Table of Contents
Motor Vehicle Accidents: Understanding Mobility and Flexibility Challenges
Motor vehicle accidents (MVAs) are a significant public health concern, causing millions of injuries annually across the United States. In 2023 alone, over 6 million crashes were reported nationwide, with 391,428 in Florida. (Catalyst Physical Therapy). These accidents often result in injuries that impair mobility and flexibility, affecting victims’ ability to perform daily tasks and maintain their quality of life. This comprehensive blog post examines how MVAs contribute to mobility and flexibility issues, the specific injuries associated with them, their impact on daily activities, and effective treatment strategies. We also examine the role of advanced diagnostics in treatment and legal documentation, particularly in personal injury cases, based on clinical insights from Dr. Alexander Jimenez, a chiropractor and nurse practitioner in El Paso.
How MVAs Cause Mobility and Flexibility Problems
Mobility refers to the ability to move freely, while flexibility is the range of motion available at a joint. Both are essential for everyday activities, such as walking, sitting, or lifting objects. MVAs disrupt these abilities through sudden, forceful impacts that strain or damage the musculoskeletal system, leading to pain, stiffness, and restricted movement.
Common Injuries from MVAs
MVAs can cause various injuries, each with unique effects on mobility and flexibility. Below is a detailed look at the most common types:
| Injury Type | Description | Impact on Mobility/Flexibility |
|---|---|---|
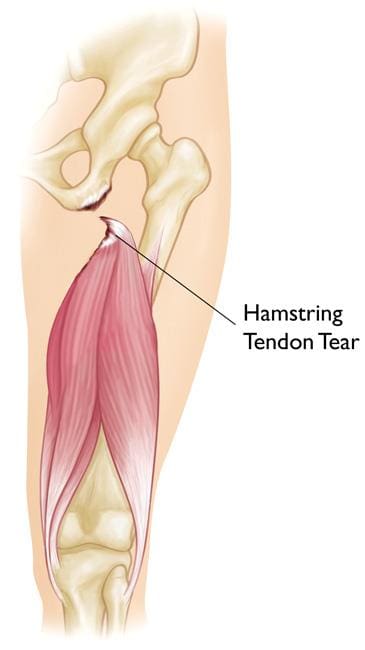
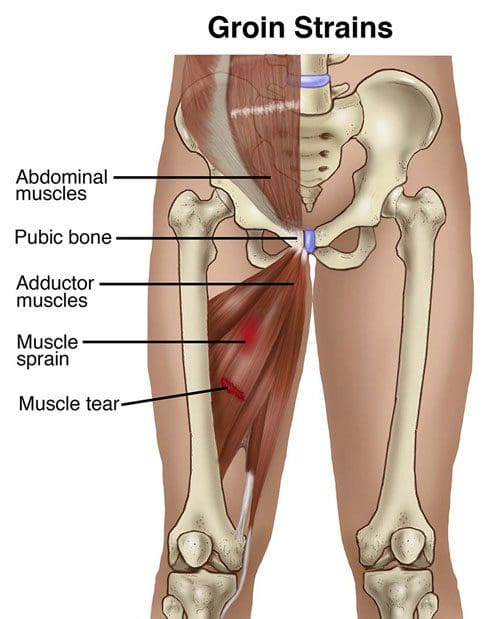
| Soft Tissue Injuries | Damage to muscles, ligaments, or tendons, often resulting from rapid movement, such as whiplash. | Causes pain, swelling, and stiffness, limiting movement. (Catalyst Physical Therapy). |
| Spine Injuries | These injuries can include herniated discs or damage to the spinal cord due to compression or impact. | Leads to chronic pain, numbness, or paralysis, restricting motion. (Cox Law Firm). |
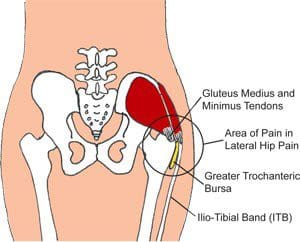
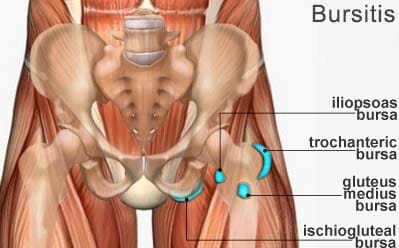
