Introduction
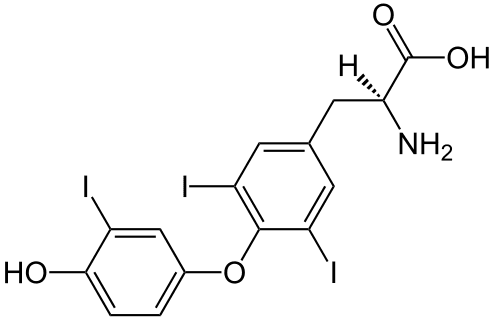
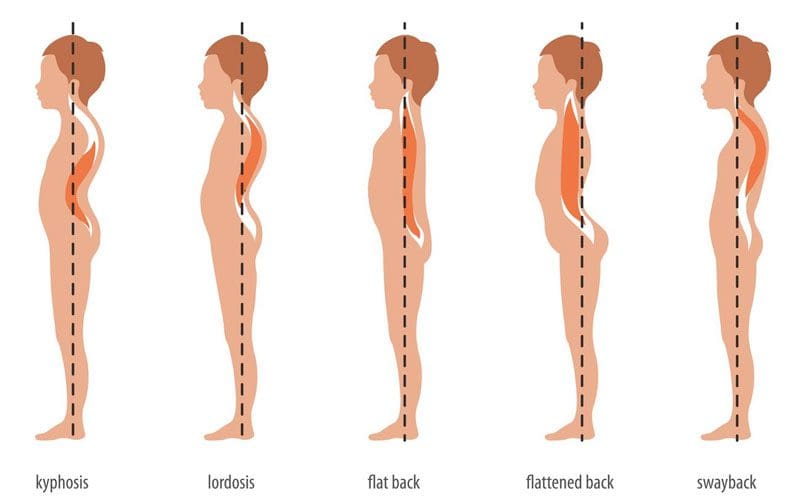
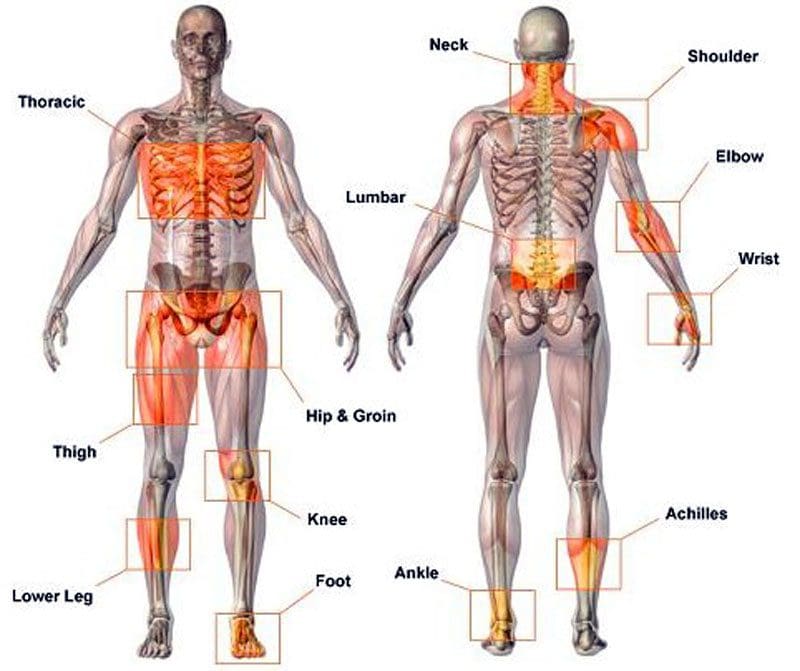
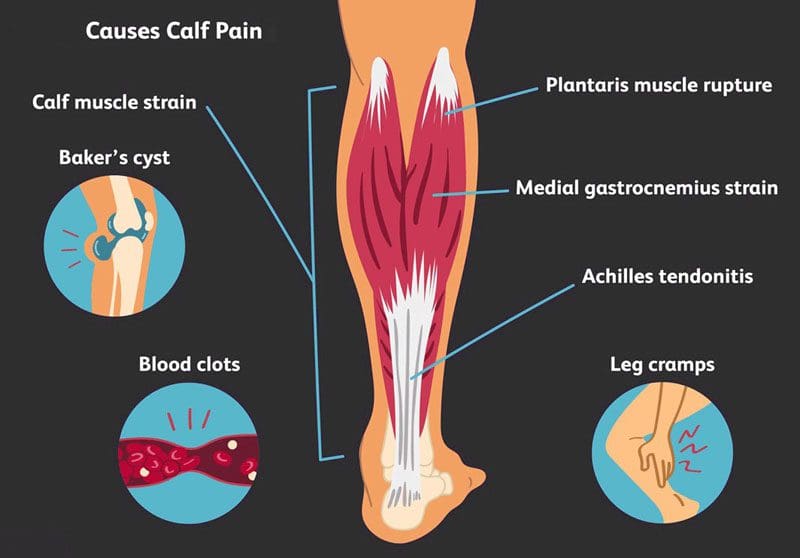
In today’s podcast, Dr. Alex Jimenez, Senior Health Coach Kenna Lee Vaughn, and Master Nutritionist Ana Paola Rodriguez Arciniega discuss inflammation and immunity. Inflammation can be both beneficial and harmful to the body especially in the immune system. When a person is injured, inflammation can help the body to heal the affected area. However chronic inflammation in the body can cause many problems that can cause bodily harm and many individuals have residual pain in the affected areas. When inflammation affects the immune system, it can cause chronic diseases like leaky gut.
Can my insurance cover it? Yes. In case you are uncertain, this link has the list of all the insurance providers that we cover.
What Is Inflammation?
Dr. Alex Jimenez and his crew discuss what is inflammation and the cause of it. Inflammation can become chronic if it is not taken care of and can actually leak into the organ systems in the body.
