Can individuals dealing with scoliosis incorporate various exercises and stretches to improve their posture and reduce pain?
Table of Contents
What Is Scoliosis?
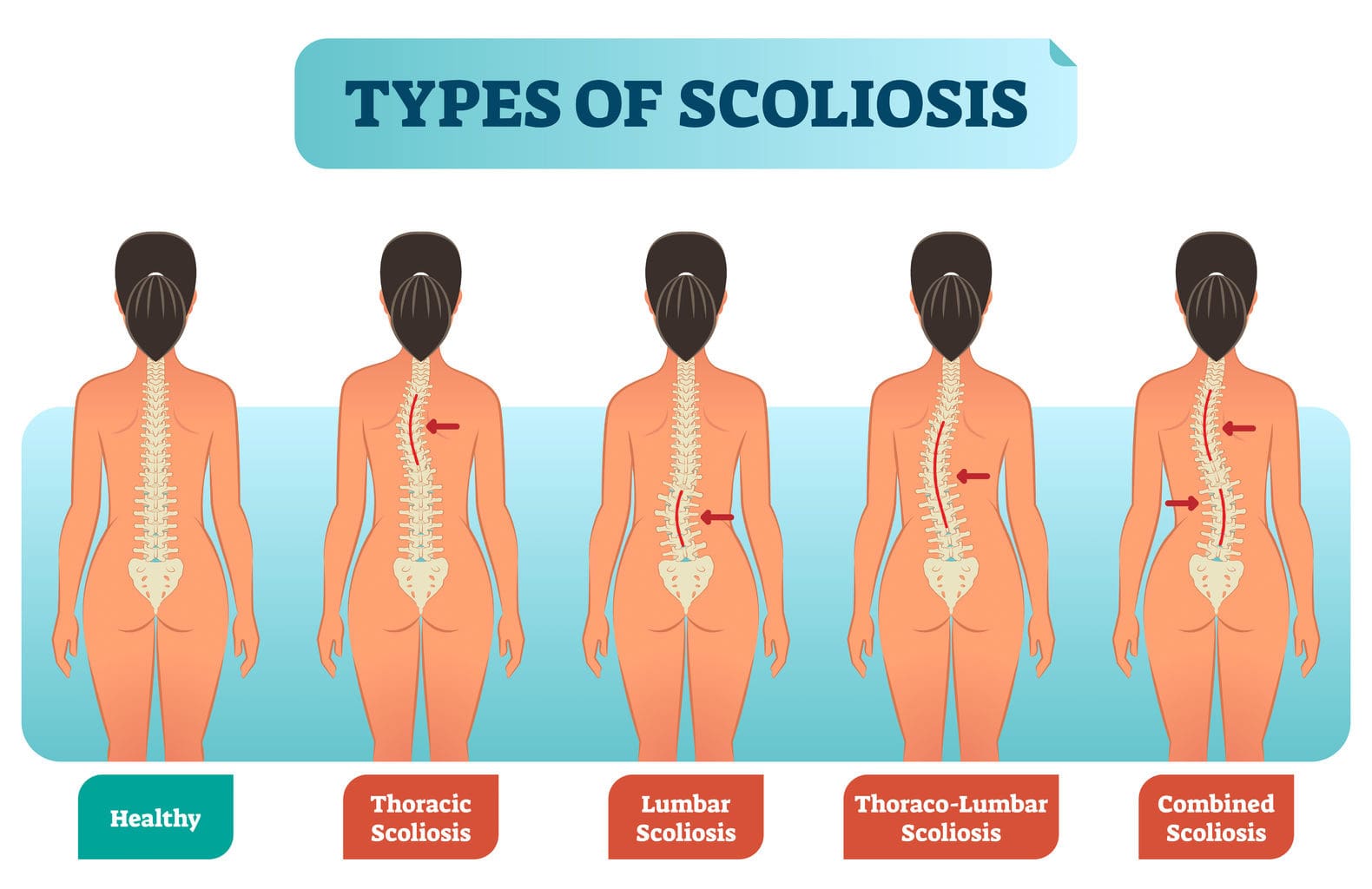
More often than anything, many people have tried to maintain proper posture to prevent musculoskeletal and spinal conditions from forming. However, it can be difficult to maintain an appropriate posture when strenuous environmental factors come into play. This can range from being in a hunched position to developing spinal conditions that can affect the curvature of the spine. One of the most well-known spinal conditions many people can develop through numerous risk factors is spinal scoliosis. Spinal scoliosis is often defined as a curvature deviation in the normal vertical spinal line. (Janicki & Alman, 2007) This causes the spine to develop an S or C curve in the thoracic or lumbar portion of the spine, leading to overlapping risk profiles in the body and causing pain-like symptoms that can make a person feel miserable. Today’s article looks at scoliosis, how it affects the body, and how various exercises can help manage scoliosis. We discuss with certified medical providers who inform our patients how non-surgical treatments, like various exercises, help manage symptoms associated with scoliosis. While asking informed questions to our associated medical providers, we advise patients to include various exercises and pain management techniques to reduce pain-like symptoms correlating with scoliosis. Dr. Alex Jimenez, D.C., encompasses this information as an academic service. Disclaimer.
