Table of Contents
Introduction
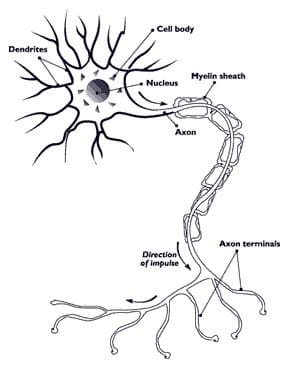
In the body, there are trillions of nerves that inhabit the body and are connected to the central nervous system. The nervous system is split off into two parts which are the central nervous system which consists of the brain and spinal cord, and the peripheral nervous system which consists of the nerves that are branched out throughout the body from the spinal cord. The nervous system’s function to the body is to send out neuron signals all over the body to and from. When there are unwanted factors that start to affect the nerves in the body, it can disrupt the signals from transporting throughout the body and affect a person’s ability to function. In this 2 part series, we will be taking a look at understanding what is polyneuropathy and looking at the different types of polyneuropathies that can affect the body. In Part 2, we will look at what is neuropathy pain and its symptoms. By referring patients to qualified and skilled providers who specialized in neurological services. To that end, and when appropriate, we advise our patients to refer to our associated medical providers based on their examination. We find that education is the key to asking valuable questions to our providers. Dr. Alex Jimenez DC provides this information as an educational service only. Disclaimer
Can my insurance cover it? Yes, in case you are uncertain here is the link to all the insurance providers we cover. If you have any questions, please call Dr. Jimenez at 915-850-0900.
What Is Polyneuropathy?
Polyneuropathy or peripheral neuropathy is experienced by approximately 40 million people in the US, as research shows that it is a result of nerve damage that is located outside of the brain and the spinal cord. Many peripheral neuropathies are mixed neuropathies with both large fiber and small-fiber involvement and are increasingly recognized in the demonstration of specific involvement of small myelinated or unmyelinated fibers, e.g. small fiber neuropathies. This refers to a disorder of numerous peripheral nerves at a given time and is often characterized by a distal, symmetric sensory deficit (“glove and stocking” distribution). Since the peripheral nervous system sends out sensory information to and fro to the brain and spinal cord, polyneuropathy can occur through many factors like exposure to toxins, metabolic problems, and traumatic injuries that can affect the body. Polyneuropathies can also be further subclassified as primarily axonal or demyelinating in nature.
HCTP Therapy

Stem cells* or HCTP (human cellular tissue products) are a form of regenerative medicine that is used by both international and nationally affiliated clinics and distribution organizations used for help individuals that are dealing with chronic pain. HCTP’s function is to help boost the body’s own natural healing process by regenerating damaged cells, repairing diseased tissues, and organs back to their original state and function in the body. As more and upcoming research begins to talk about the beneficial properties of HCTP, many individuals begin their wellness journey without dealing with chronic pain.
The Types of Polyneuropathies
Since polyneuropathy is a multitude of damaged peripheral nerves that can affect the sensory signals in the body, research has found that there are multiple types of neuropathies that can take from hours to days or even years to develop and cause havoc to the nerves in the body. Polyneuropathy can also affect the nerves that are responsible for controlling the body’s primary functions like movement, feeling, digestion, and heart rate.
Mononeuropathies
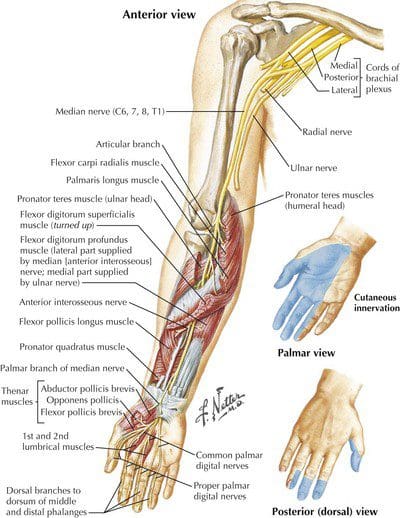
Research has shown that mononeuropathies are single nerve damage that is close to the skin and near the bone causing isolated nerve lesions with deficits restricted to the nerve in question. Mononeuropathies are commonly related to entrapment and trauma that has been affecting the nerves in the wrist. Some of the frequently encountered mononeuropathies in clinical practice include:
- Median
- Ulnar
- Radial
- Peroneal
- Lateral femoral cutaneous
Since there are several individual nerves that are affected by mononeuropathies, it can come in usually at random and non-contiguously and is often related to vasculitis or other inflammatory/autoimmune conditions like diabetes. Some of the examinations reveal deficits attributable to the involvement of one or more isolated peripheral nerves that can cause mononeuropathy to progress into chronic disorders if it is not treated.