[02:11:47] Dr. Alex Jimenez DC*: Guys, we’re presenting a dynamic speaking specifically about inflammation today. Inflammation is the topic of what we’re going to be discussing as functional medicine specialists. What we do and we evaluate whether you’re an internist, whether you’re a physical medicine doctor, whether you’re a chiropractor or a physical therapist, an endocrinologists part of treating. We try to correlate medicine and bring what’s best inappropriate for a patient. We do our due diligence in assessing precisely the best approach for a patient. Now, the term functional medicine is a new term relative. For the last decade or so, it’s a practice that assesses the entire body to evaluate the correlations and the kind of associations that are indicative of things that can affect many organ systems, such as how inflammation in today’s particular topic matter affects the heart, how inflammation affects the brain, how inflammation affects the gut, how inflammation affects different components of the body. We’re going to hear terms that we’re going to listen to dynamics, and we’re going to hear present changes in modern medicine and words that are being used, such as leaky brain, leaky gut. They don’t sound like they have a clinical basis, but today modern medicine embraces the concept of correlated messages in personalized medicine. What’s good for Billy is not suitable for Billy’s sister sometimes, and even though they may have the same cold, there are reasons for us to adapt their approaches. So what we do in physical medicine is to correlate the issues of treating people specifically for pain disorders. We have chronic pain; we have acute pain when dealing with functional medicine. We’re working with the dynamics that assess where the inflammation comes out and the genesis of inflammatory processes. Today’s particular topic that we’re going to be discussing is inflammation at its basis because it is the most critical component of chronic, acute inflammation. It’s the part of repair and recovery. So today, we have a presentation we have Ana Paola Rodriguez Arciniega and Kenna Lee Vaughn. Ana is our master nutritionist, and Kenna Lee Vaughn is a supreme senior health coach. I call it. And what we do is we’re going to be discussing inflammation as it pertains to just a fundamental ideology and an understanding of what it is. So from there, we’re going to be able to do that; we’re going to see that these issues affect the brain and inflammatory repair. They do different components, so they affect the gut, too. They affect the heart; they affect the intestines. All various components of the body have inflammatory processes based on inflammation in our immune system. So what we’re going to be discussing today is how inflammation affects different organ systems. So I’m going to go back and forth between Kenna and Ana right now; what I’m going to do is I’m going to have Kenna go ahead and kind of take over the screen so we can start discussing the issues. She can begin discussing how we approach inflammation in our particular practice in physical medicine and in the ideas of pain management and how it connects to different organ systems, right? Because we got to pay attention to the body the way it is. So here we have a presentation, and Kenna, tell us a bit of where we’re going to take inflammation and immunity.
Tests for Inflammation
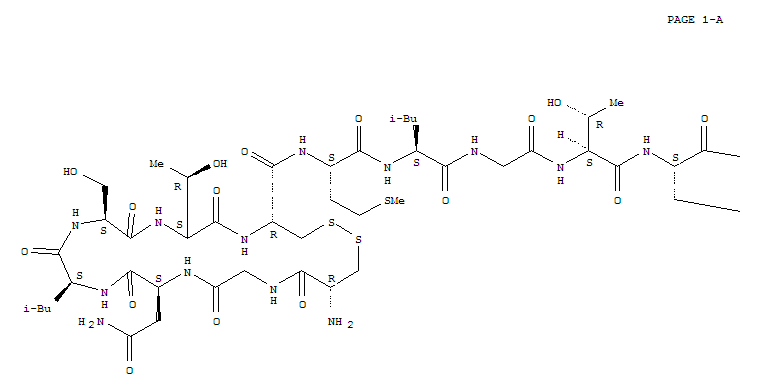
Senior Health Coach Kenna Vaughn, explains how certain tests like Living Matrix can help assess individuals that are dealing with inflammation in their bodies. She goes into detail that the tests can help a person find out what is causing them pain.
[02:15:56] Kenna Vaughn: Yes, so one thing that we do when our patients come into the clinic is we always want to assess inflammation because it does, like Dr. Jimenez saying, have so much to do with every other body system that’s going on. So one thing we do is called the Living Matrix, and this is a detailed assessment that takes us into your history and your story and helps us put a little bit of a number onto this inflammation and see precisely where we’re going. So if we go ahead and look at part of our Living Matrix, what we get is right here; we can see that it’s divided into different categories. This patient right here has a significant response to defense and repair, meaning that this is where we’re going to want to focus a lot of our attention on at first to try and go in there and see how this inflammation is impacting their immune response, how it can decrease the inflammation, help rebuild a healthy gut so that these inflammatory responses aren’t constantly firing off and get their immune response back down to a healthy level. We want our Matrix to look more uniform. We don’t want it to be all over the place. So once we start with our initial assessment and break down this defensive repair, we can focus our attention on these other areas that the patient may need help with. Another great tool that we have is lab testing that we use, and I have a sample I’m going to go ahead and pull onto the screen right here. This is from Vibrant America, one of the companies that we use. This is their gut zoomer. One thing that I love about their gut zoomer is you can see right here, not only is it just assessing their intestinal permeability and how that has to do with inflammation.
[02:17:50] Dr. Alex Jimenez DC*: Kenna, can you just hit the plus mark on there so we can see a little bit better? It’s a little bit too small, just a little plus mark on the percent sign. Yes. A little bit more. There you go. Now we can read it, thank you. Good.
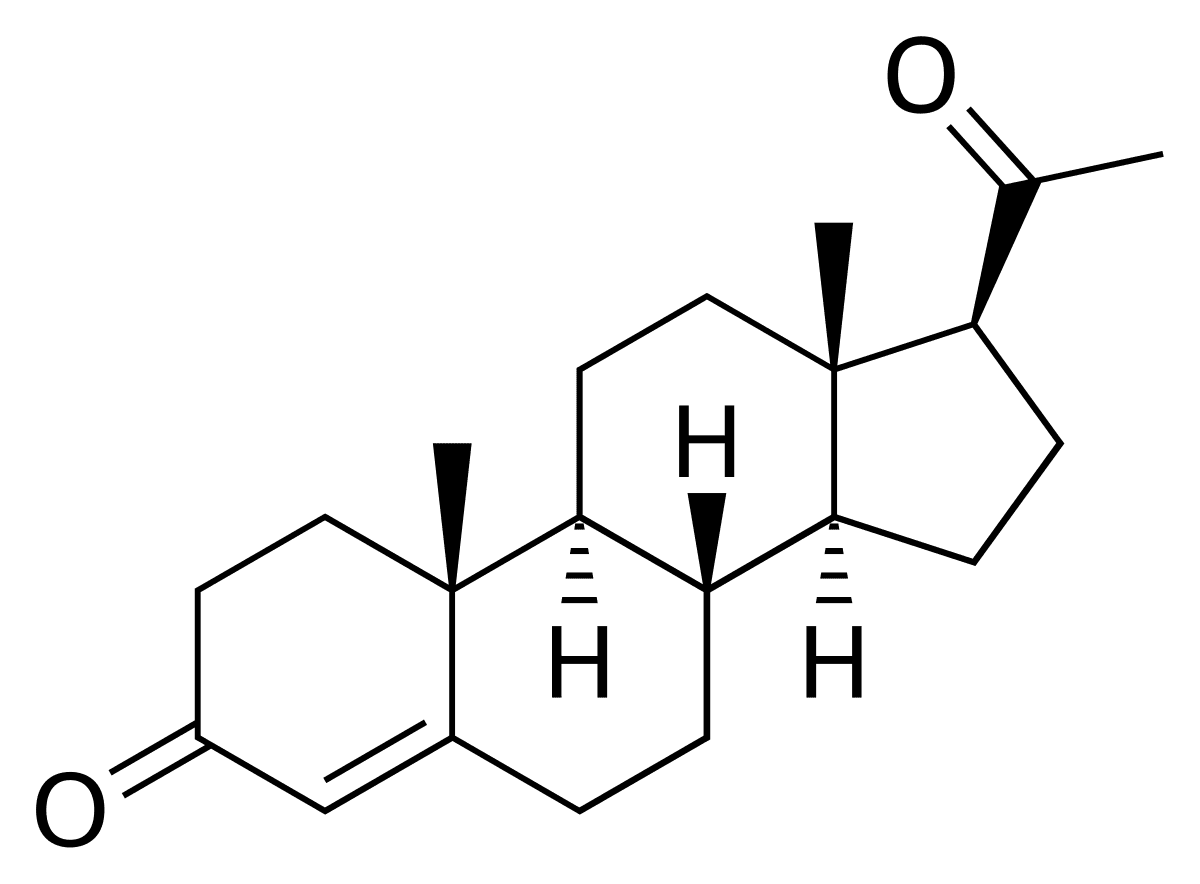
[02:18:01] Kenna Vaughn: Perfect. So one thing that I like is not only are we looking at the intestinal permeability, but we’re also seeing how their intestinal permeability is impacting their cardiovascular health, metabolic health, neurological health, hormone levels, TIBO, autoimmune health nutrition. We can use this test as a great snapshot and the Matrix on where to focus first to tame that inflammation and help our patients feel better quicker because this takes out a lot of guesswork. Of course, every patient is different, and we do use more tests than just this. But this one, in particular, is excellent when considering inflammation and our gut health and using it alongside that Matrix and how they coincide with each other.