How Does It Affect The Body?
Since scoliosis is a spinal deformity condition that affects the spine, it can happen at any age and is categorized into four group forms:
- Congenital (Presented by birth)
- Neuromuscular (Resulted from cerebral palsy or muscular dystrophy)
- Idiopathic (The common spinal condition)
- Degenerative (Adult-onset scoliosis)
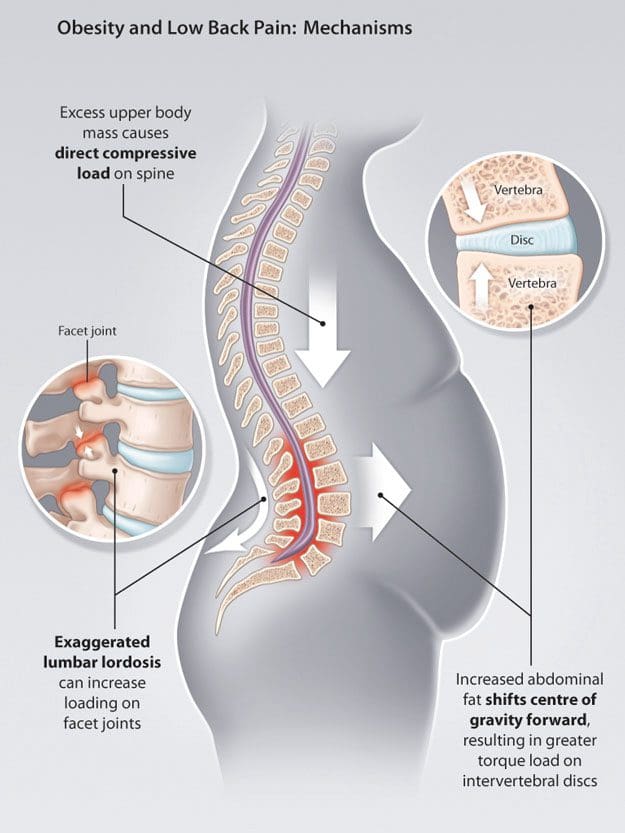
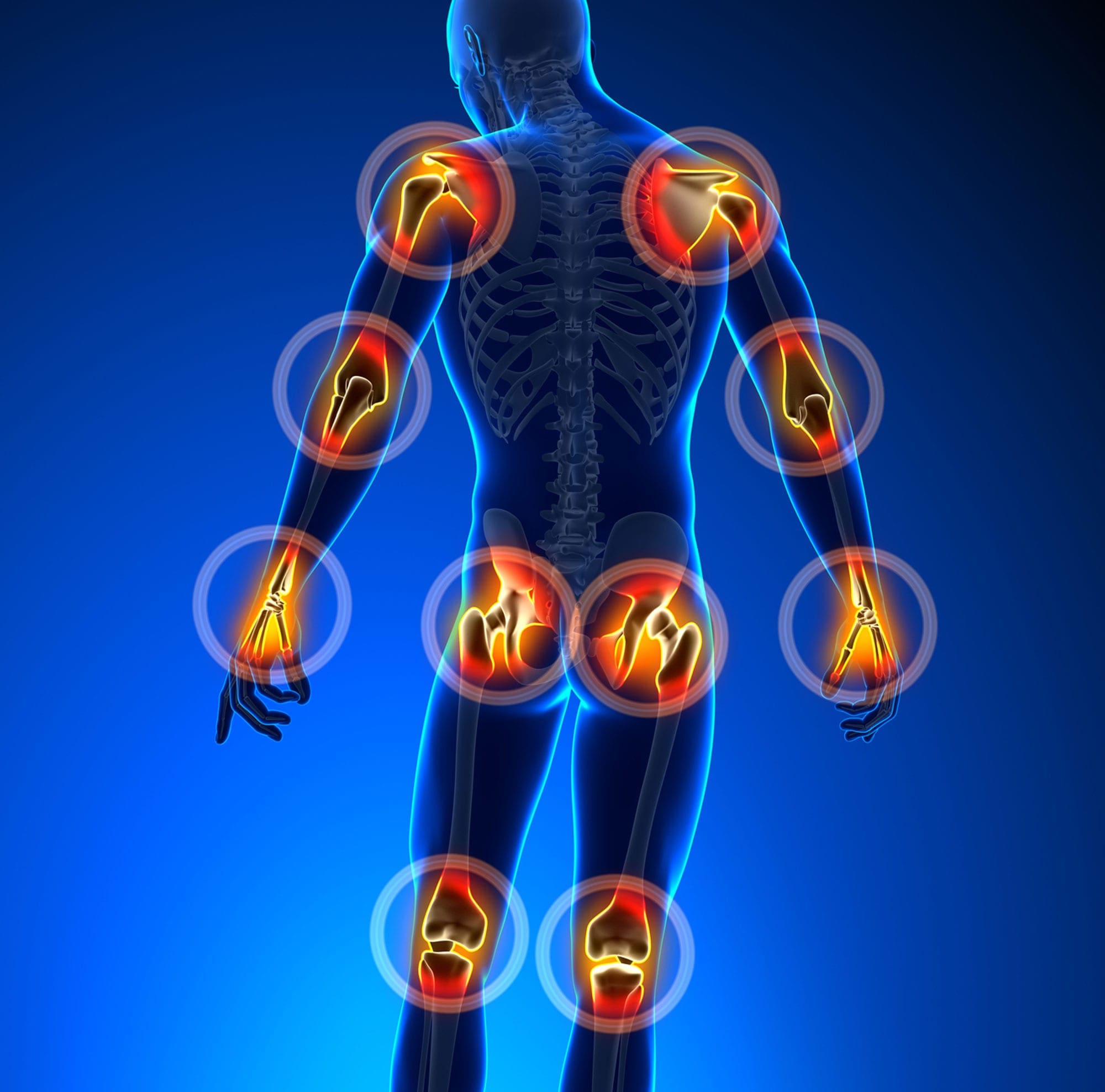
Within these four groups of scoliosis, some of the pain-like symptoms can vary depending on the size of the curve and how far the progression leads to overlapping risk profiles in the thoracic and lumbar spine portions. (Aebi, 2005) Some of the symptoms that are associated with scoliosis are back pain. Many individuals with scoliosis, especially adolescent individuals, have back pain associated with adolescent idiopathic scoliosis due to increasing age, injuries, and how severe the spine is curved. (Achar & Yamanaka, 2020) Additional symptoms that many individuals experience with scoliosis that can affect their bodies have specific features that cause pain. Individuals with scoliosis often have increasing asymmetrical pain when standing for prolonged periods and residing at rest, thus mimicking sciatica pain. (Zaina et al., 2023) This is because pain is one of the biomarkers for scoliosis. When pain starts to affect the body, issues like muscle dysfunction, concave disc pressure, asymmetrical facet joint strains, and a high BMI (body mass index) become the main mechanical parameters in the body. They are assessed by doctors when being examined. (Ilharreborde et al., 2023) When individuals are being assessed by their doctors to manage scoliosis, non-surgical treatments can help manage the pain-like symptoms and restore joint stability and mobility to the body.
