Are treatments more successful when patients know key terms that describe their back pain and associated conditions?
Table of Contents
Nerve Pain Types
When individuals need to better understand their spine diagnosis, being able to distinguish between key terms can make a significant difference in understanding the development of a personalized treatment plan. Terms that describe back pain and various associated conditions can include:
- Sciatica
- Radiating and Referred pain
- Radiculopathy
- Radiculitis
- Neuropathy
- Neuritis
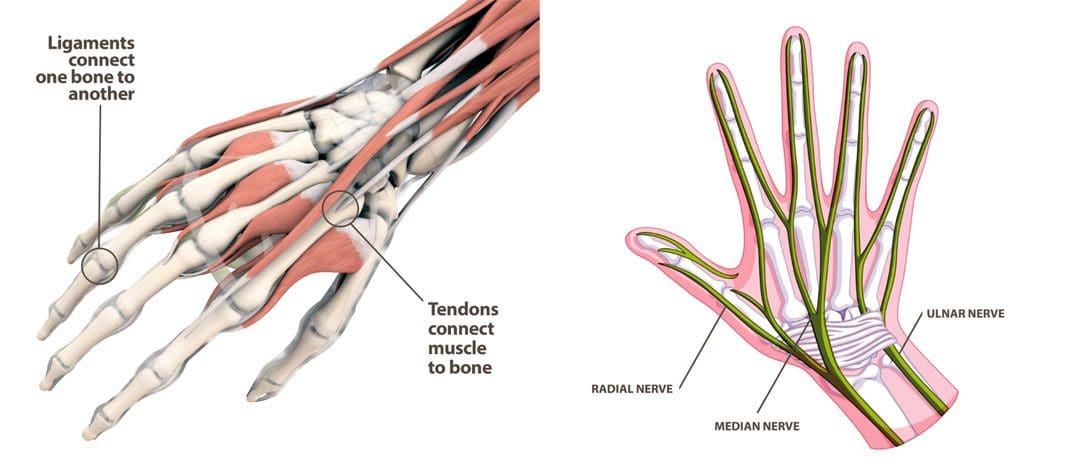
Causes of Back Pain
Back pain symptoms are most commonly caused by the continued practice of unhealthy/poor posture and overcompensated and weakened muscles. Even for individuals that exercise regularly, the movement choices that are made throughout the day can disrupt the way the muscles, tendons, ligaments, and fascia function to maintain proper body alignment.
- Injuries to, and conditions of, the structures of the spinal column like the bones, discs, and nerves, are generally more serious than posture problems and soft tissue-related pain.
- Depending on the diagnosis, structural problems can cause symptoms related to nerve compression, irritation, and/or inflammation. (Michigan Medicine, 2022)
Spine and Nervous System
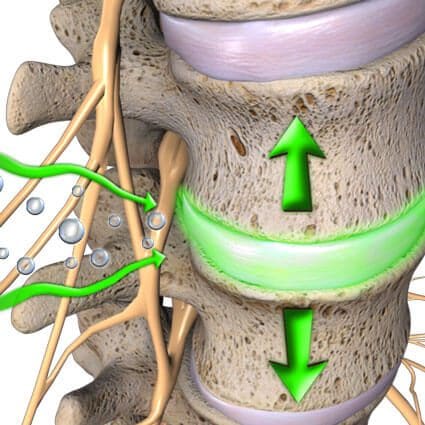
- The peripheral nerves extend out to the extremities with sensation and movement capabilities.
- Nerve roots exit the spinal canal which is part of the peripheral nervous system.
- The spinal nerve root then exits the spinal column through the foramen. (American Academy of Neurological Surgeons, 2023)
- The branching of nerves from the spinal cord and exit out of the foramina occurs at every level of the spine.
Terms
There are different medical terms when getting a spine diagnosis or going through the treatment process.
Radiculopathy
- Radiculopathy is an umbrella term, describing any disease process that affects a spinal nerve root and is something that’s happening to the body.
- When a healthcare provider informs you that your pain is due to radiculopathy, a number of more specific diagnoses, clinical signs, and symptoms may be included as part of the description.