| Joint Injuries | Impact from the dashboard or seatbelt often results in damage to the knees, hips, or shoulders. | Results in swelling, pain, and reduced range of motion, potentially causing osteoarthritis. (Kitchellaw). |
| Nerve Damage | Damage to nerves frequently occurs as a result of spinal or soft tissue damage, such as sciatica. | It impairs movement control by causing tingling, weakness, or numbness. (Sciatica Clinic). |
-
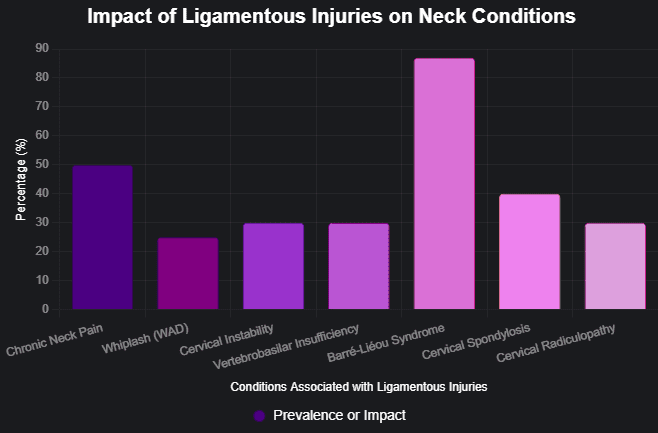
Soft Tissue Injuries
MVAs frequently cause soft tissue injuries, especially whiplash, a common occurrence in rear-end collisions where the head jerks forward and backward. The process strains neck muscles and ligaments, resulting in pain, stiffness, and a reduced range of motion. Other soft tissue injuries, such as muscle tears or ligament sprains in the back or shoulders, can similarly limit movement and cause discomfort (Sage Hill Physio). -
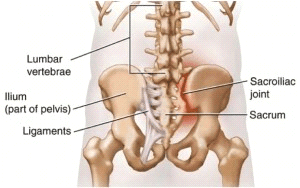
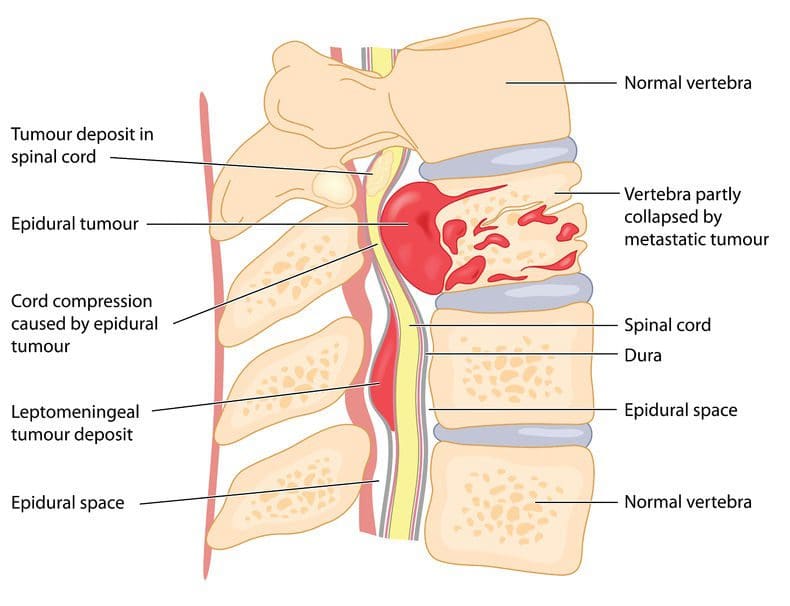
Spine Injuries
Spine injuries, such as herniated discs, are a serious consequence of MVAs. Damage to the cushioning between vertebrae can result in a herniated disc, which can potentially press on nerves and cause pain, numbness, or weakness. These injuries can limit a person’s ability to bend, twist, or stand for long periods. In severe cases, spinal cord injuries can lead to partial or complete paralysis, drastically reducing mobility (Cox Law Firm). -
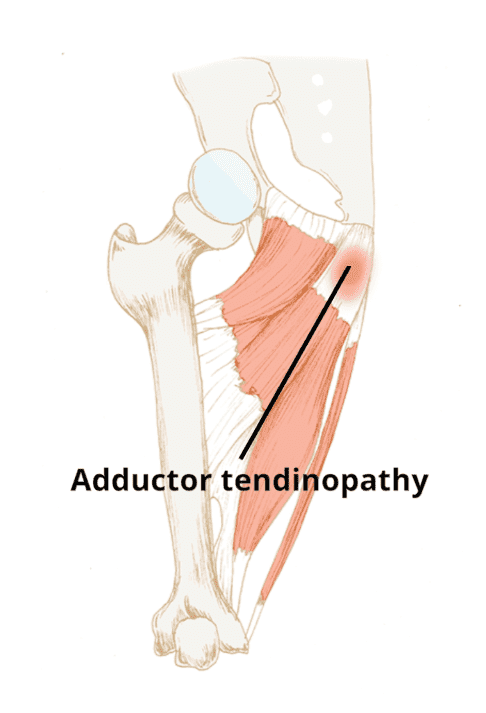
Joint Injuries
Joints, including those in the knees, hips, and shoulders, are vulnerable in MVAs. Impact from the dashboard or seatbelt can cause joint trauma, leading to pain, swelling, and reduced motion. Over time, these injuries may contribute to osteoarthritis, a degenerative condition that further impairs flexibility (Kitchellaw). -
Nerve Damage
Nerve damage can result from direct trauma or secondary injuries like herniated discs. MVAs often trigger or worsen conditions like sciatica, where pain radiates from the lower back down the leg. Nerve damage can cause tingling, burning, or numbness, making it difficult to move and resulting in discomfort. (Sciatica Clinic).
Mechanisms of Injury
