In today’s podcast, Dr. Alex Jimenez, health coach Kenna Vaughn, Truide Torres, biochemist Alexander Jimenez, and Astrid Ornelas discuss how sciatica can be caused by a variety of health issues that result in the compression or impingement of the sciatic nerve.
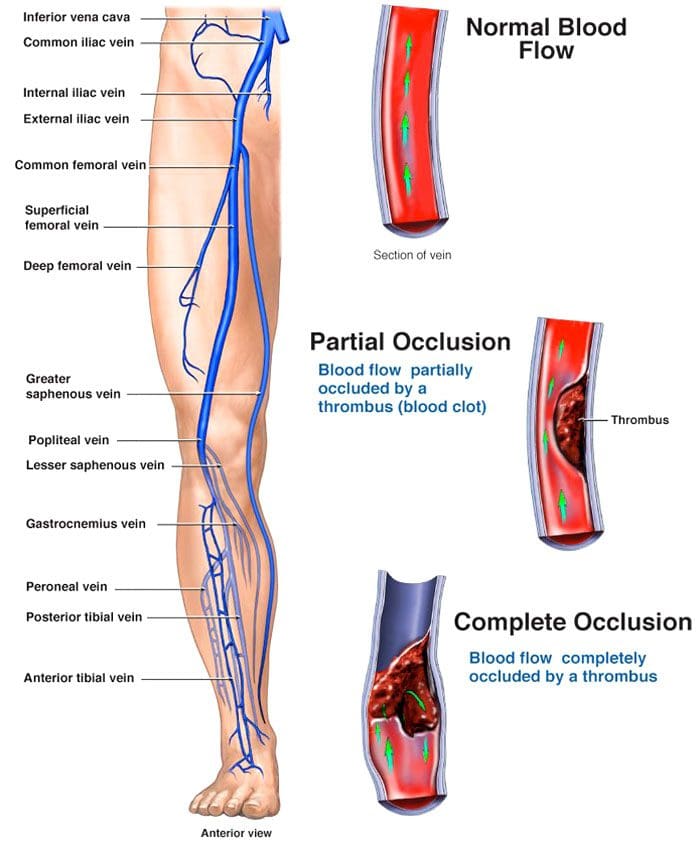
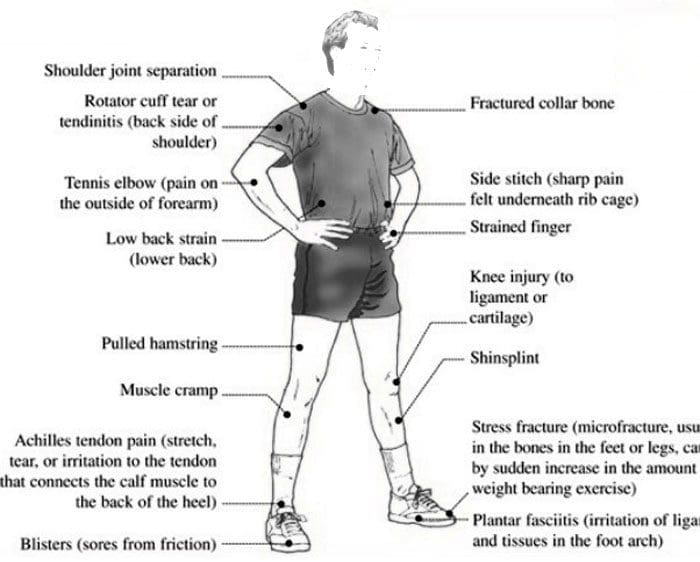
Dr. Alex Jimenez DC*: Hey, guys, we’re live today. We’re going to be discussing the scourge of the back, the scourge of the back for myself. I’m a chiropractor practicing out here in El Paso, Texas. We usually have a disorder that’s typically there isn’t a day that we don’t see it, and it affects so many people. But there’s a lot of confusion with, and I call it, the scourge of the low back. It’s called sciatica. Sciatica is a disorder that has many, many reasons and many, many causes. One of the most important things is first to assess the reason and cause of sciatica. But most importantly, when it first hits an individual, it strikes them, usually with a shocking misunderstanding as to what’s going on in their legs. They feel pain in the low back. They sometimes feel pain in the leg. Different areas depend on where the issue lies, so a little bit of its anatomy breakdown and explanation of what it is. First of all, it’s a syndrome. It’s a syndrome that has many reasons and many causes. The issues that come about and are that that make sciatica arise are vast. I would venture to say that there are a million people that come in with sciatica. There are a million reasons that have presented each one of those patients. There is a majority of problems in and a subset of issues. We’re going to go over that. Today, our goal is to bring out the awareness that it is a problem, just like the present anemia. And there are many reasons why a person would have anemia. Many people are familiar with anemia, and they say that’s low blood, but you’re going to find out where the blood issue is to determine exactly what the causes of anemia are. Well, the same thing with sciatica. There’s a lot of reasons why the sciatic presentation occurs. So we’re here to kind of begin the process of explaining that. So we’re going to get real deep and down and nasty with the science of it. We’re going to try to give you some tools that you can look at and assess. So your provider can give you a better explanation, or you can ask better questions in terms of where your sciatica originates. So the first thing is to understand the anatomy, and I’ll go through the anatomy in a very visual way. But I want to first kind of take you to a visual, and my visuals are very three-dimensional and offered through complete anatomy. Complete anatomy has given us the ability to use this and show, and it is something that many medical students use. So in today’s modern-day, we don’t have to use some visceral or some sort of human anatomy. We can use these tools to help us present to the patients and to teach. So it’s probably one of the most used anatomical structured systems, and we use it to teach people in our patients every day, given the dynamics of sciatica. Here we have a picture of a sciatica HDMI, so we can see a presentation of what the sciatica nerve looks like when we can see it. The interesting dynamics here is that when you look at the interesting presentation, you can see as I go away how vast and how large it is. Now the first thing is I rotate this individual. You got to see that it comes from a large glute plexus in the lumbar spine to the sacral nerve roots. So anywhere down the line that anything is touching this thing, this beautiful, powerful nerve, you’re going to find that there is pain radiating down. So we’re going to discuss those issues. And as we kind of go over that, we want to understand that so away from HDMI. So what we’re looking at are the issues that present with us when we discuss it. So what are the causes, and what is sciatica? Sciatica is inflammation of the sciatic nerve, and as it presents what happens many times, it is the largest nerve in the body, and it’s how most people know it, and it travels from the lumbar plexus to the leg. So, anywhere that that thing is touched, it’s going to radiate pain. Now, what are the causes? Well, they could be from vascular. They could be compressive. They could be lymphatic. There could be a space-occupying lesion, such as a tumor causing the issues. Now, a good clinician will do a lot of different tests and a lot of different assessments to determine where it is having the problem. So when I have a patient, they come in when the first thing we have to do is a history we have to assess and find out what’s going on. So finding the history of something that suddenly someone starts sitting or they become active, or they get hit in the back, and they start having sciatica, it boats to a well, dynamics. So what happens is, what we need to do is we need to discuss the dynamics of where it begins and what goes on. So in terms of our direction, I would like first to take you to the physical assessment. When you explain to your doctor what’s going on, you need to tell him