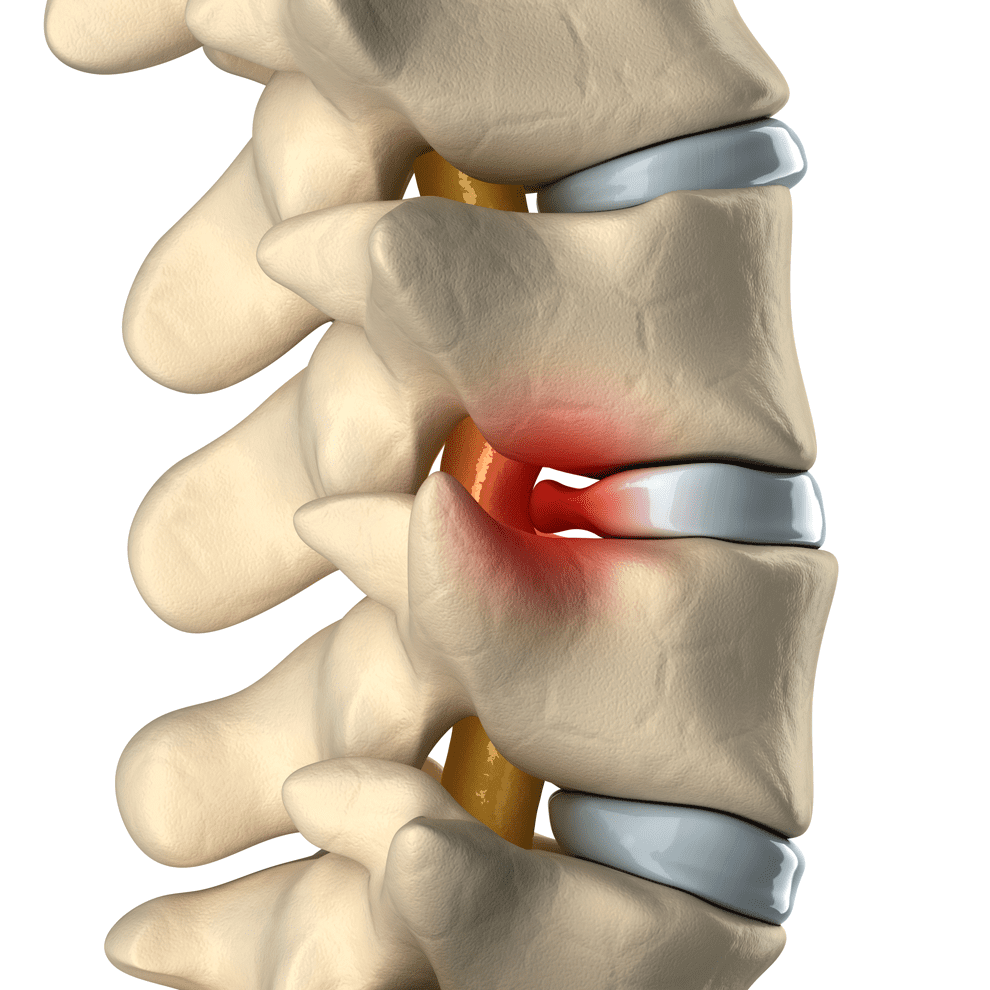
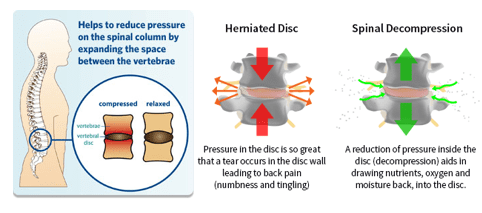
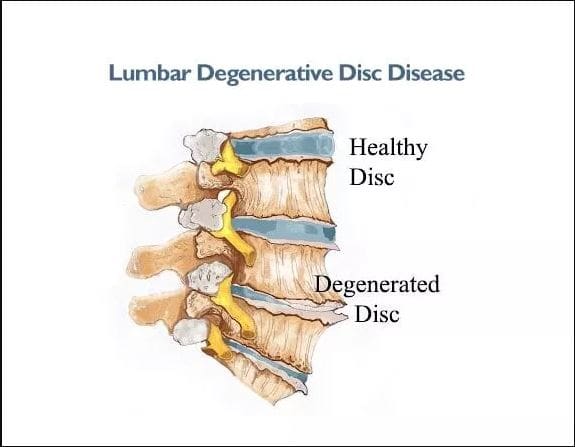
- Common causes of radiculopathy include herniated disc/s and spinal stenosis.
