Can neurological physical therapy help individuals diagnosed with a recently acquired or chronic neurological condition gain strength and functioning?

Table of Contents
Neurological Physical Therapy
Neurological physical therapy can be extremely beneficial. It aims to restore functional mobility, strength, balance, and coordination in those with neurological conditions that affect their quality of life and ability to move around. It also helps recover from neurological injuries or prevent the progression and worsening of chronic neurological conditions. Depending on the severity of the condition, individuals may receive this therapy as an inpatient or outpatient. Exercise can help improve mobility, increase independence, and decrease the need for assistance, all of which can improve one’s quality of life.
Process
Neurological physical therapy is geared toward treating individuals with conditions affecting the brain and spinal cord, such as stroke, spinal cord injury, and Parkinson’s disease, to help restore mobility and function. The therapy is performed in hospitals, private practice physical therapy clinics, doctors’ offices, rehabilitation facilities, or at a patient’s home. Whether an individual needs inpatient or outpatient physical therapy will depend on the severity of the neurological condition.
- Newly acquired neurological conditions such as strokes or traumas like spinal cord injuries and traumatic brain injuries or TBIs often require inpatient rehabilitation.
- Once the patient gains enough strength, coordination, and independence with movements like standing and walking, they can progress to outpatient physical therapy.
- The patient will undergo a physical exam after a physical therapist has gathered enough information about medical history during the initial evaluation.
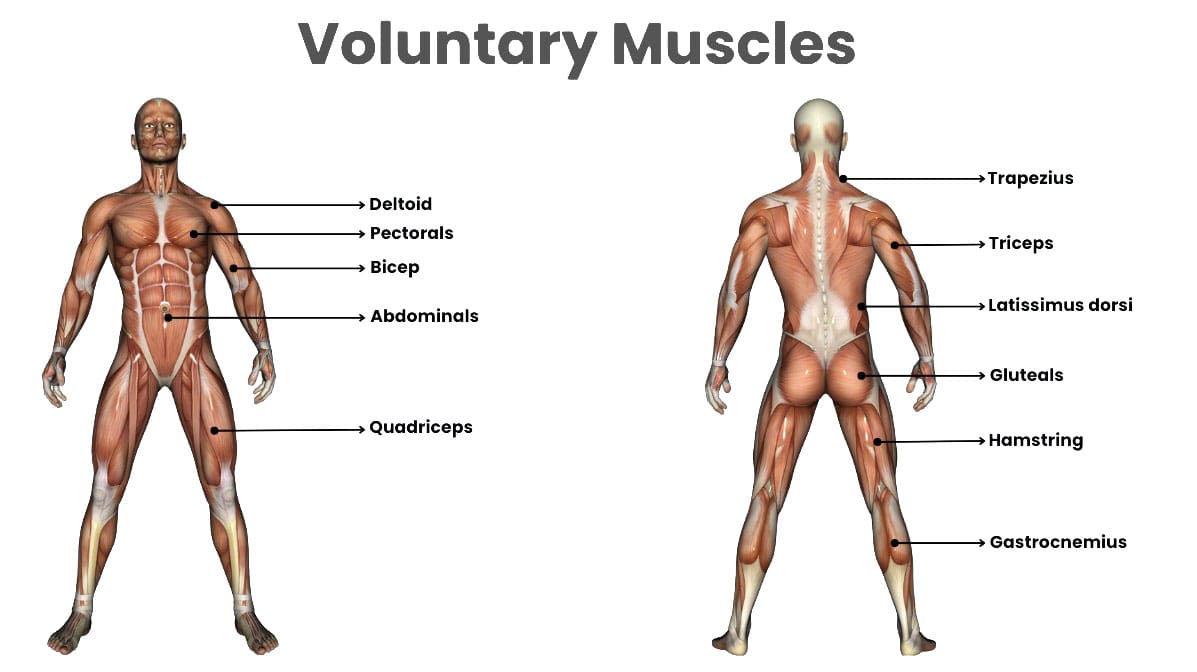
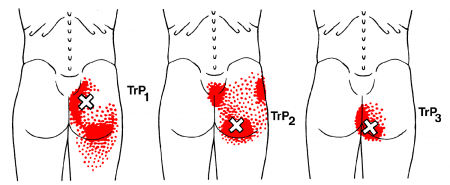
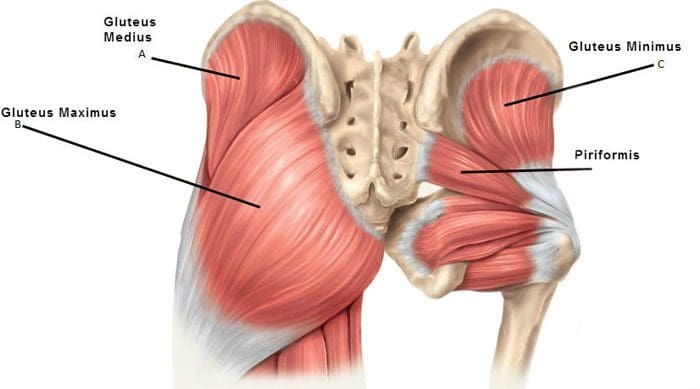
- The therapist will check muscle strength, coordination, range of motion, reflexes, and the muscle tone of the arms and legs. They may also perform neurological tests to examine coordination, such as following moving objects with the eyes, touching the finger to the nose, and rapidly alternating movements.