exactly when you started having it. That’s very important. The history is very like when these issues are? Do you have a sedentary life? So these are the types of issues that present most of the time a person comes into the office with having a severe presentation that they’re shocked? They didn’t expect this and what occurs in this particular area is that you can see where the nerve root comes in. So over here, you’ve got to figure out where it came from. As you notice, a lot of the reasons that many of these individuals have is because it’s a little bit of atrophy and muscular issues that arise. As you can see right here, there’s a lot of areas where the nerve can keep becoming trapped, and this is the main reason that most people have this issue now as they go through this and they present a symptom. I got to figure out, and we have to figure out where the problem originated with our team. So as I go through that, I want to give you a different dynamics here in what I’m going to explain. I’m going to present my team to you so that they’re all going to. Each one of them is going to explain a little different aspect of what goes on. Today, we will discuss how a coach, such as an individual helping the doctor, can assess the situation. We are going to talk to our coach Kenna. We’re going to talk to Astrid, who’s going to bring some science knowledge here. We will bring a patient in, discuss the experience with her, and bring in our top guy from the university at the biochemical level. He will teach us a little bit about some nutraceuticals and some applicational processes that we can do to help an individual with sciatica. So at first light to tell, I like to ask a question to Kenna. So Kenna, what I want to do is I want to ask you exactly what it is that you notice when a patient presents with sciatica and what kind of things we can do in the office and what’s our approach specifically more like the metabolic issues and the disorders that present that way? So when we’re looking at here, let me go ahead and head into this area, tell me a little bit about how we present a patient and what we deal with when we’re talking to an assessment or doing an assessment.
Kenna Vaughn: So one thing that many patients with sciatica have is the pain they’re feeling, of course and that low back. But another thing is they don’t have a lot of movement due to that pain, and movement is essential. It’s what life revolves around. So we take that movement, and we look at how we can help this patient decompress that sciatic nerve with the adjustments that Dr. Jimenez does, but also how can I benefit from my side of things for this patient? So we do have a lot of great resources available to us. We send our patients to Push, which is a gym here that helps them get that calibration in their muscles that they need to build up those stronger muscles all around that sciatic nerve so that this nerve doesn’t get pinched frequently or as often. And another thing we have available to us is an app called Dr. J. Today. And what that does is it syncs with the bracelet that our patients wear, which allows us to track their movement. So we want to focus on that movement as part of it. And another thing we can do is nutraceuticals in supplements. So what are nutraceuticals and supplements? One of the main ones we focus on that almost every individual should be taking is vitamin D3, and we like it coupled with vitamin K. This will help your bones and circulation. And it’s going to help to decrease that glucose by increasing your insulin sensitivity. And this is where it comes into play with sciatica.
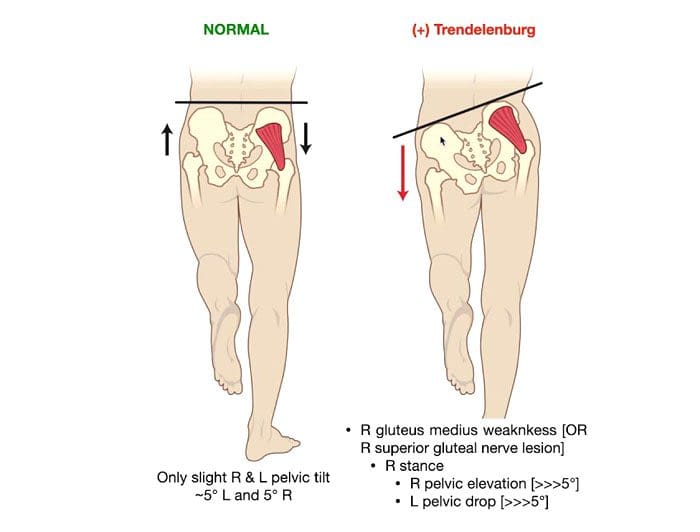
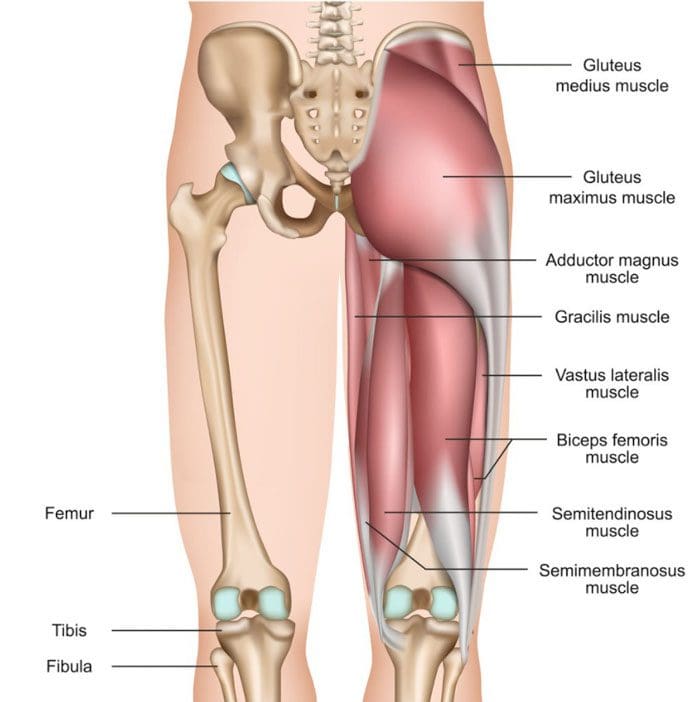
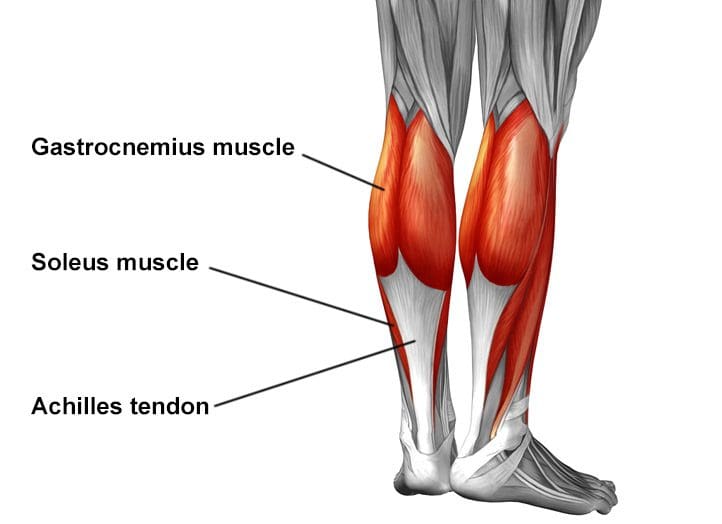
Dr. Alex Jimenez DC*: I had a question for you in terms of that. When you’re discussing that we’re dealing with and sciatica as a pain in the hips, we’re correlating, and we’re tying together, I guess, a disorder that many people have as metabolic syndrome and many times are overweight. And that was one of the presentations that many of the patients with sciatica, not that everyone is overweight, with sciatica. Still, many people who become sedentary and don’t move as much do suffer from metabolic syndrome. So to get that under order, one of the things is to bring the insulin under control. And once we do that, we start losing weight and getting more active with the exercise protocols. She mentioned Push because we began to calibrate the hips. Now, as you can tell from our picture here, there’s a whole lot of muscles in this region, OK? So as I kind of use the application, you can see a little bit more of the muscle tissue that is involved. So as we look at the muscle tissue, we can see that calibrating and these muscles that control the hip actually propel the creature, so propel humans, so to speak, right? So what happens is as this happens, if this becomes deconditioned through a sedentary lifestyle. Well, the thing that’s lying underneath also stops working, and the muscles stop working as effectively. So one of the ways that we treat people is through a coach to assess their body mechanics and put them through the Push Fitness protocols that can help them get a calibration of the structures. One of the things that we also do in this process is we look at the sitting issues and tell me a bit of what you do, Kenna, in terms of helping people adjust their lifestyle or modify their mobility issues.