[02:18:49] Dr. Alex Jimenez DC*: Kenna, is this the best test, or is this only one of the tests we use? I can answer that.
[02:18:56] Kenna Vaughn: This is only one of the tests that we use. It depends on what will be the best course of treatment for them and the protocols we take. But this one really does offer an excellent overview of everything that’s going on inside that gut and gives us a great baseline to even start with for later on that we can test our patient again, and we can track right here. We can track how their levels go up and down to ensure that protocol is working.
The Immune System
Dr. Alex Jimenez discusses how many factors can affect the immune system. Many chronic pathogens can cause not only inflammation to the body’s systems but can develop chronic pain that can make a person miserable.
[02:19:25] Dr. Alex Jimenez DC*: What I like to mention is that what we look at is whether you’ll see the word gut commensal means. The thing is that the bugs that we have. So, in essence, as we look at those particular dynamics, we see what’s going on. Can you minimize that specific screen on the report and bring it down and so I can go back to the Matrix there behind it? The Matrix behind it is one of those areas that can teach us that an individual doesn’t just have one area that is having a problem in most situations. You’ll see that people have energy issues, biotransformation issues, and they also have vascular issues, neuroendocrine issues, a structural integrity issues. And we’re going to be discussing even assimilation issues. What we try to do is begin in a direction. So with functional medicine, we can assess to a detailed questionnaire where the problem is not just inflammation, but where the disorders seem to be creating the most significant kind of like impact for the individual. Based on this detailed history, which is pretty profoundly deep, we can assess where we want to begin as a starting point. Otherwise, I would get from our patients that nutritional advice is confusing. As it’s confusing, it just wraps you around, so many times thought processes from different doctors that you become tied up within a spin of cobwebs of also an enigma wrapped around some chaos, at which point, you find yourself lost. This is a problem affecting most doctors dealing with the type of practice. So what we try to do is bring order and clarity in the direction we’re taking. Based on this, today’s particular discussion is about the immune system. So once we figure out that there is an immune system, I know Ana will be able to take over the screen right now. And as she does, what we’re going to be able to see is that in the dynamics of what Anna presents, she’s a nutritionist, a massive nutritionist, and an educator as well. She teaches, and she’s taught at different places. She will bring us some insights into immunity and the direction of this particular commentary. So do you have access to the screen share Ana?
[02:21:57] Ana Paola: Yes.
[02:21:58] Go ahead and pop your screen up. And then what we’ll do is we’ll take it from there, and we can look at it. Now, I know you had mentioned something regarding the immunity and the direction. We want to discuss this. Go ahead and tell us in your direction.
[02:22:11] Ana Paola: Well, everything has to come together as you said before. So eventually, what we’re going to start seeing is that inflammation has a direct response to immunity. And sometimes people come over to us, and they say, like, Oh man, I think I have a food allergy, or I keep having like this infectious disease. I don’t know where it’s coming in. Once I get that flare-up of infection disease, I get inflamed, and I get bloated. It seems like my life is coming like it’s like falling apart, so sometimes you have to go along; well, not sometimes, but all of the time, you have to look at the antecedents, look at the triggers, look at the mediators are the ones that are like the leading players. These primary factors are inducing this particular condition. And try to link them together and most of the time. And while not most of the time, inflammation will be a big part of it because it’s like the main trigger of everything we might have the gun, but inflammation is always the trigger. So it’s just like the same thing with immunity. It’s just that we have to look at the symptoms whenever a patient comes over and you see that they are having some allergic reaction, or maybe she has a rash, or perhaps he’s having bloating problems. OK, go directly to the cup because right there is where we’re going to find the answer. So yes, maybe we can make that connection right now. Why is inflammation, or why is there meaning-provoking food or the leading cause of this inflammatory response? Or are these in units your response that I’m having? But you will see after this quick explanation of why it’s going on.
[02:24:20] D. Alex Jimenez DC*: Let me kind of interject there. One of the aspects that Ana mentioned was discussing antecedents, triggers, and mediators to clarify the antecedents. Antecedents are things that are predisposing factors. These are things that your genetic, your environment, it could be things that constantly are in your life. They’re the things that maybe you live in an area where there’s high electric, high toxins; these are your antecedents, your environment also antecedents, it’s a lot to do with your genetics. So when you look at someone’s genetics, these are the predisposing factors. You know, the number one thing that determines your fate in life is genetics. I have black hair. I have a particular type. Those are the things that define my genetics. So whether we have that, we see that our genetic predisposition significantly influences us. What we’re learning in modern medicine is that your genetics are what we use it as an example of a like a gun versus a gun is the thing that you can have in your house that your genetics; OK, whether you choose to trigger it and fire it, it’s up to you, OK? And in many situations, we can mitigate and work the triggering factors. So when she mentioned seeing at the antecedents, triggering the trigger activates those and the anteceding environments. Now sometimes, what we have is have mediators. These are things like stress. We are learning that these are things that continue the problem. Items of constant foods. These are specific allergens and certain things that cause inflammation. These are the mediator that kind of this keep it going. It’s like when you start a balloon and start it, that’s the trigger. It goes up. But everybody keeps the balloon up, keeping it going to the party. Those are the mediators. So we need to figure out what those mediator components are. So I just wanted to explain precisely what antecedents, triggers, and mediators work. Go ahead, Ana.
Our Body’s Immune System
Master Nutritionist Ana Paola explains how our body’s own immune system has many defenses that can help protect the body from inflammation. She discusses how certain pathogen factors can affect the immune system, whether it is a food allergy, obesity, or chronic gut problems.