The sudden forces in MVAs—such as rapid deceleration, twisting, or blunt impact—create various injury mechanisms:
- Whiplash: Rapid neck movement strains ligaments and muscles, causing nerve irritation.
- Blunt Force Trauma: Impact from steering wheels or airbags can fracture bones or damage joints.
- Compression Injuries: Sudden deceleration compresses the spine or joints, resulting in damage to the disc or cartilage.
- Indirect Trauma: Minor accidents can cause hidden injuries, like nerve compression, which may lead to chronic issues if untreated (SimplyPT).
Even low-speed collisions can cause significant damage, underscoring the importance of a medical evaluation after any motor vehicle accident (MVA).
References
- Catalyst Physical Therapy. (n.d.). Motor Vehicle Accident Injuries. Retrieved from https://catalystpt.org/pain-conditions/motor-vehicle-accident-injuries/
- Cox Law Firm. (n.d.). How to Adapt to Mobility Loss. Retrieved from https://www.coxcoxfilo.com/blog/how-to-adapt-to-mobility-loss/
- Kitchellaw. (n.d.). Long-term Effect of Car Accident Injuries. Retrieved from https://www.kitchellaw.com/blog/long-term-effect-car-accident-injuries.cfm
- Sage Hill Physio. (n.d.). Motor Vehicle Accident Recovery. Retrieved from https://www.sagehillphysio.com/blog/Motor-Vehicle-Accident-Recovery
- Sciatica Clinic. (n.d.). Automobile Collisions Resulting in Nerve Injury Explained. Retrieved from https://sciatica.clinic/automobile-collisions-resulting-in-nerve-injury-explained/
- SimplyPT. (n.d.). Hidden Injuries from Car Accidents. Retrieved from https://simplypt.com/hidden-injuries-from-car-accidents-why-you-shouldnt-skip-physical-therapy/
Impact on Daily Activities and Quality of Life
Mobility and flexibility problems from MVAs can profoundly affect daily life, turning routine tasks into significant challenges. These physical limitations often lead to emotional and financial consequences, further reducing quality of life.
Physical Limitations
- Difficulty with Basic Movements: Pain, stiffness, or weakness can make activities like getting out of bed, dressing, or climbing stairs laborious. For example, whiplash can restrict neck movement, making it difficult to turn the head (Catalyst Physical Therapy).