Kenna Vaughn: So what their mobility, as I said, we use the app, and we also use Push Fitness, and the supplements have a lot that comes into play because like I said, with that increasing the insulin sensitivity, what we’re going to want to do it, that is it’s going to help to control the blood sugars. And you might not necessarily relate blood sugars to sciatica just yet, but as I said, everything is connected. So when we put our patients on a protocol and have them control these blood sugars, it also helps maintain their inflammation because sugars and chemicals cause that inflammation in the blood. And that’s also it’s going then to cause nerve damage to our body and our system. And then, once we have that nerve damage going, we’ll see many more patients sitting down, which relates to that lack of motion. And then we see a lot of patients coming in with sciatica.
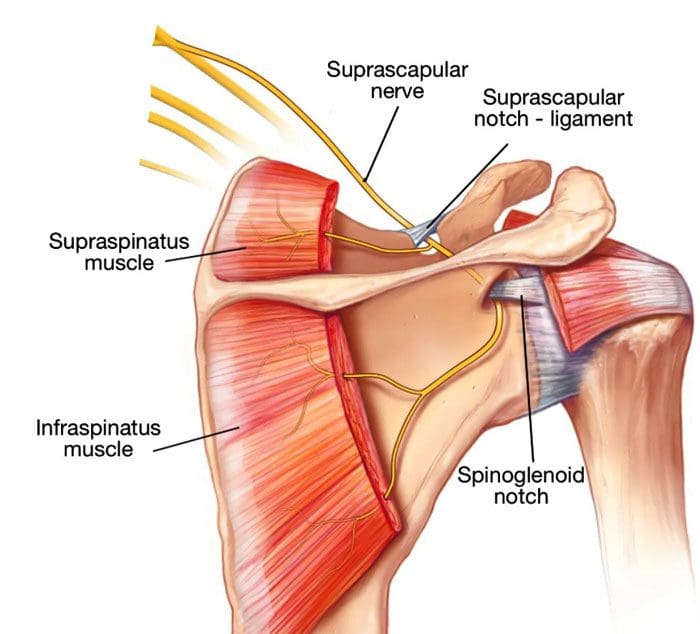
Dr. Alex Jimenez DC*: Sciatica. So basically, we’re going back to the same monster, which is called inflammation. Right. So inflammation is the deal. People that have sciatica will often tell the story of how it kind of looms with them. It’s like having this untrustworthy nerve back there that if they have stress or go through emotional dynamics, it affects sciatica. So this threshold that activates the sciatica presentation could have even an emotional component to it. So we want to bring that to light, too, because many people have normal lives, but they don’t have the presentation under normal situations. Suddenly, bam, they get an emotional, financial issue, family things, and sciatica just flares. Where is that even logical, right? The key is inflammation, inflammatory response, stress responses. And those issues do create an almost perfect storm to create a predisposition for inflammation. So that’s why we bring in the dietary components and the food to start eating better to prevent inflammation again. Those are some of the things. So she also mentioned the issue of Push. Push is our fitness center, where we actually put people through exercise protocols, and when we start putting people through exercise protocols, it’s there to calibrate. Now, what’s the biggest muscle in the body? Well, not too far from the anatomy to an anatomical structure. You can see the muscles in this particular area, and everybody knows that the glutes are the big muscles. So when you see this powerful muscle, if this muscle becomes decalibrated from a sedentary lifestyle, you’re going to notice that you’re going to have a lot of predisposition. So it’s like a car with flat tires. So if the car has flat tires, it starts swaying and moving to the wrong side. Well, if it’s swing, you can imagine that it affects the axis and the axles, and all that kind of stuff starts happening. Things like these happen, but in our human structure, there’s a finely calibrated system here. One of the things that many people don’t know and don’t think about is the lymphatic structure. Now, if you can see here, you can see the lymphatic. Now those guys ride directly next to the venous and arterial structures, and you can see it here. So as you can see that for progressing, you also look at the arteries. So if someone doesn’t have an arterial system that is working well and sitting on this, you can see congestion occurring around the structures, around the nerves. Now there’s a lot of nerves in here. So when you start looking at these dynamics, you start seeing that a person who is not using their muscles has an increased congestion level. So as I remove these muscles here, you can see this picture, and I’m going to remove every one of them. You start seeing the noticeable dynamics of how complex their nervous system is. So over here, you can see the complexity of how those nerves function. It’s amazing to see all the structures in here. So when you look at this, you can see the amount of influence that lack of movement would cause. It’s almost like a traffic jam. Imagine sitting on this thing all day long, OK, let alone be inactive. So one of the things we want to do is to assess exactly what it is. And one of the things that we do is to calibrate the system. So going back to removing these picked areas, you want to go ahead and work on the big systems. OK, well, as you can see, these muscles bring a huge component into helping sciatica. Now, where are the sciatic issues coming from? Now let’s go ahead and start discussing those particular issues as we can kind of go through this. And I want to take you through a little anatomy lesson here because it does require a little bit. As I remove these things, we’re going to see all of the structures that come in, and actually, but you can see if I can get the nervous system only out to