Entrapment Neuropathy
Entrapment Neuropathy is nerves that are at risk and are passing through tight fibrous or
fibro-osseous channels. Research has found that entrapment neuropathies are usually caused by compressed or irritated peripheral nerves that are traveling through narrow anatomical spaces in the body. Entrapment neuropathy can cause the body to have mechanical distortion that leads to focal
demyelination and possibly axonal injury to the nerves in the body. Some of the most common factors and symptoms that are caused by entrapment neuropathy include:
- Median nerve at the wrist (carpal tunnel)
- Ulnar nerve at the elbow
- Peroneal nerve at the fibular head
- Increased body mass index
- Predisposed systemic diseases (Hyperthyroidism, diabetes)
Axonal Polyneuropathies
Also known as Diabetic Neuropathy, axonal polyneuropathies are most often distal symmetric polyneuropathy that is consist of large or small fibers that cause autonomic neuropathy to coexist. Studies have found that axonal polyneuropathies are a paralytic disorder that causes motor nerve fiber degeneration and are considered asymmetric neuropathy that may involve cranial nerves, thoracic or limb nerves in the body. Axonal polyneuropathies have resulted from ischemia (vasa Nervosa) and entrapments while also being a result of immune-mediated epineural microvasculitis causing proximal motor neuropathy (diabetic amyotrophy) that causes severe proximal limb pain and weakness to the body. Some of the factors that can cause axonal polyneuropathies can be inherited like demyelinating polyneuropathies and are due to metabolic disorders, vasculitis, and nutritional habits.
Demyelinating Polyneuropathies
Demyelinating polyneuropathies is an immune-mediated/inflammatory autoimmune disorder in the body. This disorder is usually inherited and can be caused by nutritional and toxin factors that are affecting the body. Research studies have shown that demyelinating polyneuropathies can become chronic over time and occur when the body’s own immune system starts to attack the myelin sheath that is around the nerve cells. One of the most common forms of demyelinating polyneuropathies is Acute Inflammatory Polyradiculoneuropathy (AIDP) or Guillain-Barre syndrome. AIDP is an autoimmune segmental demyelination of motor skills that is greater than sensory nerves. Some of the symptoms of demyelinating polyneuropathies can include:
- Facial weakness
- Molecular mimicry (i.e. Campylobacter jejuni)
- Ascending weakness and respiratory compromise
- Areflexia
Another common form of demyelinating polyneuropathies is Charcot-Marie-Tooth. This is a hereditary motor and sensory neuropathy that causes musculoskeletal deformities like pes cavus, hammertoes, and “inverted champagne bottle” legs while causing distal weakness and atrophy to the body.