- Reduced Independence: Severe injuries may necessitate assistance with daily tasks, resulting in a dependency on family or caregivers. (Kitchellaw).
- Work and Financial Implications: Mobility issues can prevent individuals from working, resulting in lost income and financial stress. Vocational rehabilitation may be needed to adapt to new roles (LMLawNYC).
Emotional and Psychological Impact
- Frustration and Depression: The inability to perform normal activities can lead to feelings of helplessness and depression, particularly if recovery is slow (LMLawNYC).
- Anxiety: Fear of reinjury or pain can cause anxiety, especially when resuming activities like driving (Michigan Auto Law).
- Social Isolation: Physical limitations may prevent participation in social or community activities, leading to loneliness and isolation.
Long-term Complications
Untreated injuries can lead to chronic conditions, such as:
- Chronic Pain: Persistent pain from whiplash or herniated discs can become a lifelong issue (Kitchellaw).
- Osteoarthritis: Joint injuries may progress to degenerative conditions, further limiting mobility.
- Permanent Disability: Severe spinal cord injuries can result in permanent mobility loss, requiring lifelong care (Cox Law Firm).
Early medical intervention is crucial in preventing these outcomes and restoring function.
References
- Catalyst Physical Therapy. (n.d.). Motor Vehicle Accident Injuries. Retrieved from https://catalystpt.org/pain-conditions/motor-vehicle-accident-injuries/
- Cox Law Firm. (n.d.). How to Adapt to Mobility Loss. Retrieved from https://www.coxcoxfilo.com/blog/how-to-adapt-to-mobility-loss/
- Kitchellaw. (n.d.). Long-term Effect of Car Accident Injuries. Retrieved from https://www.kitchellaw.com/blog/long-term-effect-car-accident-injuries.cfm
- LMLawNYC. (2024, January 25). Immobility Caused by Car Accidents. Retrieved from https://www.lmlawnyc.com/blog/2024/01/immobility-caused-by-car-accidents/
- Michigan Auto Law. (n.d.). Trauma After Car Accident. Retrieved from https://www.michiganautolaw.com/blog/2025/03/31/trauma-after-car-accident/
Treatment and Rehabilitation
Effective treatment of MVA-related mobility and flexibility problems requires a multidisciplinary approach, combining chiropractic care, physical therapy, pain management, and, in severe cases, surgery. Early intervention is key to preventing chronic issues.
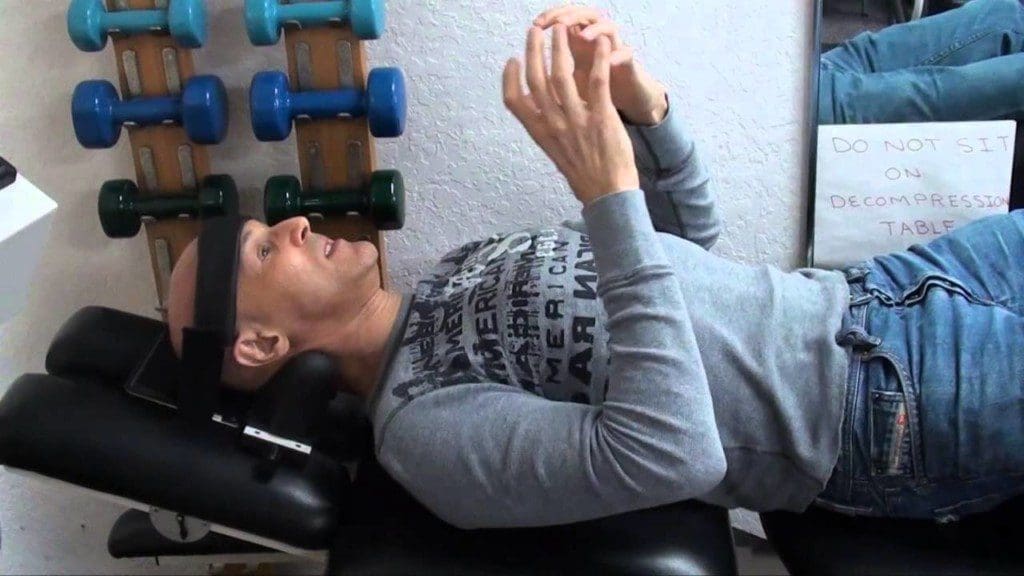
Chiropractic Care
Chiropractic care focuses on restoring spinal alignment and improving mobility through non-invasive techniques. Spinal adjustments, or manipulations, realign vertebrae, relieve nerve pressure, and enhance movement patterns (Wall Family Chiropractic). Dr. Alexander Jimenez, a chiropractor and nurse practitioner in El Paso, specializes in treating motor vehicle accident (MVA) injuries. His approach includes:
- Detailed Assessments: Evaluating injury mechanisms, biomechanics, and medical history.