the minimal component of it, the big ones. And as you can see here, you can look over this way and see anywhere down the line right here by where the nerves are. Them out where the disk comes out in this particular area as it penetrates forward, it goes this what we call the sacral notch, which is this guy right here. This hole is a sacral notch where it comes out, and you can see that it can be bumped into the bone and the actual femur here. So there’s a lot of areas that we can see that directly affect the sciatica regions. But having gone through that, I’m going to go into that in a little bit deeper. But I want to go ahead and get a little personal story right now. I want to ask an individual now what sits in here, and most women, you know, this is where they contain babies, right? So in a situation where you have an individual that is going through a lot of changes, such as an individual who’s having a child, you can see where the hips actually change and right down there, if you can see down there, this is where the sacrum has to open up to allow for the birthing canal. You see that big hole right there. A baby’s got to go through there, and if it can’t go through there, which it probably won’t until probably the ninth month where this area starts expanding, guess who’s going to go by, then kick in on the way down? OK, that would be a child. OK, so let’s talk about that. I’d like to present Trudy here because she has a story of how it affected her.
Trudy Torres: Well, I guess, you know, as a woman, you know, it’s an extremely joyful situation when you find out that you’re going to be a mom. If it’s your first-time baby, you’re in for a roller coaster. You know, like you guys were mentioning, there’s a lot of different scenarios that you go through emotionally, physically. So when you’re pregnant, you’re the perfect storm for something like this to come up. You know, you are just balanced from you’re so, so tired the first trimester. I’ve always worked out. So for me, I have never experienced sciatic pain before, and for me being so active, I went from being 100 percent active to just being so tired. I had to be super careful about spending my energy, especially in the first trimester. So on top of that, if you add, you know, everything else that’s going on physiologically with me and then my life became so sedentary. On top of that, you know, I have a desk job. So sitting at a desk and then not compensating, moving all of a sudden, that pain is so excruciating. I did not experience this with my first baby. I experienced this with my second child. And, of course, I gained more weight with my second child. So once again, you know, you’re adding problem over the problem. And just because you’re pregnant, that doesn’t mean you’re eating for two, because unfortunately, some of us, you know, have that misconception, and that’s when your weight tends to get a little bit out of control. So you’re adding a lot of different factors that create the perfect storm and are just super, super hard. One of the things that Kenna mentioned that helped me was becoming active and being exposed to Push. I had someone here that was able to work out specifically with me being pregnant. Obviously, my limitations as you start gaining more weight, it’s not the same thing that you can do when you’re not having a baby. So I was able to continue to work out later on in and, you know, after I was exposed to chiropractic and implementing exercise.
Kenna Vaughn: So the main symptoms you had when you had sciatica, and you were pregnant, was it mainly just pain, or did you also get that tingling feeling because there is more than one symptom of sciatica?
Trudy Torres: No. Unfortunately, it was just not pain. It was pain. It was burning all down my leg. I did not know what was going on. As I said, this was not with my first pregnancy, and every pregnancy is different with my first child. I watched more what I ate. I was still active, so I believe it was a combination of things, you know, that I felt like I was eating for two. I gained more weight than I should have.
Dr. Alex Jimenez DC*: I got a question: Was it when you rapidly gained weight during the final trimester?
Trudy Torres: I think everything kind of started happening a little at a time. I wasn’t that active in the first trimester, so I began having flare-ups not as bad as once I gained the weight. But, you know, once I gained more weight, that’s when I started having more severe symptoms, as I said, the burning, the lower pain. It was just excruciating, and it’s something that I don’t wish upon my worst enemy.
Dr. Alex Jimenez DC*: Now, did you ever have a recurrence after you had your baby?
Trudy Torres: Yes, I did. I did, and unfortunately, I did, but one of the things has helped me keep that under control. It’s been being active, continue to watch my weight. My supplements were one thing that I would ask Coach or Dr. Jiménez when you’re pregnant. I know we were talking about the different supplements. What do you still recommend for pregnant women to get on the different vitamin D and K supplements?