- The individual general level of attention, cognition, and sensation will also be assessed to determine if these areas have been affected by the neurological condition. (Cleveland Clinic, 2022)
- The therapist will then assess the patient’s ability to perform movements called transfers, which are transitions to and from positions such as lying down to sitting up or standing up to sitting.
- They will note if the patient can perform these movements independently or if they need assistance.
- The initial evaluation will also include an assessment of balance, quality of gait, and whether the therapist needs to assist.
- Depending on the severity of the neurological condition, the therapist may provide the patient with or recommend purchasing an assistive device to help walk.
Treatment Sessions
During therapy sessions, patients may receive the following interventions:
Gait Training
- To improve walking ability, proper instruction on using assistive devices such as canes, walkers, and crutches.
Balance Training
- To improve static/stationary and dynamic/while moving balance, both sitting unsupported to improve core control and standing upright with or without handheld support.
Therapeutic Activities
- To improve independence with bed mobility skills like rolling and sitting up from lying down and transfers on and off beds, chairs, and toilets.
- Therapeutic exercises for stretching and strengthening muscles and improving coordination and motor control.
Endurance Training
- This can be done with cardiovascular equipment like treadmills, stationary bicycles, and ellipticals.
Vestibular Therapy Interventions
- Balance exercises with head movements and exercises to treat a common cause of dizziness are used to improve eye movement control.
- Examples are the Dix-Hallpike and Epley maneuvers.
Conditions
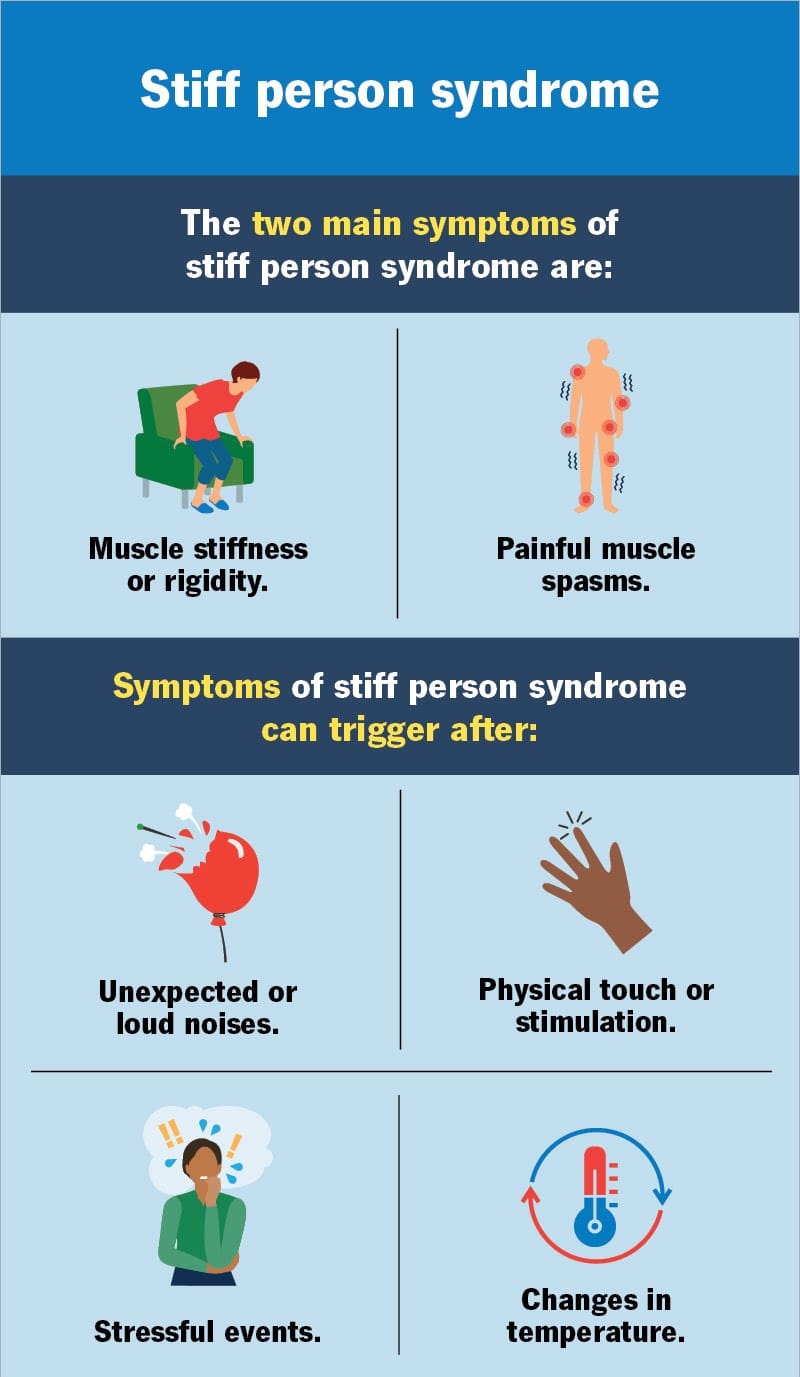
Neurological physical therapy can treat various conditions. Some neurological conditions are progressive, worsening over time, and require regular physical therapy and at-home exercises to maintain optimal health and wellness. Neurological conditions that can be treated with physical therapy include: (Cleveland Clinic, 2022)