- Less common causes can include a synovial cyst or tumor that presses on the nerve root. (Johns Hopkins Medicine, 2023)
- Radiculopathy can occur in the neck, low back, or in the thoracic area.
- Often, radiculopathy is brought on by some form of compression of the nerve root.
- For example, extruded material from a herniated disc can land on a nerve root, causing pressure to build.
- This can cause symptoms associated with radiculopathy, including numbness, weakness, pain, or electrical sensations. (Johns Hopkins Medicine, 2023)
Even though there’s a spinal nerve root on either side of the spinal column, injury, trauma, or issues stemming from degeneration affect the nerves in an asymmetric fashion. Degenerative changes, known as normal wear and tear, typically occur in this fashion. Using the previous herniated disc example, the material that leaks from the disc structure tends to travel in one direction. When this is the case, the symptoms tend to be experienced on the side where the nerve root makes contact with the disc material, but not the other side. (American Association of Neurological Surgeons, 2023)
Radiculitis
- Radiculitis is a form of radiculopathy but it is about inflammation and not compression. (Johns Hopkins Medicine, 2023)
- Radicu– refers to the spinal nerve root.
- The suffix – itis refers to inflammation.
- The word refers to a spinal nerve root that is inflamed and/or irritated rather than compressed.
- In disc herniations, it is the gel substance that contains various chemicals that is inflammatory.
- When the gel substance makes contact with nerve roots, an inflammatory response is triggered. (Rothman SM, Winkelstein BA 2007)
Radiating or Referred Pain
- Radiating pain follows the path of one of the peripheral nerves that transmit sensory information like heat, cold, pins and needles, and pain.
- The most common cause of radiating pain is impingement/compression of a spinal nerve root. (American Academy of Orthopaedic Surgeons. OrthoInfo)
- Referred pain is experienced in a different area of the body that is away from the pain source which tends to be an organ. (Murray GM., 2009)
- It can be brought on by myofascial trigger points or visceral activity.
- An example of referred pain is symptoms in the jaw or arm when an individual is having a heart attack. (Murray GM., 2009)
Radicular
- The terms radicular pain and radiculopathy tend to get confused.
- Radicular pain is a symptom of radiculopathy.
- Radicular pain radiates from the spinal nerve root to either part or all the way down the limb/extremity.
- However, radicular pain does not represent the complete symptoms of radiculopathy.
- Radiculopathy symptoms also include numbness, weakness, or electrical sensations like pins and needles, burning, or shock that travels down the extremity. (Johns Hopkins Medicine, 2023)
Neuropathy
- Neuropathy is another umbrella term that refers to any dysfunction or disease that affects the nerves.
- It’s usually classified according to the cause, like diabetic neuropathy, or the location.
- Neuropathy can occur anywhere in the body – including the peripheral nerves, the autonomic nerves/organ nerves, or nerves that are located inside the skull and innervate the eyes, ears, nose, etc.
- An example of peripheral neuropathy is carpal tunnel syndrome. (American Academy of Orthopaedic Surgeons. OrthoInfo. 2023)
- One spinal condition that is known to cause peripheral neuropathy is spinal stenosis. (Bostelmann R, Zella S, Steiger HJ, et al., 2016)
- In this condition, changes in the foramina have a narrowing effect on the space that begins to compress the nerves as they exit.
- Neuropathy can affect just one nerve or many nerves simultaneously.
- When multiple nerves are involved it is known as polyneuropathy.