Dr. Alex Jimenez DC*: That’s an excellent question, and one that I’ll answer very clearly as a wide disclaimer; you need to make sure that your doctor knows what you’re experiencing. Obstetricians, which are OB-GYN doctors. They’re very well astute as to what type of supplements. So in the world of supplementation, it is wise to have a doctor assess that, and many of them will make sure that you have good supplementation. The area where it’s the accurate assessment is you have to have supplementation. Your body’s trying to produce an enormous amount of cellular activity as it creates life. It draws upon a particular area that inflammation goes crazy, the body goes into dynamic changes. So nutrition becomes an essential thing from intestinal nutrition through metabolic nutrition. So one of the things is that you have to have a doctor, typically today’s individual who is in there as young childbearing age, they have a doctor evaluating. So yes, one of the essential things is from folic acid to vitamin E, D. These are a whole, complete gamut of vitamins that are assessed and given by their doctors. So most women will know that if they take some medication, they have to put it clearly by their doctor. That’s the most important thing. And the second thing is on the supplementation side; once your doctor knows, he’s probably going to give you something of a basic level of supplementation and nutritional assessment. So in terms of that, a dietitian can evaluate you and assess you and determine what’s going on in terms of the aggressive approaches where an individual is not pregnant; there’s a lot of things that can be done. But let me ask you this. I know that you do a little bit of a CrossFit, and you do that kind of stuff. And you mentioned that you had sciatica after. I want to go to the point that many people who have sciatica lead a predisposed life to sciatica now, meaning that once you get it, it’s not that your terminal is that you always have the potential of having it, so whether your body dynamics have changed. Typically, you’re not 18, and now you’re 40. What happens is your body is warning you that it’s not working as it should be. And suddenly, the nerve starts becoming flared up, either the compression through atrophy of muscle or imbalance of muscles. So all those things are essential; I notice that you mentioned something that you did. It also affected you after. Did you do some competitions later, and did it affect you?
Trudy Torres: I did do competitions after. What helped me keep it under control was that its different factors to keep it under control. You know that keeping moving makes sure that you’re taking the right supplements in chiropractic care. I’m a firm believer, you know, of a holistic approach, and I believe that a combination of all it has helped me keep it under control. I have not had flare-ups, but I believe it’s because I’ve had all these different combinations. As I said, you know, I kept active. I have, you know, been in average weight. I have also implemented chiropractic, you know, as maintenance.
Dr. Alex Jimenez DC*: You know, I would like to give people a kind of insight as to what happens when you first go to a doctor, and they assess you; there are many ways to figure it out. One of the ways that it’s an easy way if there’s degenerative and there are bone changes is an x-ray. And that’s what we typically look at, and we first start all assessments. But the definitive assessor who gives the vast amount of information is looking for some compression. And at that point, sometimes we have to look at the arterial-venous circulation. But the number one way to determine if someone has sciatica due to a disc injury or some compression or space-occupying lesions like a tumor or some arthritis or some sort of imbalance in the muscle is genuinely the MRI. The MRI is an excellent tool. Now, if there is bone involved, a CAT scan is used. The EMG is used to determine the muscular tone and the muscle’s ability to react and see which tone levels. But you don’t need to be a rocket scientist and put someone through that. They already know that their muscles are tight, and there is an issue. The ability to determine how the nerve functions is a nerve conduction velocity test that tells you how fast and slow the nerves could work. Now in the situation where we do a bone scan, we’re trying to look for any metabolic issues outside, and there could be a tumor or some problem. But that’s rare, and that’s not typical, but the number one way to assess an issue is through an MRI and an X-ray. Those will give you the most significant, broadest areas. Now I want to go ahead and talk a bit about nutraceuticals and specifically nutraceuticals. We’re going to go ahead in this about the treatments for it. And as we go through that, I’d like to go ahead and discuss certain areas and specific supplements. Now Astrid is our resident nutraceutical information gathering. We also have a biochemist in the background who will bring some insight to a different level. But what kind of things do we typically offer patients when they need it as a metabolic, a leaving protocol?
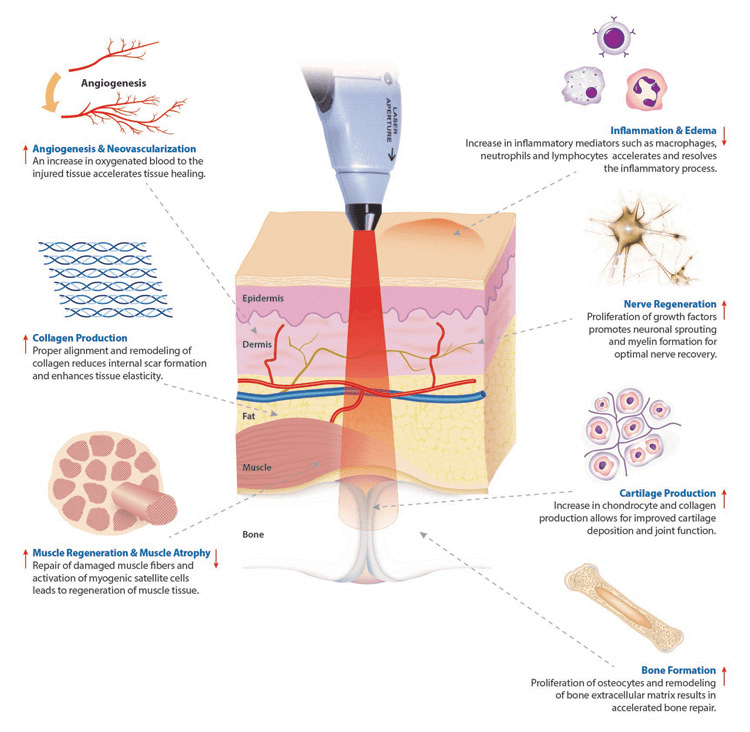
Astrid Ornelas: OK, well, first of all, I want to bring in an interesting statistic. According to researchers, approximately 80 percent of the population suffer from some type of back pain. Included in that are low back pain and sciatica. So with that being said, of course, it becomes a priority to know what is it and what can we do to assess this common problem? And like, Kenna and Dr. Jimenez, like you and Trudy have said, exercise is essential. And together with exercise, we want to bring in a diet. We want to eat foods and supplements. And because obesity or excess weight is one of the problems is one of the leading causes or one of the most common, commonly well-known causes of sciatica. We want to, you know, all together with exercise and following like a good, a good diet. We want to follow these things so that we can. If we lose weight, it can help improve sciatica. So with that in mind, there are several of them. I guess natural remedies, natural nutraceuticals, if you will, can help reduce or improve sciatica symptoms and, therefore, lose weight. So one of the ones that I want to talk about is that we have it here: turmeric or curcumin. So turmeric is a plant, it’s a flowering plant, and it’s related to ginger. And we eat the root. That’s what we know it. This yellow kind of orange-looking root is very commonly used in Asian foods and most commonly in curry and curcumin. You’ll hear turmeric and curcumin used a lot interchangeably together, and curcumin is the active ingredient that’s found in turmeric. So one of the things that I wanted to bring up with turmeric and curcumin is the benefits that many people can take, and they can either eat turmeric or take turmeric supplements. It can help to reduce sciatica or sciatic nerve pain. So turmeric has a lot of anti-inflammatory properties, which can help reduce pain and swelling, which is probably one of the most common symptoms of sciatica. There’s a lot of research studies that have found that turmeric or curcumin can reduce neural inflammation, which is inflammation in the nerves, which, as some of us here, know if your sciatica is caused by a disc herniation or a herniated disc, sometimes the substances or the chemicals that are inside of your disc, they can irritate the nerves. So taking turmeric and curcumin can help reduce the inflammation caused by these irritating compounds. It is also a powerful antioxidant that can help reduce oxidative stress, which can cause inflammation. And probably one of the highlights of taking turmeric or curcumin is that it can improve metabolic syndrome, as we previously discussed in a past podcast. Research studies have found that turmeric can help regulate body fat by reducing inflammation. It can also help lower bad cholesterol. It can lower triglycerides. It can improve blood sugar levels. And it has antibacterial properties as well.