- Strokes – loss of blood supply to the brain.
- Spinal cord injuries – damage to part of the central nervous system resulting in loss of movement and control.
- Polyneuropathies – damage to the peripheral nerves.
- Traumatic brain injuries – for example, concussions.
- Cerebral palsy – a group of disorders affecting movement, balance, and posture.
- Multiple sclerosis – a disabling disease of the brain and spinal cord.
- Parkinson’s disease – a progressive nervous system disorder.
- Guillain-Barre syndrome – an autoimmune disease attacking the nerves.
- Amyotrophic lateral sclerosis/ALS, also known as Lou Gehrig’s disease.
- Vertigo, including benign paroxysmal positional vertigo or BPPV.
Neurological conditions, like an automobile collision, can occur suddenly or be progressive, such as Parkinson’s. Physical therapy helps those individuals by increasing their use of weakened muscles, improving their motor control, coordination, and balance, and facilitating their independence with daily tasks and movements. Always seek immediate medical attention for any sudden, unexplained muscle weakness. Individuals who experience skeletal muscle weakness should discuss the type and duration of symptoms with their doctor, specialist, physical therapist, or chiropractor, as this might be a sign of a medical condition such as a neuromuscular disorder. Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to develop a personalized treatment program through an integrated approach to treat injuries and chronic pain syndromes, improving flexibility, mobility, and agility, relieving pain, and helping individuals return to normal activities. If other treatments are needed, Dr. Jimenez has teamed up with top surgeons, clinical specialists, medical researchers, and rehabilitation providers to provide the most effective treatments.
Personal Injury Rehabilitation
References
Cleveland Clinic. (2022). Neurological Exam. https://my.clevelandclinic.org/health/diagnostics/22664-neurological-exam