Table of Contents
Introduction
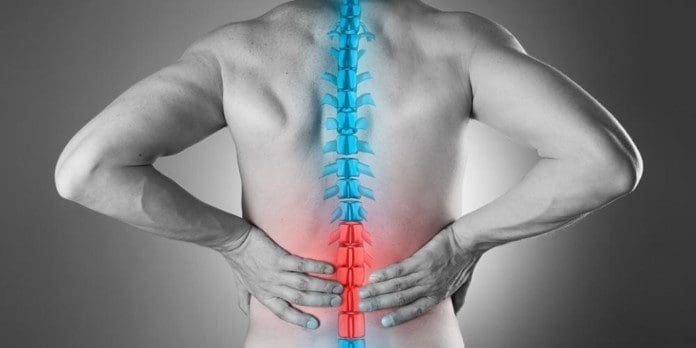
The spine is essential for maintaining our upright posture and allowing us to move without pain. The cervical, thoracic, and lumbar sections support different body areas. However, environmental factors and pathogens can cause musculoskeletal pain, leading to spine misalignment and stress on the surrounding muscles and nerve roots. Non-surgical treatments like IDD therapy can help realign the spine and relieve pain. We utilize and incorporate valuable information about our patients to certified medical providers using non-surgical treatments like IDD therapy to alleviate pain associated with musculoskeletal pain along the spine. We encourage and refer patients to associated medical providers based on their findings while supporting that education is a remarkable and fantastic way to ask our providers the essential questions at the patient’s acknowledgment. Dr. Alex Jimenez, D.C., comprises this information as an educational service. Disclaimer
The Pathological Effects Of Musculoskeletal Pain On The Spine
Are you experiencing muscle pain in various parts of your body? Do you feel stiffness in your back, neck, hips, or shoulders? Or are you experiencing localized pain in a specific area? These are common symptoms of musculoskeletal pain, which affects the spine. Unfortunately, research studies reveal that musculoskeletal pain is a leading cause of long-term suffering, disability, and decreased productivity. This type of pain can strain the surrounding muscles in the upper and lower body, affect joints, and cause overlapping risk factors that make diagnosis challenging. Research studies also suggest that musculoskeletal pain can arise from different structures, leading to local or central sensitization and correlating pain intensity and duration.
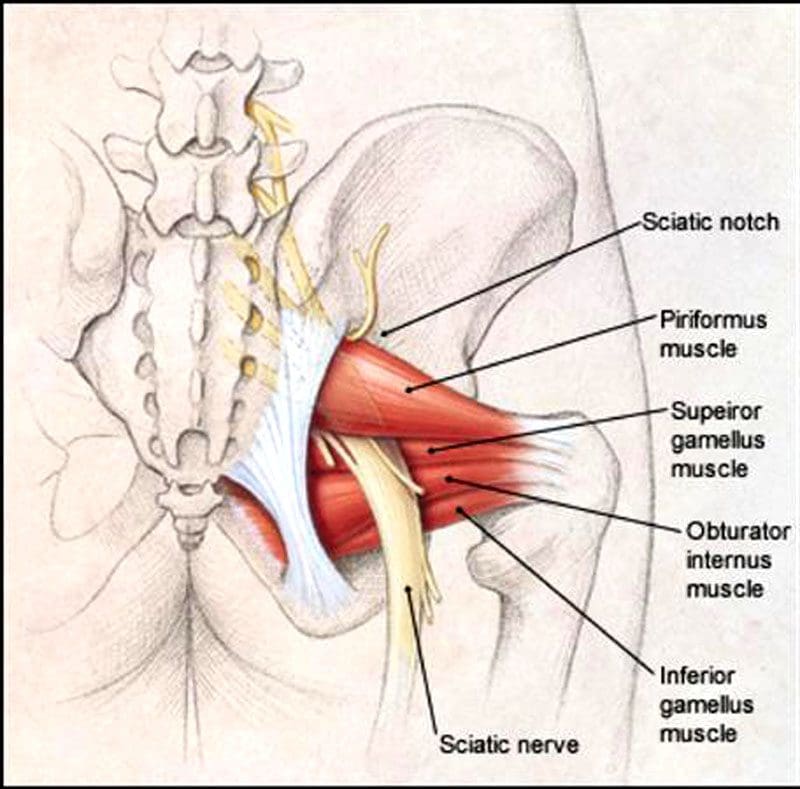
Did you know that musculoskeletal pain can have pathological effects on the spine? Research studies revealed that the musculoskeletal system significantly impacts the central nervous system regarding pain. This means that when pain occurs in a certain area, neuron signals are sent to the brain, increasing sensitivity markers to that location. In the case of a traumatic spinal cord injury, these signals can become chaotic, leading to additional risk factors for the muscles surrounding the spine. This can result in musculoskeletal pain, which may cause referred pain in other body parts. Additionally, research has indicated that severe pathologies associated with the central nervous system can also lead to musculoskeletal pain. This is because the brain’s neuron signals alert the immune system that something is wrong and needs immediate attention.