Dr. Alex Jimenez DC*: Let me ask you. We’re talking about the potential of someone having sciatica; since some people have sciatica, that kind of looms on them. Well, we’re trying to do with turmeric, and we’re trying to prevent it from kicking off. So it’s basically like prophylactic prevention. I like to go a little deeper, and we have our resident scientist here, Alexander, and he is right with us right now, and he’s got some points of view on some of those supplementations. Tell us a bit of what you learned in terms of supplementation and your point of view on how we can assist sciatica from a biochemical point of view.
Alexander Isaiah: Well, there are a couple of different ways of taking different perspectives and avoiding the whole. An inflammation response is a good way of saying it. Let me see. Can you guys see my screen here?
Dr. Alex Jimenez DC*: Yes, we see you, we see you right now. So I saw your screen. Yes, I do. We see the screen entirely.
Alexander Isaiah: Awesome. So I’m going to go into a little bit of the biomechanics of what’s going on with sciatica. Then we’re going to break down a little bit of the muscles, and then we’ll go into the supplementation aspect of what we can do to have either prevention or active treatment during treating sciatica. So here we could see we have three individuals from left to right. The first one is an individual who has a neutral spine. And you can see that as we draw a line down the middle there. External auditory Matis, the ear, is in line with their deltoid and is in line with the median part of the sacrum. In the second person, we can see that they have a little bit of dysfunction in terms of their physical aspect. So here we have an individual whose sacral promontory, which is the anterior side of the sacrum, is tilted superior, and their posterior area is tilted, posterior, inferior. I’m sorry. And what this is called, this is called a counter mutation. So by having that sacrum pointed up, you’re putting more stress on the thoracic region and causing the areas to be more inclined to different stresses. And most of the time, this is caused by tight hamstrings. So these hamstrings are pulling down, forcing the anterior side to come up and stretching these quadriceps. So it can either be done from an imbalance of over-powerful hamstrings or tight hamstrings and weak quads. In the third individual as we draw the same line down the middle. We can see that they are almost in line, but on an individual like this, we could see that their sacral promontory, the front side of the sacrum, is tilted anteriorly, which is called mutations. So we have a counter mutation over here. It’s going to go counter. And then mutation over here on the right side, so an easy way to remember this. They’ll stick forever is that this is pretty much if you think plumber’s butt, this is what it looks like. This is what J-Lo looks like. Oh, so you’ll never forget it that way. But the difference is here is that here the pressure is on the thoracic spine. But in an individual with notated hips, the pressure is in the lower back. So let’s say someone is pregnant and developing another child in this area. They’re going to be putting more pressure on the lower back versus someone who has pressure on their thoracic area. They’re going to be more pressure there. So going into a little bit more of the anatomy. We can see that we have all the different muscles here, and we could see the piriformis, which is this muscle right here. I’m going to give you different colors for you guys, so that you can see better. It is muscle right here. And then we could see the superior gemellus is right under that. So sandwiched between the two is the sciatic nerve. And if we have someone who is mutated, they’re going to be stretching these muscles more and putting more compression on that sciatic nerve, causing that area to be more inflamed. More of those neuropathies are occurring, shooting down the leg. And then in other instances, when we have the piriformis, which is split in half and the sciatic nerve is running between them, and that’s 10 percent of the population that that usually happens. And so and these people have always had sciatic problems. So by strengthening and working on those conditions and going over those nutraceuticals, we’re about to go into, we can treat and alleviate some of those symptoms. So the first one I kind of want to go into is a little bit of niacin. So niacin, we all see it as the store brand as something popping up like that. And most of the time, it’s either in 250 mg or 500 mg of capsules or tablets. I always recommend getting the tablets just because you can take half of the tablets. And I tell people this is because most of the time, nicotinic acid is the main thing is, vitamin B3 causes a little bit of a flush effect, but that’s just the way it works. So we’re going into it here. We can see that nicotinic acid, as it’s going through its chemical pathway, actually produces lots of NAD+, and NAD+ is essential in the cellular metabolism of many tissues. So going into brief biology, we all know that the mitochondria are the powerhouse of the cells we were all beaten to death growing up in basic biology. But as we take a look more in-depth at the structure of the mitochondria, we could see that it has an outer membrane, an inner membrane, and then an interim membrane space. So we’re going to look mainly at this little section here that’s folded in between, which are called the cristae. And we could see that the first complex, known as complex one or all the known as any dehydrogenase, is responsible for using NADH, converting it and using its protons, and moving it across the gradient to make ATP. But we could see that more NAD+ is produced here, right? So that’s where niacin comes into effect. We supplement more with NAD+ to cause a reduction reaction between NADH and some other electrons, forcing it into NADH. So what does this all mean? Pretty much what we’re doing is we’re creating a boulder downhill effect, so we’re making more