[02:26:24] Ana Paola: Yeah. So that’s right. And sometimes we ask the patient, OK, did you have or do you have any sibling who has previously reported allergic reactions to food? Well, that would be like an antecedent that you might want to look at or maybe, hey, what was that type of weird thing that you were put into the world or something like that? That would be a very powerful antecedent. And is your birth, your birthweight? And another thing could be breastfeeding. We need to know that someone could be linked to this problem, specifically if we’re talking about immunity and nutrition and allergies and food sensitivities. Well, let’s digress a little bit, and we’re going to talk about what is precisely what makes a healthy immunity. So we have like this fun wordplay right here that it’s dirt. So what will be like the main parts or the primary protectors of immunity is what it’s going to be like, that protective effect of immunity. Well, it has to detect and defend every kind of stranger pathogen or not like a stranger pathogen, just like a stranger microbe that we when we might be having in our system, OK? There is like this funny microbe-looking guy. It’s right there, but I’m going to keep it right there. I’m just going to keep it at bay, OK? It is detecting the microbe, and that’s like the thing it’s doing right there. The other thing that I help with the immunity might be able to do is that it has to be internally regulated. Once it fights this funky-looking microbe, it’s going to be capable of cleaning up the mess. So this is how I understand it. I always try to think about it like this, as if it was a story. So, yeah, internally regulate it. They might want to clean up the mess they made while fighting against this microbe. Another thing is that it is restorative. It has to come back after a fight. So yes, that’s like the art of this wordplay that we have around here and tolerance. It has to be able to tolerate that. There’s like this funny-looking pathogen or microbe, but since it’s not doing anything, I’m not going to attack it because if I attack it, I might do some cellular debris that will cause a more reactive action right there. And I don’t want to do that. So I’m going to tolerate that microbe that it’s right there, and I’m just going to let it be. So that’s essential. What the immunity has to do is be very diligent. It has to be. It has to be able to work whenever it is activated, and it has to be able to know what it’s going to do. I’d like not to react if it’s like a problematic microbe that we might have in our organism. So as I said before, the immune system should be able to identify any life-threatening structures that might be getting inside our system. Something fundamental is that it has to recognize stranger signals, but it doesn’t mean that it has to be all reactive all the time. Like, OK, I get it. It just went inside of the body, but it’s OK. I just detected it right. Right? We’re going to live with it. And the other thing is that it has to be prepared to respond to the threat appropriately when this dangerous presence. So if it’s not like a very life-threatening situation that the immune system might want to like, keep it as the down-low right there. So that’s like the deep part of that dirt.
[02:31:06] Dr. Alex Jimenez DC*: Ana, can you go back to the first part of that I was looking at, which was the right before that one? That’s screen right there. Detect, it’s a tremendous little kind of like a good wordplay, as you call it, the detect defense. We have had situations when we try to be a little bit smarter than the immune system, and the immune system has to be pretty much all these areas. It has to do, as you indicated, detect and defend. You know what I was given an example of for those who have cats; their cats are always kind of like they’re just sitting there quiet. But if something moves in miniature, they attack their centuries. OK, that’s the part of the immune, the what they call the innate immune system that it kind of sits waiting looking around, just evaluating looking things and making sure that it can do something. It’s ready to pounce on things. If it goes too crazy and becomes more than internally regulated, it may go internal, deregulated. In other words, it goes crazy. And for that, we have disorders where the immune system does not regulate itself and keeps ongoing, and it doesn’t stop. You know, we have caused chronic pain syndromes to autoimmune disorders. We end up seeing them in the office where the internal regulation systems are gone and continuously array. Restorative; it has to be repaired. It is the first guys on; it’s almost like when you have an electrical fire in your office, you know, and then you’ve got these electricians to show up right away. They’re the first to come in. We got to fix things up. We got to scrub it up. We’re going to make it work. So it has to be restorative. It has to be tolerant because it has to know, as you indicated, from what I’m gathering here, that it’s going to be OK with certain things, lets things pass, and certain things don’t. So let me give you an example of one where it’s internally regulated and restorative. Many years ago, we had certain medications that were Cox two inhibitors. Cox two inhibitors are inflammatory, and we don’t have to go through the names of those medications. But we learned that those medications worked so well on preventing the immune system from functioning that the actual restorative component of the immune system was blocked. Well, what happens is your body decays, and one of the symptoms is cracking of the skin and skin issues, skin repair problems as a result of trying to kind of pigeonholed the immune system. So we must be able to to to understand what the immune system is and how it affects the various organ systems. I know Ana and Kenna were discussing how it relates to different components. And what we need to see is we need to see how we can, as physicians assess where we can assist the immune system and help regulate it. Now I know you’re going to go over some different things; go ahead and continue with that.
[02:33:58] Ana Paola: Well, I think well, thank you so much. I think we already talked about being internally regulated. As you said before, it has to be very tightly controlled, not overreact over a single little thing. So it has to keep its cool down. So yeah, it’s going to be like a cool guy. Like, no drama in my house is that I know I know what is going on. I have it all under control. I will keep it tightly controlled, and that it’s me, that immune system. He’s like a cool guy. So whenever it’s like control, so restorative, it’s going to be able to repair the damage. So most of the time, when the immune system responds, it’s going to cost like some cellular debris because most of the time, the pathogens get disintegrated. And that same degranulation might cost like a very inflammatory reaction, or these particular tiny particles might get inside our gut system or our lymphoid system. Eventually, the response will be bigger if it goes that way. So as I said before, the immune system has to make sure that it cleans up its own mess. So it’s like a very cool guy, and it’s like a very clean guy. Now there we’re talking about what immunity has to do. It has to be very nice.
[02:35:51] Dr. Alex Jimenez DC*: Go ahead. Continue.