The Science Of Motion-Video

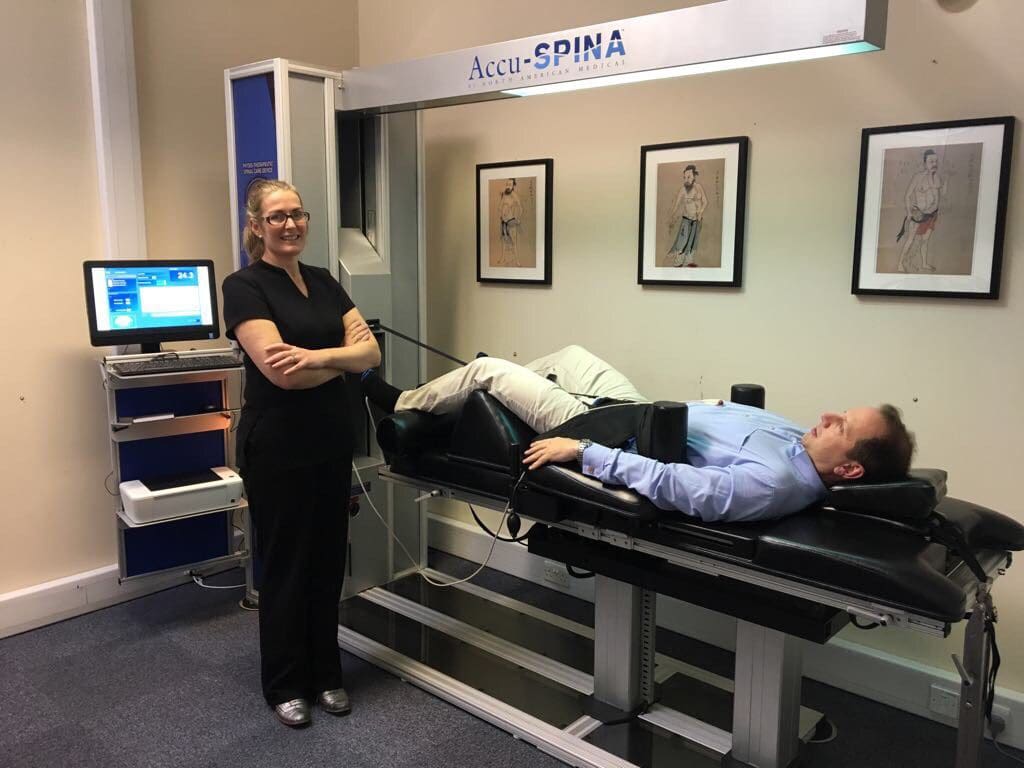
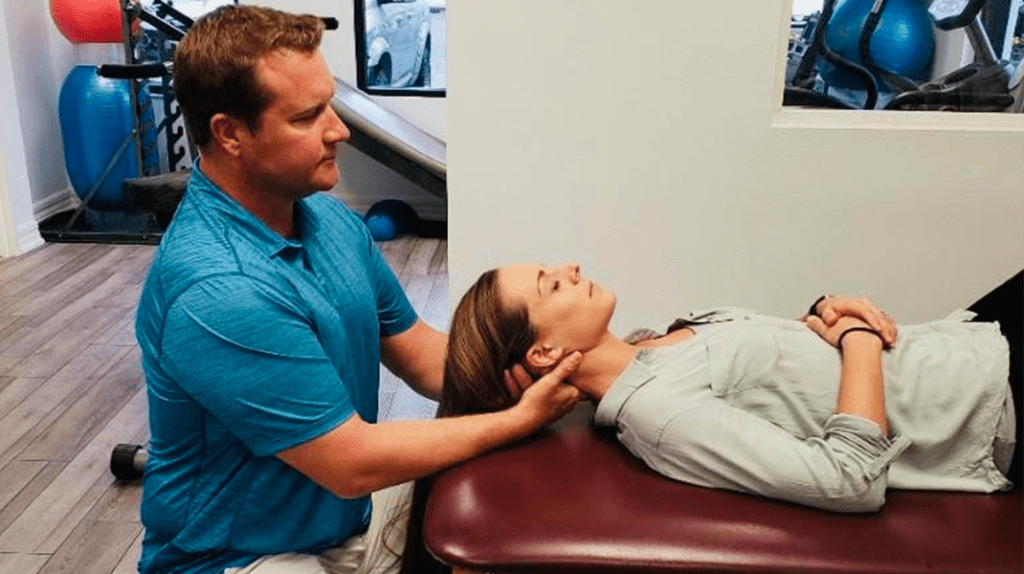
Have you been experiencing stiffness or pain in different parts of your body? Do you feel discomfort lifting heavy objects or feel a pinched nerve in your lower back or legs? These daily issues could be caused by musculoskeletal pain affecting your spinal cord. Traumatic or non-specific issues can lead to overlapping risk profiles and the development of musculoskeletal pain associated with the spine. If the spinal column is affected, it can cause neuron signals to become hypersensitive, resulting in a misalignment of the body. Fortunately, non-surgical treatments can help realign and heal the body naturally, reducing the effects on affected muscles while allowing necessary nutrients and blood to flow back to the spine. The video above explains how non-surgical treatments like chiropractic care can harness the body’s ability to heal and restore stability through manual manipulation. Chiropractic care can also be combined with decompression therapy to stretch and alleviate pressure off the spine gently.
What Is IDD Therapy?
The musculoskeletal system depends on nerves, bones, and muscles for body structure and function. When affected by unwanted pathogens, it can cause pain in various areas and make a person feel miserable. Fortunately, non-surgical treatments like IDD therapy or intervertebral differential dynamic therapy can help reduce musculoskeletal pain affecting the spine. IDD therapy is decompression therapy that can help reduce pain by mobilizing and lengthening compressed spinal discs with special treatment forces. In “The Ultimate Spinal Decompression,” Dr. Eric Kaplan, D.C., FIAMA, and Dr. Perry Bard, D.C., states IDD therapy effectively alleviates spinal pain associated with the musculoskeletal system. The book also mentions that this therapy helps free the spinal discs and nerve roots as the compressed pressure is dropped. To that point, it allows the oxygen-riched blood and nutrients back to the spinal discs to begin the healing process, as research studies revealed.