NAD, and we’re forcing it to go to product. And how does this happen? Just easy thermodynamics is you put a lot of it up the hill. The enzymes are going to force the work to go down the hill and make more energy. In doing so, and you have a more healthy metabolism of cells. And this does not only correlate to neuropathies, but it also helps with circulatory function, cardiovascular health; the main multi nucleotide muscle in the body is the heart, so you’re not only making sure that you’re neuropathies are covered, but as well as you’re making sure that you’re keeping a healthy heart just by supplementing with vitamin B3. Another great one, saying that you have more ATP produced and more functioning and healthy tissues, is green tea. I chose to use green tea because it has a very similar pathway to curcumin in the sense of anti-inflammatory effects. So the main ingredient in green tea in case you either have green tea in your house or curcumin available, whichever one’s easiest for you, they mostly have the same chemical pathways in that they inhibit either inflammation or cell proliferation neural damage. So the main chemical in green teas is called catechins, and catechins are similar to catecholamines, like epinephrine and norepinephrine, which is just adrenaline. And the main one is EGCG. The cool part about EGCG is that it inhibited NF Kappa B and ROS. ROS is just a reactive oxygen species, which is just free radicals, which can cause havoc and wreak havoc throughout your body, which is why it’s an antioxidant. So in doing so, it prevents NF Kappa B from producing any proliferating effects from cells or inflammation or neural damage. Now, if we go more into biochemistry, I can just break it down a little bit here. So EGCG will upregulate AMP. High levels of AMP will down-regulate this enzyme, called glycolysis, and allow for ATP to be converted to CATP. This is important because not only does the CATP break down things, but it mainly breaks down any adipose tissue and helps kill any cells that are proliferating too quickly, such as cancer cells. And it also keeps cells functioning properly, such as neural cells. So as we’re coming here, another cool part about green tea is it has small amounts of caffeine. If you are pregnant, we don’t recommend that you do any caffeine or stimulatory effects. Always consult with your doctor before taking any of these things. Specifically, something that does have caffeine and that we just doesn’t want to mix anything, especially during pregnancy. But if you are trying to make sure that you help your sciatica or your metabolic syndrome. Green tea has another effect. Using caffeine, which inhibits phosphodiesterase and phosphodiesterase diseases, is responsible for turning off CATP, so it’s a double whammy effect. Not only are you burning fat and shutting down glucose storage, but you’re also allowing for this catabolic or this structure that breaks down things to keep going. Here’s a little bit of an overview of the different things that green tea does and how it helps. And just kind of going into another cool part about green tea is that it binds to other very toxic things, such as iron. We know that we have iron in every red blood cell, but people who have hemochromatosis have too much iron in their blood, and they have to give blood about once a week. Someone who has hemochromatosis can take supplementation of green tea and reduce their iron levels, preventing any toxicity from those iron.
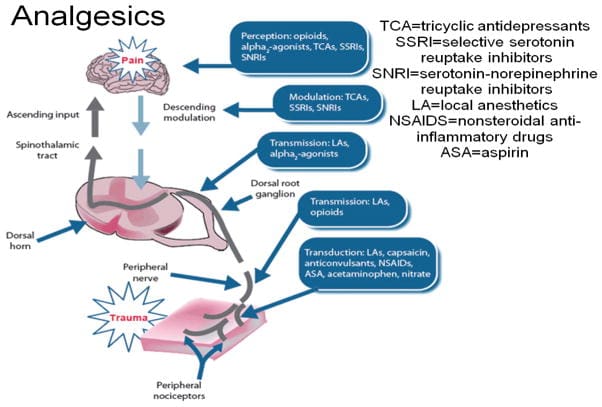
Dr. Alex Jimenez DC*: You know, when you’re talking about those pathway patterns, you remind me very clearly that many of the times, the whole idea behind our show is to try to give you natural ways. However, there are potent medications that work with these pathways, one of which is gabapentin, used for neuropathic pain. Many people don’t want to do that because of the side effects and the critical issues that it causes. We were looking at this in a natural format in a natural way. Going back to the metabolic, what are the things that we notice in the metabolic areas you have seen? What are the other supplements? Do you notice that I have been able to assist people in recovering from because Astrid mentioned turmeric, and that’s the line we’re using. We’re using the anti-inflammatory. They’re limiting, limiting the reactive oxygen species or the ROSs to prevent the inflammation from occurring. Is that correct?
Alexander Isaiah: Yes. OK. The main thing is to inhibit the production of NF kappaB, which both curcumin, other known as turmeric, both have the same name. They’re interchangeable and green tea, and both inhibit these inflammatory pathways and cancer pathways.
Dr. Alex Jimenez DC*: Yes. So let me ask you, Astrid, in terms of those inflammatory comments. Tell me a few of your thoughts on this particular matter.
Astrid Ornelas: Well, I wanted to add another compound that can benefit sciatica or sciatic nerve pain. And that is called alpha-lipoic acid or ALA. And so ALA is an organic compound, and it is produced naturally in the body, but of course, in smaller amounts. Or it can be found in foods such as red meat or organic meats or in plant foods such as broccoli, spinach, Brussel sprouts, and tomatoes. Or it can also be taken as a dietary supplement. And I wanted to discuss the effects or the benefits of alpha-lipoic acid. Because just like green tea and turmeric or curcumin, ALA is also a powerful antioxidant, and it helps reduce inflammation, according to several research studies. And it can also have a lot of benefits for people with metabolic syndrome because it can help lower blood sugar or blood glucose levels. It can improve insulin resistance, which is, you know, an effect, or it’s something that they can that can ultimately cause diabetes. And several research studies have also found that alpha-lipoic acid can also improve nerve function, which, you know, people with sciatica or sciatic nerve pain, especially caused by neuroinflammation. ALA can also help improve nerve function in these people.