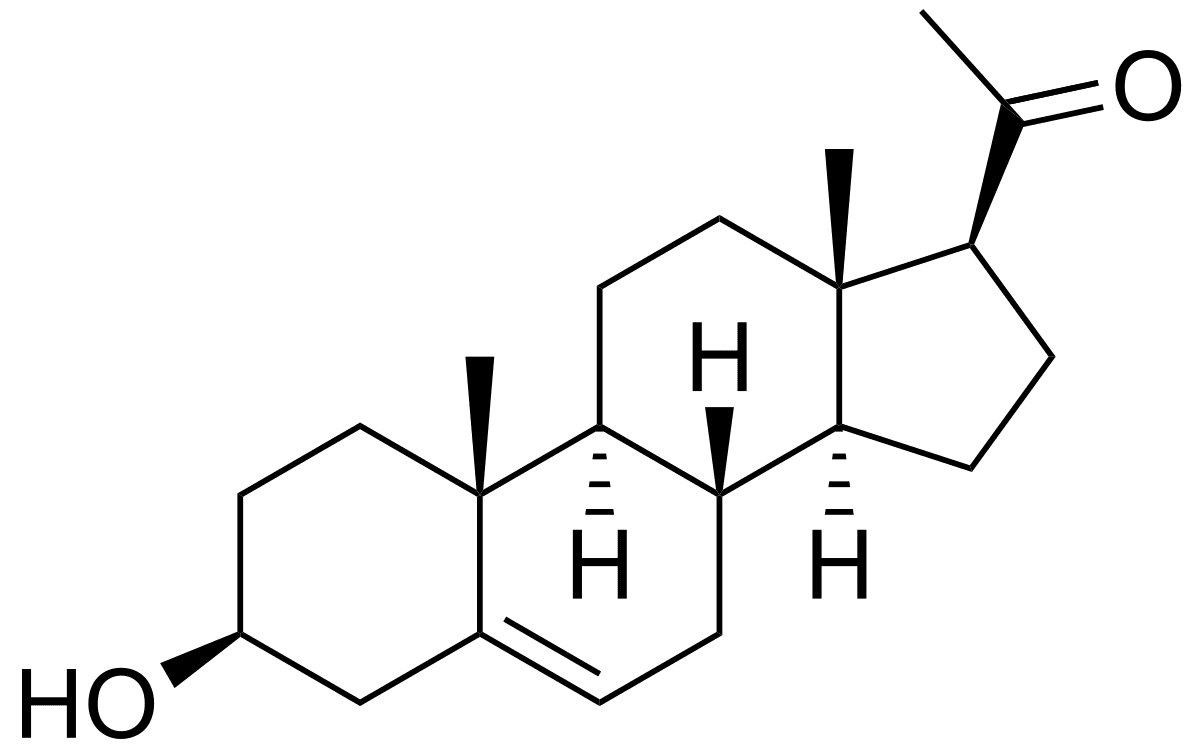
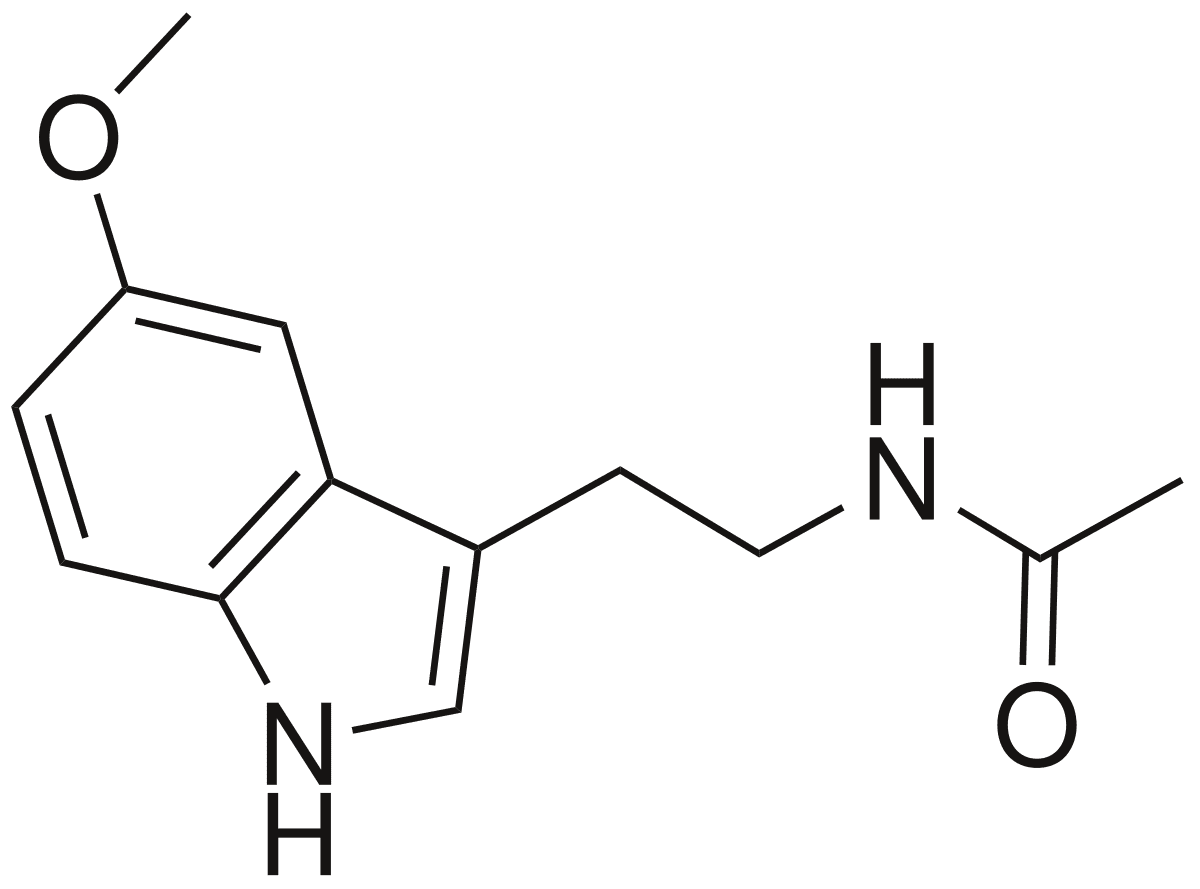
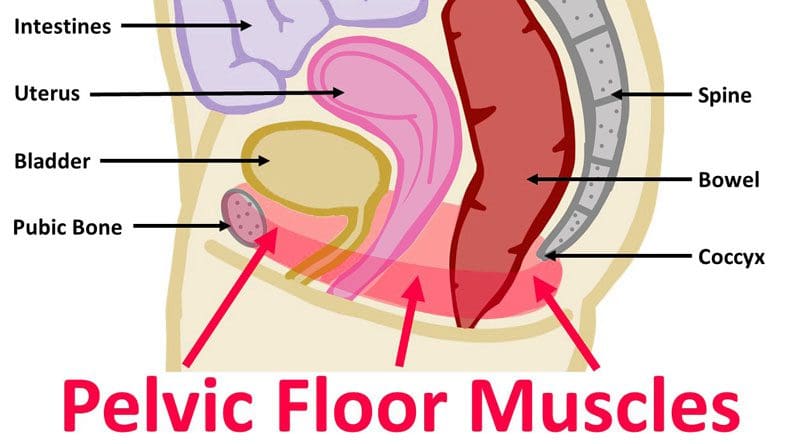
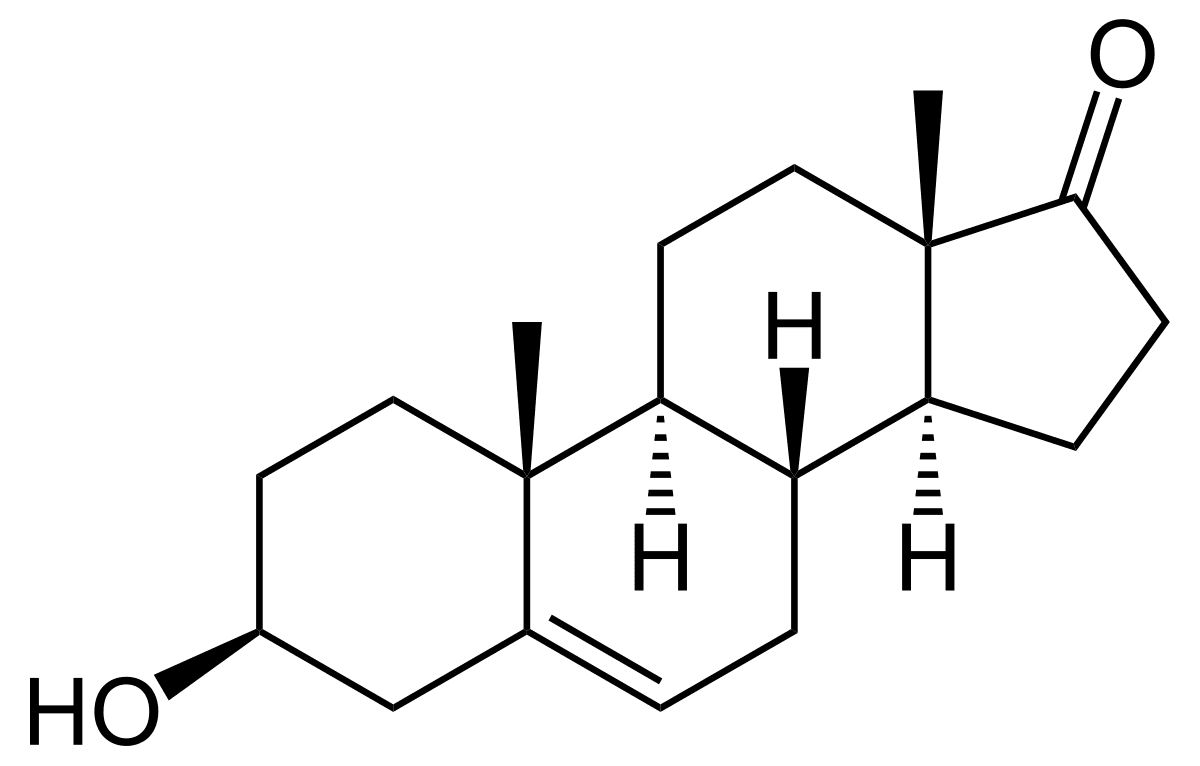
[02:35:55] Ana Paola: And it has to be tolerated, as you said before. I mean, there are going to be like good guys and bad guys, and he has to recognize that most of the guys going inside our system are not bad guys. They are microbes that might colonize our bodies, and they are perfect for us. Then he might want to tolerate them inside of our gut. And I think that leads precisely to the part of the immunity where our defense against pathogens or the barriers that come with the immune system plays a crucial role right here. So I think that the bodies are so exciting and intelligent that they gave it like a special place for all of the ring points system and all of the barriers to be precisely where they want to be for them to protect us from any pathogen that’s going to be roaming around our house, around our food, or to like a pathogen laying around there. So yeah, what is like the guys who keep the pathogens at bay? Well, it’s going to be the physical barriers; as I said before, it will be this skin. The skin is one of the most critical parts of that, of the knowledge of the immune system right here. The mucus and the saliva. So I would like to link them together and say that mucosal barriers are the most important things, and one thing about the mucosal is that it’s going to be the place where our microbiome will be present. So I would like to make that association right there. Then, of course, all that goes to the mucosal system, the skin, and the saliva. It’s going to be filled with microbes. They could be either good microbes or harmful microbes. And that’s precisely where the testing and the Living Matrix and all of the tests, don’t guess part of the functional medicine approach. It’s going to be like a significant factor right there because we don’t want to get rid of every single tiny microbe in our system or our gut, or our mouth. They need to stay there for protection to be better, so let’s put it that way. Another thing they’re saying is that celiac, for example, could be found in our nose, and it can brush out like a pathogen, so it’s set up our nose knows no stress. That’s acidic PH. So this is very important, especially when we’re talking about the gault. I recently had