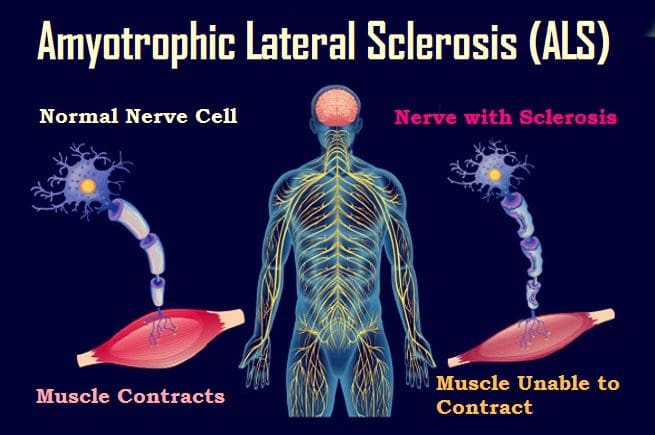
Amyotrophic Lateral Sclerosis (ALS)
Also known as “Lou Gehrig Disease,” Amyotrophic Lateral Sclerosis (ASL) is a disorder of upper and lower motor nerves affecting the nerve cells that are in the brain and spinal cord that causes a loss of muscle control, as research studies show. ALS affects motor nerves with minimal sensory involvement and causes widespread denervation of muscle in the body by causing respiratory failure, dysphagia, and a loss of independence. This may become non-ambulatory since the 2 most common forms of presentation are limb onset & bulbar onset. Studies have shown that since ALS is a progressive neurodegenerative disease of the motor neurons, it will cause paralysis over time and inevitably death 2-6 years after diagnosis.
Other studies have found that when ALS is progressing in the body and affect the primary motor nerves, it can cause extra-motor manifestations like a change in a person’s behavior, executive dysfunction, and cause language problems. When the lower motor nerves are affected it can cause atrophy, weakness, and fasciculations; while the upper motor nerve is being affected as well, causing “long tract signs”, brisk deep tendon reflexes, and pathologic reflexes (eg Babinski).
Conclusion
All in all, polyneuropathy is a multitude of peripheral nerves that are damaged and cause problems to the nervous system in the body. If left untreated over time, it can develop into chronic disorders that will affect the nerves and cause the body pain and be dysfunctional. By making small changes to a certain lifestyle, eating anti-inflammatory foods, or exercising regularly, individuals can dampen the effects of inflammation in the nerves and begin their wellness journey.
References
Brotman, Ryan G, et al. “Amyotrophic Lateral Sclerosis.” StatPearls [Internet]., U.S. National Library of Medicine, 29 Aug. 2021, https://www.ncbi.nlm.nih.gov/books/NBK556151/.
Hafer-Macko, C, et al. “Acute Motor Axonal Neuropathy: An Antibody-Mediated Attack on Axolemma.” Annals of Neurology, U.S. National Library of Medicine, Oct. 1996, https://pubmed.ncbi.nlm.nih.gov/8871584/.
Leonard, Jayne. “Polyneuropathy: Causes, Symptoms, and Treatment.” Medical News Today, MediLexicon International, 3 Feb. 2022, https://www.medicalnewstoday.com/articles/317212.
Masrori, P, and P Van Damme. “Amyotrophic Lateral Sclerosis: A Clinical Review.” European Journal of Neurology, John Wiley and Sons Inc., Oct. 2020, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7540334/.
Medical Professional, Cleveland Clinic. “Mononeuropathy: What Is It & How to Treat It.” Cleveland Clinic, 24 Mar. 2021, https://my.clevelandclinic.org/health/diseases/16014-mononeuropathy.
Medical Professionals, Johns Hopkins. “Chronic Inflammatory Demyelinating Polyradiculoneuropathy.” Johns Hopkins Medicine, 27 Mar. 2019, https://www.hopkinsmedicine.org/health/conditions-and-diseases/chronic-inflammatory-demyelinating-polyradiculoneuropathy.
Schmid, Annina B, et al. “Entrapment Neuropathies: A Contemporary Approach to Pathophysiology, Clinical Assessment, and Management.” Pain Reports, Wolters Kluwer, 22 July 2020, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7382548/.
Staff, Mayo Clinic. “Amyotrophic Lateral Sclerosis (ALS).” Mayo Clinic, Mayo Foundation for Medical Education and Research, 22 Feb. 2022, https://www.mayoclinic.org/diseases-conditions/amyotrophic-lateral-sclerosis/symptoms-causes/syc-20354022.
Staff, Mayo Clinic. “Peripheral Neuropathy.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 3 July 2021, https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/symptoms-causes/syc-20352061.
Disclaimer
Professional Scope of Practice *
The information herein on "Understanding All Types Of Polyneuropathies | Part 1" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card