Movement Medicine: Chiropractic Care- Video

Various Exercises For Managing Scoliosis
When many individuals dealing with scoliosis go in for non-surgical treatments, they will be assessed and evaluated by pain specialists to determine what the next steps for treatment can be provided for them. For scoliosis, non-surgical treatments like chiropractic care can be provided to reduce the musculoskeletal conditions associated with scoliosis. Chiropractors utilize mechanical and manual spinal manipulation of the spine. They can set the vertebra back in place while restoring the spinal joint with optimal motion, improving the range of motion, and allowing the body to function properly. (Milne et al., 2022) At the same time, chiropractors can recommend various exercises and stretches to help manage symptoms associated with scoliosis as part of their treatment plan. Incorporating various exercises can help rectify spinal deformity, help the different muscle groups become stronger, and allow the individual to work a bit on managing scoliosis symptoms. Below are some of the various exercises and stretches to manage scoliosis.
Practicing Good Posture
Practicing good posture can benefit many individuals with scoliosis, especially young ones. Many people realize that maintaining good posture can help reduce muscle pain and tension in the back. It allows many people to realign their bodies and retrain them to stand with good posture naturally. Maintaining good posture, whether standing or seated, can allow doctors to scan the body for any tension signs. For those with scoliosis, it can gradually strengthen the weak core muscles in their bodies.
Abdominal Presses
Abdominal presses allow the individual to maintain neutral spinal alignment while strengthening the abdominal core muscles. To do this:
- Individuals must lie on their backs on a yoga mat, keeping their backs in a neutral, tension-free position with bent knees.
- They raise both feet and thighs off the mat to form a 90-degree angle with their knees above the hips. *They can support themselves with a chair or wall.
- Next, individuals can use their hands to push and pull the knees with their abdominal muscles.
- When doing this static exercise, make sure that they hold for three full breaths in two sets of ten and relax in between.
Bird-Dog
Bird-dog is a yoga move that can help stretch tight and weak muscles in the back and allow the body to balance itself. To do this:
- Individuals can be on their hands and knees with a neutral spine position on a yoga mat, ensuring their hands are under their shoulders and their knees are under their hips.
- With controlled breathing, extend one arm straight out while extending the opposite leg back.
- Maintain the position for five to thirty seconds, and slowly return to the neutral spine.
- Repeat the motion with the opposite for 10 to 15 reps.
Incorporating these exercises can help manage pain-like symptoms associated with scoliosis, help many individuals strengthen their weak muscles, and help improve their posture on their health and wellness journey.
References
Achar, S., & Yamanaka, J. (2020). Back Pain in Children and Adolescents. American Family Physician, 102(1), 19-28. https://www.ncbi.nlm.nih.gov/pubmed/32603067
https://www.aafp.org/pubs/afp/issues/2020/0701/p19.pdf
Aebi, M. (2005). The adult scoliosis. Eur Spine J, 14(10), 925-948. https://doi.org/10.1007/s00586-005-1053-9
Ilharreborde, B., Simon, A. L., Shadi, M., & Kotwicki, T. (2023). Is scoliosis a source of pain? J Child Orthop, 17(6), 527-534. https://doi.org/10.1177/18632521231215861
Janicki, J. A., & Alman, B. (2007). Scoliosis: Review of diagnosis and treatment. Paediatr Child Health, 12(9), 771-776. https://doi.org/10.1093/pch/12.9.771
Milne, N., Longeri, L., Patel, A., Pool, J., Olson, K., Basson, A., & Gross, A. R. (2022). Spinal manipulation and mobilisation in the treatment of infants, children, and adolescents: a systematic scoping review. BMC Pediatr, 22(1), 721. https://doi.org/10.1186/s12887-022-03781-6
Zaina, F., Marchese, R., Donzelli, S., Cordani, C., Pulici, C., McAviney, J., & Negrini, S. (2023). Current Knowledge on the Different Characteristics of Back Pain in Adults with and without Scoliosis: A Systematic Review. J Clin Med, 12(16). https://doi.org/10.3390/jcm12165182