this patient that came to me, and she was like, having like this like bloating problem, and she didn’t know why. And I started asking for like, OK, tell me a little bit more about your medication history. And she said to me that she had been on anti-reflux medication for around five to seven years, but she wasn’t sure about it. So, man, she was suffering from a very extreme SIBO just because she wasn’t producing enough or sufficient gastric acid for the food to be ready to be digested enough, so then she was like having a bad reaction. So yeah. PH, gastric acid, and that acid environment that has to be inside our upbringing say things like the small intestine are essential for our bacteria to be in symbiosis with, so that is very important.
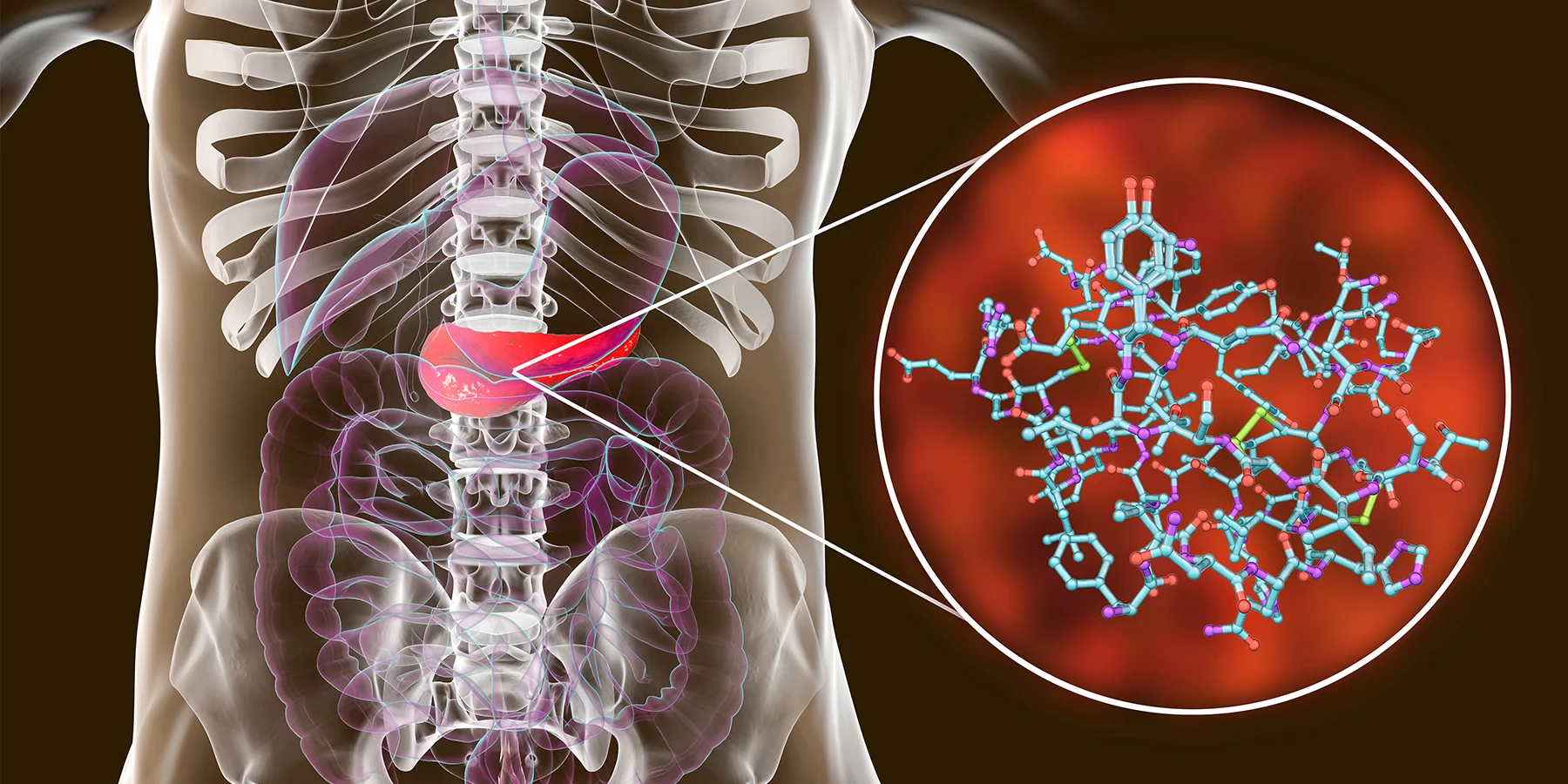
[02:40:20] Dr. Alex Jimenez DC*: Ana, you mentioned certain areas. When you were discussing things, you would go and take the screen for a second there. The idea behind the immune system, how God designs it is you see my screen there already. What you see here is that there are areas of the immune system and barrier systems. So the way God designed us is from when the first moment that an antigen or antibody or a reaction or reactants or, let’s say, an antigen enters the body, it is first met with your adenoid tissue. This is the nasal immune system. This over here ends up with your lower respiratory system, your brachial, or your bronchial immune system as it goes into your skin. It’s the salt system with skin. The gault is what she was indicating: the gut is in your immune system. The vault is vaginal areas, and your general is a region where this also protects you. So the designer intended for us to be protected and in many ways, and we can see those things. So when we look at this kind of dynamic, we can see that the body is well protected. However, what we’re going to be discussing are the inflammatory reactions as they occur in the body and how they affect the body. And we’re going to continue to do it in a future podcast as well. So what we want to do is Ana, you can take over the screen there or go ahead and run your program. I just wanted to make sure I get absolute clarity in terms of the types and the areas of where your skin, your intestines, your pulmonary system, not only your nasal area but even your genital areas affect your ability to protect yourself.