- When it’s just one, it’s known as mononeuropathy. (Cleveland Clinic. 2023)
Neuritis
- Neuritis is a type of neuropathy that indicates nerve inflammation. (American Association of Neurological Surgeons)
- Neuritis describes inflammation of peripheral nerves after they have exited the spinal column. (National Institutes of Health. U.S. National Library of Medicine. Medline Plus. 2022)
- Peripheral nerves are the long, thin strands that supply sensation, feeling, and movement impulses to all areas of the body located outside the central nervous system.
- Neuritis can lead to radicular pain, as well as other nerve symptoms. (National Institutes of Health. U.S. National Library of Medicine. Medline Plus. 2022)
Sciatica
- Sciatica describes symptoms that include radiating pain and sensations that travel into the hip, buttock, leg, and foot.
- One of the most common causes of sciatica is radiculopathy.
- Another is spinal stenosis. (Cleveland Clinic. 2023)
- Piriformis syndrome is where a tight buttock/piriformis muscle constricts the sciatic nerve, which runs underneath. (Cass SP. 2015)
Chiropractic
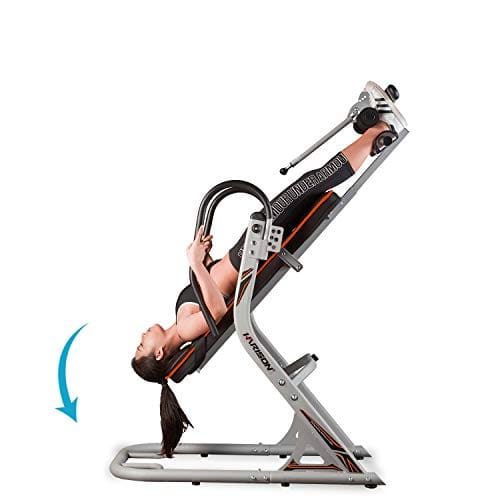
Chiropractic adjustments, non-surgical decompression, MET, and various massage therapies can relieve symptoms, release stuck or trapped nerves and restore function. Through the treatments, the chiropractor and therapists will explain what is happening and why they are using a specific technique. Knowing a little about how the neuromusculoskeletal system operates can help the healthcare provider and the patient in developing and adjusting effective treatment strategies.
Sciatica During Pregnancy
References
Michigan Medicine. Upper and Middle Back Pain.
American Academy of Neurological Surgeons. Anatomy of the Spine and Peripheral Nervous System.
Johns Hopkins Medicine. Health Conditions. Radiculopathy.
American Association of Neurological Surgeons. Herniated Disc.
American Academy of Orthopaedic Surgeons. OrthoInfo. Cervical Radiculopathy (Pinched Nerve).
Rothman, S. M., & Winkelstein, B. A. (2007). Chemical and mechanical nerve root insults induce differential behavioral sensitivity and glial activation that are enhanced in combination. Brain Research, 1181, 30–43. https://doi.org/10.1016/j.brainres.2007.08.064
Murray G. M. (2009). Guest Editorial: referred pain. Journal of applied oral science: Revista FOB, 17(6), i. https://doi.org/10.1590/s1678-77572009000600001
American Academy of Orthopaedic Surgeons. OrthoInfo. Carpal Tunnel Syndrome.
Bostelmann, R., Zella, S., Steiger, H. J., & Petridis, A. K. (2016). Could Spinal Canal Compression be a Cause of Polyneuropathy? Clinics and practice, 6(1), 816. https://doi.org/10.4081/cp.2016.816
Cleveland Clinic. Mononeuropathy.
American Association of Neurological Surgeons. Glossary of Neurosurgical Terminology.
National Institutes of Health. U.S. National Library of Medicine. Medline Plus. Peripheral Nerve Disorders.
Cleveland Clinic. Spinal Stenosis.
Cass S. P. (2015). Piriformis syndrome: a cause of non-discogenic sciatica. Current sports medicine reports 14(1), 41–44. https://doi.org/10.1249/JSR.0000000000000110