Conclusion
When the spine experiences traumatic forces or injuries, it can result in musculoskeletal pain that can be constant and miserable for the individual. However, no one should have to endure such pain. The spine supports the upper and lower sections of the body and needs to be mobile to perform this task. Non-surgical treatments, such as IDD therapy, can help alleviate unwanted pressure off the spinal discs and nerve roots that have become hyper-sensitive due to trauma or injury. This decompression therapy can help restore mobility to the spine and rehydrate the spinal discs to begin the healing process. With IDD therapy, individuals can relieve pain and experience freedom of movement.
References
Arendt-Nielsen, L., Fernández-de-Las-Peñas, C., & Graven-Nielsen, T. (2011). Basic aspects of musculoskeletal pain: from acute to chronic pain. The Journal of manual & manipulative therapy, 19(4), 186–193. https://doi.org/10.1179/106698111X13129729551903
Bang, A. A., Bhojraj, S. Y., & Bang, A. T. (2021). Back pain and musculoskeletal pain as public health problems: Rural communities await solution. Journal of global health, 11, 01007. https://doi.org/10.7189/jogh.11.01007
George, S. Z., & Bishop, M. D. (2018). Chronic Musculoskeletal Pain is a Nervous System Disorder… Now What?. Physical therapy, 98(4), 209–213. https://doi.org/10.1093/ptj/pzy002
Kaplan, E. & Bard, P. (2023). The Ultimate Spinal Decompression. JETLAUNCH.
Puntillo, F., Giglio, M., Paladini, A., Perchiazzi, G., Viswanath, O., Urits, I., Sabbà, C., Varrassi, G., & Brienza, N. (2021). Pathophysiology of musculoskeletal pain: a narrative review. Therapeutic advances in musculoskeletal disease, 13, 1759720X21995067. https://doi.org/10.1177/1759720X21995067
Schimmel, J. J., de Kleuver, M., Horsting, P. P., Spruit, M., Jacobs, W. C., & van Limbeek, J. (2009). No effect of traction in patients with low back pain: a single centre, single blind, randomized controlled trial of Intervertebral Differential Dynamics Therapy. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society, 18(12), 1843–1850. https://doi.org/10.1007/s00586-009-1044-3