The Barrier Tissue
Master Nutritionist, Ana Paola discusses how the body’s enzymes are anti-microbial. She goes in-depth as well as she explains that the barrier tissue in the body can memorize where the infection is and can help the body to find it.
[02:42:10] Ana Paola: Yes, sure. Now, yes, that was very insightful. And of course, as you said before, the one who designed us knew precisely where it’s like extraordinary things for us to be protected. Another thing that I would like to mention is the protective enzymes that we have, like lysozyme in our tears. We know that they are like anti-microbial. And lysozymes could be found in maternal milk, and it’s like the most crucial enzyme after six months. It goes off after six months of breastfeeding, so it’s one of the most highly active enzymes that could protect the baby. So another thing that I like to mention, and I would like to associate this with, leaky gut and the permeability theme right here, is that the battered tissue has a memory that could help us find an infection better the next time made up here.
[02:43:31] Dr. Alex Jimenez DC*: What do you mean by memory? What does that mean? Memory does it? Does it remember? Talk to me about the memory component of the barrier system. This is new, and this is not something that was the recent studies reveal that those barriers have memory. So when it identifies, is this cross-react into or this antigen, there is an antibody reaction that you’re lining remembers. So it’s crazy. Go ahead.
[02:44:02] Ana Paola: Yes, they can recall that these tank-like pathogens that I’ve wanted to get through them or if that went through them the first time. And it’s safe to say that the barriers tissue up a function are or are part of the innate immunity right there. It’s like they know they are there to protect, but they will not make any specific information or any specific antigen to find a new pathogen. But they will fight or do something they are like the good guys. Immediately after every action is signed up for mature responses. We’re going to activate Band-Aid immunity that will internally to adaptive immunity or will like kind of make like this interaction. And it’s going to be for a more specialized reaction. And that same information is going to translate to the barrier and that it’s going to be the information that these good guys are going to get or are going to activate when they encounter by the same pathogen that they were before. So now they can fight it, they know how to react, how to fight it, and the infection or the information or the injury will be carried out a little bit faster this time.
[02:45:34] Dr. Alex Jimenez DC*: So, you know, when I’m going to take over and to give you a visual of the innate immune system, the natural immune system, what it does, it actually can identify the dynamics of whatever it is and bring it to an end. It’s incredible to see when we talk about neutrophils, specifically neutrophils, and macrophages, the ability to see exactly where that’s going. Let me see if I can do this. Can you guys see that screen right there? Yeah. So you can see how the uniqueness is of this particular macrophage. Here we have, you know, an element or, in this specific situation, it’s anthracis, Bacillus anthracis, and it’s a very deadly type of bacteria. You can see here, but do you see how the macrophage can jump on it and conform to its size? It identifies it, and it goes to destroy it. So this is an immune system. This is what I was talking about the sensory system. So you can actually kind of, you know, if you just think of it, it morphs into a design. So what we look at the immune response as it occurs now, Kenna do you have anything in terms of when you run a commentary on this particular component of it? So what we’ll do is, Ana, let me ask you this question in terms of this when we look at the immune structure as you’re going through your presentation. Tell me a bit about the physical barriers because this is new. What you have mentioned to me it is a unique component. We’ve always known that the T cells, the B cells from the humoral system, and the innate system have been able to identify things. But you’re telling me that the actual barrier itself is it remembers the barrier, the wall lining.
[02:47:35] Ana Paola: Yes, and as you said before, it’s like a very new light topic right here because we have to think about it as I like to think about all of our beneficial microbes get to weigh. They can leave them in enough symbiotically kind of way. That is the part of the microbiome and the barrier structure that very tight structure can provide better protection against pathogens. So that is like one of the things that. I want to talk like touch base, and that’s so yeah, that’s like practically one of the things, but as you said before, it is very new in terms.
[02:48:30] Dr. Alex Jimenez DC*: In terms of the inflammation, let me ask you this with your personal experience and what you have seen over the years. You know, what we look for is what affects our patients, right? So let me ask you in your clinical experience about your epithelia, your lymphoid tissue, and as you indicated, there are phases of inflammation. Tell us a bit of how your personal experiences with the immune system. How has it affected multiple organ systems?
[02:49:03] Ana Paola: Most experts would like to start with their gastrointestinal tract permeability. I think that it’s like the most important thing or like that. The something that I get concerned with the most and the thing that I notice is that in very old patients and the kind of work that I do there have been like enough and very important is that is there that we got from the permeability and the stability of the other tissues with very prolog, 968 contra hospital length of stay, so that is one of the things that I think affect the people the most and that more times they stay in the hospital is going to be like the worst. Like, they’re not going to have any improvement. They’re going to continue losing unless those skeletal mass, it’s going to be even harder to fight against infections once they start getting that metabolic and attritional state. So I think and know that that provision prebiotics and probiotics and this kind of patience will have a significant effect on them, and they’re going to get a better outcome out of it. So yes, that’s one of the first things that we have to put into that idea. The other thing that I know helps is that it’s one of my attrition and nutrition. One of the promoters of probing anti-inflammatory pathways might help reduce bad pro-inflammatory responses that very few patients have. And maybe I’m talking about critically ill patients, but this can function chronically ill patients. And I’m talking about cardio, metabolic distress, or I’m talking about allergic reactions. I’m talking about every type of chronic disease. So yes, in that particular set of things and immunonutrition, it will be like a big help out of bit. But it’s going to be nutritional foods that will have an anti-inflammatory effect. They are going to repair that tissue that will be distressed by all, by all of that diseases inside of the patient.
