.3389/fpsyt.2021.598119
Serafini, Mauro, and Ilaria Peluso. “Functional Foods for Health: The Interrelated Antioxidant and Anti-Inflammatory Role of Fruits, Vegetables, Herbs, Spices and Cocoa in Humans.” Current pharmaceutical design vol. 22,44 (2016): 6701-6715. doi:10.2174/1381612823666161123094235
Zellner, Debra A et al. “Food selection changes under stress.” Physiology & behavior vol. 87,4 (2006): 789-93. doi:10.1016/j.physbeh.2006.01.014