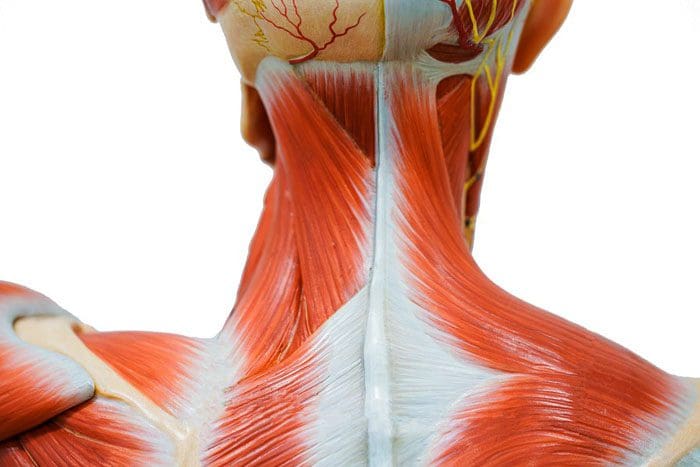
Relaxing the low back muscles. The low back supports the weight of the upper body and provides mobility. The lumbar spine/low back is a complex structure of interconnecting:
- Bones
- Joints
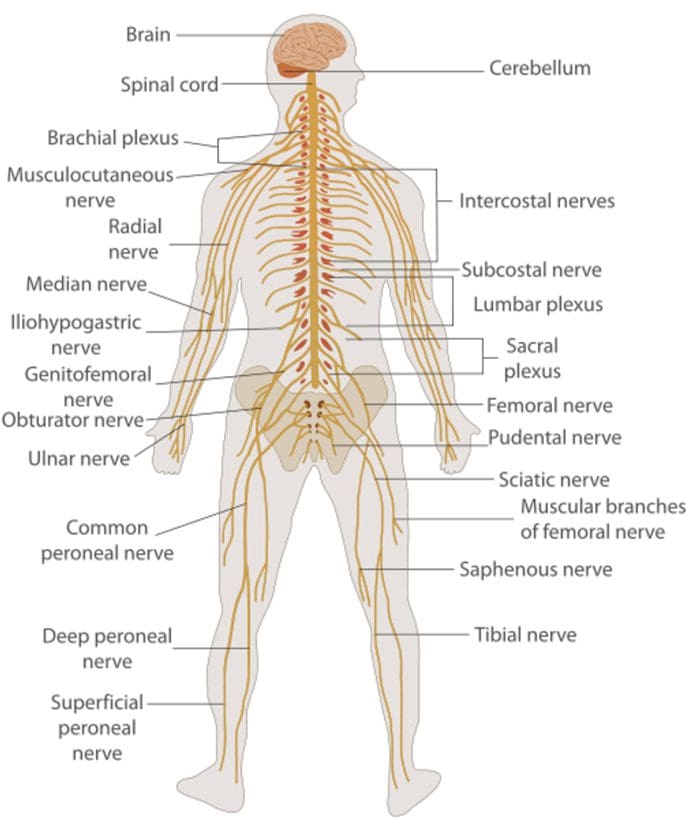
- Nerves
- Ligaments
- Muscles
- All work together to provide support, strength, and flexibility.
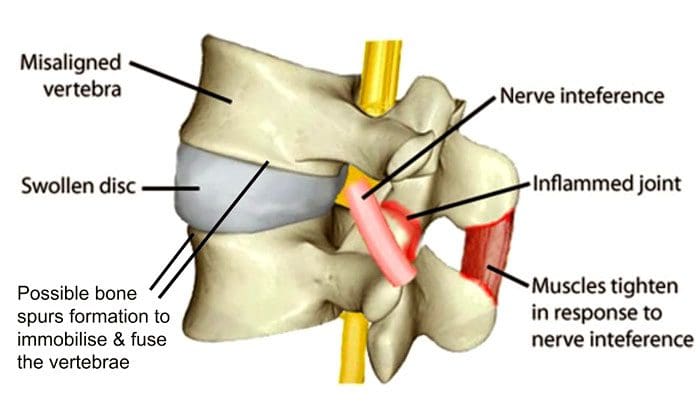
However, this complex structure is highly susceptible to injury and pain. The muscles in the low back support the spinal column and are responsible for flexing, rotating the hips when walking. The nerves in the low back supply sensation and power the muscles in the pelvis, legs, and feet. The most common acute low back pain cases are brought on from injury to the:
- Muscles
- Ligaments
- Joints
- Discs
The body also reacts to injury by triggering an inflammatory response. Inflammation can cause severe pain. The key is relaxing the muscles and keeping them loose.

Table of Contents
Lower back pain causes
The most common cause is muscle spasms, which can be triggered by:
- Constant improper posture
- Repetitive and overuse motions
- Chronic inflammation brought on by underlying condition/s
- Quick awkward movements like twisting, reaching, and/or bending at the wrong angle can set off pain symptoms.
- If the same back muscles are getting strained and/or pulled continuously, this could indicate an underlying problem with a misaligned vertebra.
Correct improper postures
Improper posture and body positioning eventually present with discomfort and pain. Individuals are constantly hunched over and slumped in front of computers and devices, along with sitting with crossed legs, sleeping on a non-supportive mattress, and there is a perfect recipe for low back pain. Adjusting sitting, desk, and computer ergonomics and using smart devices with posture awareness will go a long way to correct improper posture.
Stretch and loosen tight muscles
Stretch out throughout the day and before going to bed. Sitting all day at work, then going home and sitting all evening is not healthy for the body’s muscles. The muscles shorten, as do the ligaments and tendons. Stretching keeps the body loose and limber. Try out different forms of stretching, as well as foam rolling for the back.
Get the body moving
Cramped or pulled muscles need time to recover. Too much rest or being completely inactive makes sense but is not recommended. Light movement keeps the blood flowing, especially in and around the injured/sore area. This increases healing and shortens recovery time. Just some light walking is recommended. Getting up and moving while relaxing around the house will get the muscles back in shape.
Body Composition
Benefits of collagen
Gastrointestinal Health
Collagen generates a protective barrier effect on the intestinal mucosa that lines the digestive tract. One study found that collagen supplementation protects against the breakdown of the intestinal wall after a burn injury. A lack of collagen from aging or other factors could impair the structure of the intestinal mucosa. This could lead to digestive problems like leaky gut syndrome and irritable bowel syndrome.
Joint Health and Mobility
Collagen provides structure and cushion in the joints. As the body ages, the cushion wears down, and joint mobility decreases. This increases the risk of injury. Taking collagen supplements can help improve symptoms of osteoarthritis, rheumatoid arthritis, and other conditions.
References
Finta, Regina et al. “The effect of diaphragm training on lumbar stabilizer muscles: a new concept for improving segmental stability in the case of low back pain.” Journal of pain research vol. 11 3031-3045. 28 Nov. 2018, doi:10.2147/JPR.S181610
Lugo, James P et al. “Efficacy and tolerability of an undenatured type II collagen supplement in modulating knee osteoarthritis symptoms: a multicenter randomized, double-blind, placebo-controlled study.” Nutrition journal vol. 15 14. 29 Jan. 2016, doi:10.1186/s12937-016-0130-8
National Institute of Neurological Disorders and Stroke. Pain: Hope Through Research. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Hope-Through-Research/Pain-Hope-Through-Research. June 9, 2017.