- Advanced Imaging: Using X-rays and MRIs to diagnose conditions like whiplash or herniated discs.
- Personalized Treatment: Combining spinal manipulation, muscle therapy, and exercises to restore function (Dr. Alex Jimenez).
Dr. Jimenez’s clinical rationale for advanced imaging emphasizes the importance of accurate diagnosis. Hidden injuries, such as nerve compression, may not be evident without imaging, which guides tailored treatment plans and provides critical documentation for legal claims.
Physical Therapy
Physical therapy strengthens muscles, improves flexibility, and restores range of motion. Therapists use:
- Manual Therapy: Techniques like joint mobilization to reduce stiffness (Catalyst Physical Therapy).
- Exercises: Stretching and strength training to support joints and enhance resilience (Sage Hill Physio).
- Education: Teaching proper body mechanics to prevent further injury.
Early physical therapy can break the cycle of pain and disability, improving recovery outcomes (SimplyPT).
Pain Management
Pain management strategies include medications, injections, or alternative therapies like acupuncture. These approaches control pain while rehabilitation addresses underlying causes (Kitchellaw).
Surgery
When conservative treatments fail, we reserve surgery for severe cases like significant spinal cord damage or fractures. It aims to stabilize structures or repair tissues but carries risks and requires extensive recovery (Sage Hill Physio).
Role of Advanced Diagnostics
Advanced imaging (X-rays, MRIs, CT scans) and diagnostic assessments (EMG, nerve conduction studies) are crucial for:
- Accurate Diagnosis: Identifying hidden injuries like fractures or nerve damage (Catalyst Physical Therapy).
- Treatment Planning: Tailoring Interventions to Specific Injuries.
- Legal Documentation: Providing evidence for personal injury claims (Dr. Alex Jimenez).
References
- Catalyst Physical Therapy. (n.d.). Motor Vehicle Accident Injuries. Retrieved from https://catalystpt.org/pain-conditions/motor-vehicle-accident-injuries/
- Dr. Alex Jimenez. (n.d.). Personal Injury Doctor. Retrieved from https://dralexjimenez.com/personal-injury-doctor/
- Kitchellaw. (n.d.). Long-term Effect of Car Accident Injuries. Retrieved from https://www.kitchellaw.com/blog/long-term-effect-car-accident-injuries.cfm
- Sage Hill Physio. (n.d.). Motor Vehicle Accident Recovery. Retrieved from https://www.sagehillphysio.com/blog/Motor-Vehicle-Accident-Recovery
- SimplyPT. (n.d.). Hidden Injuries from Car Accidents. Retrieved from https://simplypt.com/hidden-injuries-from-car-accidents-why-you-shouldnt-skip-physical-therapy/
- Wall Family Chiropractic. (2024, October 30). Restoring Mobility and Range of Motion After a Car Crash. Retrieved from https://wallfamilychiropractic.com/2024/10/30/restoring-mobility-and-range-of-motion-after-a-car-crash/
Personal Injury Cases and Legal Aspects
MVAs often lead to personal injury cases, where victims seek compensation for medical expenses, lost wages, and pain and suffering. Accurate medical documentation is essential for these claims, and chiropractors play a critical role.