Conclusion
Dr. Alex Jimenez and his crew give a recap of today’s podcast on inflammation and how it affects not only the immune system but also the entire body system. Inflammation can cause many chronic issues in the body and can make it dysfunctional.
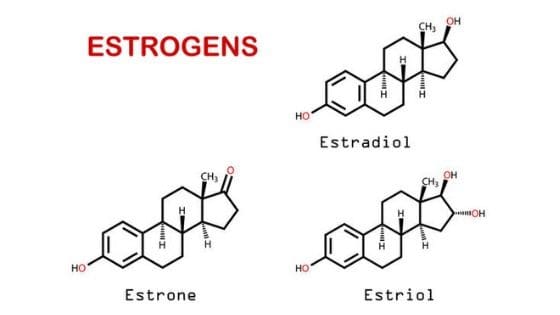
[02:52:03] Dr. Alex Jimenez DC*: What I like sharing here is that let me go ahead and share my screen here. And you can see that when I look at what goes on when I see a patient. And as we’ve been able to work with patients, it may start as an issue that it’s a back problem, a knee problem. It’s a chronic issue. And what we’ve seen is the inflammatory components don’t just stop there at the knees. We’re dealing with an individual, and we find out that I often deal with an individual who’s had multiple joint issues, maybe even replacements at an extreme or just chronic knee pain or chronic discomfort. We are trying to make the connection here that it relies upon the general state of the immune system and the inflammatory response. So as we look at the way the body responds, it’s, I think, essential to be as a clinician, as a group of people that are out here looking at to see what is the correlation to all of a sudden their brain fog, OK, because now we have a joint problem that a person is also having memory issues. They are sometimes taking, you know, proton pump inhibitors, such as for anti-acid production in the stomach, which now alters their biome, or what they call their gastric biome or the bacteria affecting the immune system directly. As you look over here again, as Kenna had put, this particular picture, you can see that it crosses the line. So we sometimes have to become like almost like scientists to figure out where this correlates, not just to say, OK, this is a joint problem and send him out to, let’s say, a joint specialist or it’s a memory problem, send them to a neurologist. We’re trying to put it together, and that’s what functional medicine works on. So what would Kenna be presenting there and if you want? I want to end today with the component going back to your vibrant study. Do you have that available there? So as you got that, and by the way, Kenna, we’re the only podcast in the world that has a six-month-old as one of our guests. So you can sometimes hear them there because we’re all-inclusive here, so we are ready, and my mommy took care of me. She could bring me all of the Motorola back in the day so people would look at me and say, Jadiah, Hey, I was with a little kid, and that was just a nightmare. So she had to bring me to work. Otherwise, the house was going to be torched. So tell us a bit of what was going on here in terms of the intestinal permeability. As we see this, we see that the gut or commensal bacteria are essential again to end with this vital component. It affects cardiometabolic. Cardiometabolic, the cardio system, the metabolic system, the irritable bowel system, the liver, the nutrition, the autoimmune. Is there something that you want to add to this?
[02:55:16] Kenna Vaughn: Yes, I was going to add on to the fact that since we’re talking about the immune system, a robust and healthy gut really will help you fight off so many more pathogens that you come in with when you have something like intestinal permeability and you are exposed to a pathogen. And if you have a leaky gut, that’s just another area that allows this pathogen to seep through back into their bloodstream. So we’re not going to be able to fight it as well. So, you know, we say here a lot from the kitchen to the genes, and one thing that we focus on in the kitchen is making sure our patients have a super-strong, healthy gut. So they can fight off everything. Well, not everything, but they can fight off more things that they come in contact with because we don’t want it leading to other areas of poor health. As you can see, it’s connected, as Dr. Jimenez said, that cardiovascular, metabolic, neurological, even your hormones, and there’s just so much that comes down to the gut and the environment and the foods we’re eating. And so, if we attack the gut and make sure that we’re building it up to be healthy, we will start to see our health improve in other aspects of our life, including inflammation, our immune systems, and things along that line.
[02:56:34] Dr. Alex Jimenez DC*: It’s incredible as we come that grows here, the magnitude of what the intestines have to do and correlate with all our bodies. Now it’s very logical. Our world experience comes through as a child from our mouths. So it would be very logical that when our God and our creator created the protective system, there was going to be a relationship with the outside world and the bacteria within our systems. So what we are aware of is where most chronic disease begins. The chronic disease starts at the mouth. And from dental hygiene to oral hygiene to intestinal balance, we need to start there. And at that point, it is impressive. Once we understand that this is a significantly correlated and associated issue, we can work towards a causative reason and find out where it is that it’s a being affecting the joints, brain fog, or cardiopulmonary reaction because we don’t want to end up in front of a doctor just because we didn’t pay attention. We got to know that we did do something to prepare our bodies. And today, I’m going to leave it there because we are all doing our thing, and we can try and make this a little shorter. But I want you to know that we will be presenting a deeper insight into inflammation and immunology because it is the basis of many chronic disorders. Now we just began with today, the innate system will end up in the humoral system, and we’ll be putting it together over time. And hopefully, we will add to it until the level of understanding that our population can have because I believe most people need to understand that. I want to know when you drive; you kind of look at the speedometer today, you got to know what your A1C is at. You got to understand your triglycerides. You’ve got to know what your LDL is. Your HDL is. Are you got to realize your lipid profile? We know how our metabolic system is today. You hear stories of ketones where we’re set, and we’re poised to be able to share with the public that technology has moved. We can measure, you know, as simple as how many walks you do, how many what you’re eating, what your diet is. And we can calculate a lot of things to determine how to keep your optimal health. So I want to thank you guys all. You can stop sharing that so we can all be on the same screen here; what we can all do is we can do ourselves a good service by connecting the dots. It’s essential to connect what you eat that may not affect your joints or your inflammatory or chronic disorder today. However, it may be doing it three to four or five days later where you don’t perceive it. You’ll notice that people who eat clean diets, their joints stop hurting their brain fog goes away. That’s why we have a quick fix, and it’s called the elimination diet that we instantly change the way someone’s metabolism is. It is working on what we call antioxidants, a reactive oxygen species resulting from lousy metabolism. So again, the immune system is at its core. So we’ll be discussing this much more elaborately. I want to thank you guys all, and I want to tell you that I appreciate you guys taking the time and being with us for the next one, and I look forward to the next time we can hook up. Maybe this weekend or so. You guys have a blessed day. Thank you, Kenna and Ana; I appreciate you guys.
[03:00:16] Ana Paola: Thank you.
Disclaimer