Dr. Alex Jimenez DC*: OK. That’s an essential point of view. As you can see here on our list, we have quite a few different presentations and areas such as vitamin C, vitamin D, calcium, fish oils, omega 3s with EPA, berberine, glucosamine, chondroitin, alpha-lipoic acid, acetyl-l-carnitine, ashwagandha, soluble fibers, vitamin E, green tea, and turmeric. As you can tell, there’s a lot of things that we can do to stop the inflammatory cascade. We’re going to be going into all those because sciatica is so complex and diverse that we have to find the best for the patient from the millions of presentations that it has. So throughout the anatomy, as we discussed, and I’ll show you back the anatomy in a second here, you can see that there’s a lot of physiological and as Alex presented biomechanical imbalances that, if not taken into consideration, we will end up with issues in the future as a result of these predisposing dynamics. Now, as we recover these dynamics, we’re going to discuss many different topics. So I wanted to at least give a little more on the side of the things that we do now in terms of differential diagnosis. Many other issues can cause these presentations and from, you know, the dynamics of just a compressive nerve through space-occupying dynamics. We have other areas that come in and affect the patients. So what we’re going to do is in the following seminars, we’re going to go over specific types of things we can do, but let’s give you some guided ideas in terms of the treatment protocols that are out there. We have chiropractic care, which is a form of chiropractic. Chiropractic means mobilizing joints and moving the body, and there are thousands of ways we can do it. A lot of people think that it’s just manipulation or adjusting the spinal. We have to take a lot of things into consideration. We work on the bones; we work in the muscles; we work on the counter muscles. We have to formulate many dynamics to figure out what’s best in line to assist each patient. Once we find out the cause and find out what we call etiology or the pathology and the problem. We can go and use different methods. We use acupuncture, nutraceuticals. We work hand in hand with different providers to provide medications. We also do the goal ultimately in sciatica is to eliminate any chance of surgery if there is a surgical need or that needs to be done. But that’s such a small dynamic that we don’t want to go there unless we have to. We have different other protocols in different methods of treatment, like dry needling. We do aggressive rehabilitation. Now, why are we doing rehabilitation? Because as you saw in the picture earlier, the muscles we have were extremely involved in calibrating the hips. We want to make sure that we, we determine now over here, we got some basic care. We also got some aggressive care. Now, as you know, some basic care will be like ice-cold ultrasound, tens units, spinal adjustments, lifestyle changes, which is pretty much the biggest one because most people end up in a chiropractic office because their lifetime lifestyles change. Now, what do I have? I have a person who was an athlete at one point that suddenly got a desk job and now doesn’t move as much. Well, that’s easy. We can start getting that person back into yoga, pilates, tai chi, getting their bodies to align pelvically, and their whole body structure to get back to where it should be. Here’s the deal as soon as you can get past the inflammation and prevent that, and we can get you to move your body in a way that you did when you were a child, kind of like moving, dancing, and walking. That’s the way to calibrate the glutes. This is a powerful muscle, and as we’ve learned through technology and science, immediate atrophy occurs with the muscles not used. So imagine what happens when you start getting a job, and you used to be an athlete, and now you sit down eight hours a day, that’s going to give some great dynamic. So one of the crazy components is that as I look at this, I give you an idea of the types of exercises we can do. We can go into the extreme kind of CrossFit environment. And if we look at that, you just don’t look at the crazy structures, but you see people moving dynamically. A lot is going on here, and you can see that we can come up with our rehab centers. We have extreme athletes, too, even the people that are, you know, able to move just a little bit. But the point is that as we do this process, we can help someone with the treatments and protocols occurring, as you can see in this particular area. We can see Trudy and me. This is one of the things that the reason I was alluding to. But we can see when you were doing some self-treatment here. Tell me a little bit about what you were doing and what you were experiencing at that point.
Trudy Torres: That was, I believe, if I recall correctly, that was after my competition. I did compete for CrossFit. And, you know, it’s hard, after for a couple of hours. It takes a toll on your body. So I was kind of stretching my hip and stretching, you know, the rest of my glute area to avoid that flare up again. That’s something that once you experience it once and you have to go through the treatment, it stays in the back of your head because you certainly don’t experience pain again. That’s why you have to pay attention to all the different preventive areas and approaches to avoid ever having a flare-up.
Dr. Alex Jimenez DC*: Well, I got to tell you that I led you there because I know you had a lot of experience with sciatica. Alex, let me ask you this. You know, you were an aggressive competitor in the world that you did things. Tell me a bit of the thing that you did that you noticed when you were working. Let’s say an as a collegiate athlete, did you ever have hip issues?
Alexander Isaiah: Only when I didn’t stretch or when I didn’t work on my core muscles, or when I wasn’t making sure that I was anatomically in line, I did have some issues either with joint pain or just lower back problems or even upper back problems that all just tied into either flexibility or I just wasn’t paying attention to either my diet as strictly as I should, especially at that level. So, yes, I did.
Dr. Alex Jimenez DC*: Yeah. You know what? There’s a lot to be covered here, and we’re going to be discussing a lot of issues. Did anyone want to add something else before we kind of closeout? I want to thank my crew for what we’ve done here. We are going to continue with this. Because we’re going to go real deep, this story of sciatica is going to get nasty with information. This is the beginning of touching on the subject matter. Thank you, Alex, for bringing the information because extremely, very deep in terms. I want to thank Astrid for giving us insights into biochemistry. My true patient, Trudy, and my coach over here, Kenna, and the supporting staff. So I want also to go if you guys want to find us. We’re here, and we’re here in this area where we are available. If we can help you and you can contact us at any given time. I want to thank you all, and I appreciate it. We’re going to be hitting sciatica relentlessly because it was relentlessly the scourge. It is ripping apart a lot of people at their works. They just quietly suffer. They don’t sleep, they stress out, and it causes a disruption. And it happens in mommy’s world, and it disrupts the whole family directly because a happy mommy is a happy family. So the entire thing is what we want to do is to assess what’s going on here. Find out the treatment protocols and give you the best options possible. Thank you guys very much, and God bless.