Dr. Jimenez’s practice in El Paso exemplifies this. His use of advanced diagnostics, such as X-rays and MRIs, ensures thorough documentation of injuries, supporting both treatment and legal proceedings. This documentation can demonstrate the extent of injuries, such as herniated discs or fractures, thereby strengthening compensation claims. (Dr. Alex Jimenez). Legal firms, such as Cox Law Firm, emphasize the importance of such records in securing fair settlements (Cox Law Firm).
References
- Cox Law Firm. (n.d.). How to Adapt to Mobility Loss. Retrieved from https://www.coxcoxfilo.com/blog/how-to-adapt-to-mobility-loss/
- Dr. Alex Jimenez. (n.d.). Personal Injury Doctor. Retrieved from https://dralexjimenez.com/personal-injury-doctor/
Case Studies and Clinical Observations
The sources do not provide specific case studies; however, clinical observations from chiropractic practices highlight effective treatment strategies. For example, patients with whiplash often experience significant improvements in neck mobility and pain reduction after spinal adjustments and targeted exercises (Wall Family Chiropractic).
Dr. Jimenez’s approach integrates chiropractic care with functional medicine, addressing both physical and emotional aspects of recovery. He notes that emotional trauma, such as anxiety or depression, can exacerbate mobility issues, necessitating holistic care. His use of advanced diagnostics ensures precise treatment, improving outcomes for MVA victims in El Paso (Dr. Alex Jimenez).
References
- Dr. Alex Jimenez. (n.d.). Personal Injury Doctor. Retrieved from https://dralexjimenez.com/personal-injury-doctor/
- Wall Family Chiropractic. (2024, October 30). Restoring Mobility and Range of Motion After a Car Crash. Retrieved from https://wallfamilychiropractic.com/2024/10/30/restoring-mobility-and-range-of-motion-after-a-car-crash/
Prevention and Long-term Management
Preventing motor vehicle accidents (MVAs) is the most effective way to avoid mobility and flexibility problems. Safe driving practices, such as wearing seatbelts, avoiding distractions, and obeying traffic laws, can reduce accident risks.
For those affected by MVAs, long-term management strategies include:
- Regular Exercise: Strengthening core muscles and improving flexibility through yoga or physical therapy (Sage Hill Physio).
- Proper Posture: Using ergonomic furniture to reduce spinal strain.
- Home Modifications: Installing ramps or grab bars to enhance accessibility (Kitchellaw).
- Ongoing Care: Regular chiropractic or physical therapy visits to monitor progress.
Home recovery tips, such as heat/ice therapy, gentle stretching, and proper nutrition, can also support healing (Wellness for Warriors).
References
- Kitchellaw. (n.d.). Long-term Effect of Car Accident Injuries. Retrieved from https://www.kitchellaw.com/blog/long-term-effect-car-accident-injuries.cfm
- Sage Hill Physio. (n.d.). Motor Vehicle Accident Recovery. Retrieved from https://www.sagehillphysio.com/blog/Motor-Vehicle-Accident-Recovery
- Wellness for Warriors. (n.d.). Motor Vehicle Accidents. Retrieved from https://wellnessforwarriorsct.com/motor-vehicle-accidents/
Conclusion
Motor vehicle accidents can have devastating effects on mobility and flexibility, leading to physical, emotional, and financial challenges. Injuries like whiplash, herniated discs, and joint damage can disrupt daily life, but early intervention with chiropractic care, physical therapy, and advanced diagnostics can significantly improve recovery. In El Paso, Dr. Alexander Jimenez’s expertise in treating motor vehicle accident (MVA) injuries, supported by precise imaging, offers hope for victims seeking both healing and legal recourse. By understanding these challenges and seeking prompt medical attention, individuals can regain their mobility and improve their quality of life.
Key Citations
- Motor Vehicle Accident Injuries Overview
- Adapting to Mobility Loss After Accidents
- Personal Injury Doctor Services
- Long-term Effects of Car Accident Injuries
- Nerve Injury from Automobile Collisions
- Immobility Caused by Car Accidents
- Restoring Mobility After a Car Crash
- Emotional Trauma After Car Accidents
- Motor Vehicle Accident Recovery Strategies
- Hidden Injuries from Car Accidents
- Motor Vehicle Accidents and Injuries