“For individuals affected by headaches that occur 15 or more days a month for more than three months, can knowing the signs and symptoms help healthcare providers help treat and prevent chronic tension headaches?”
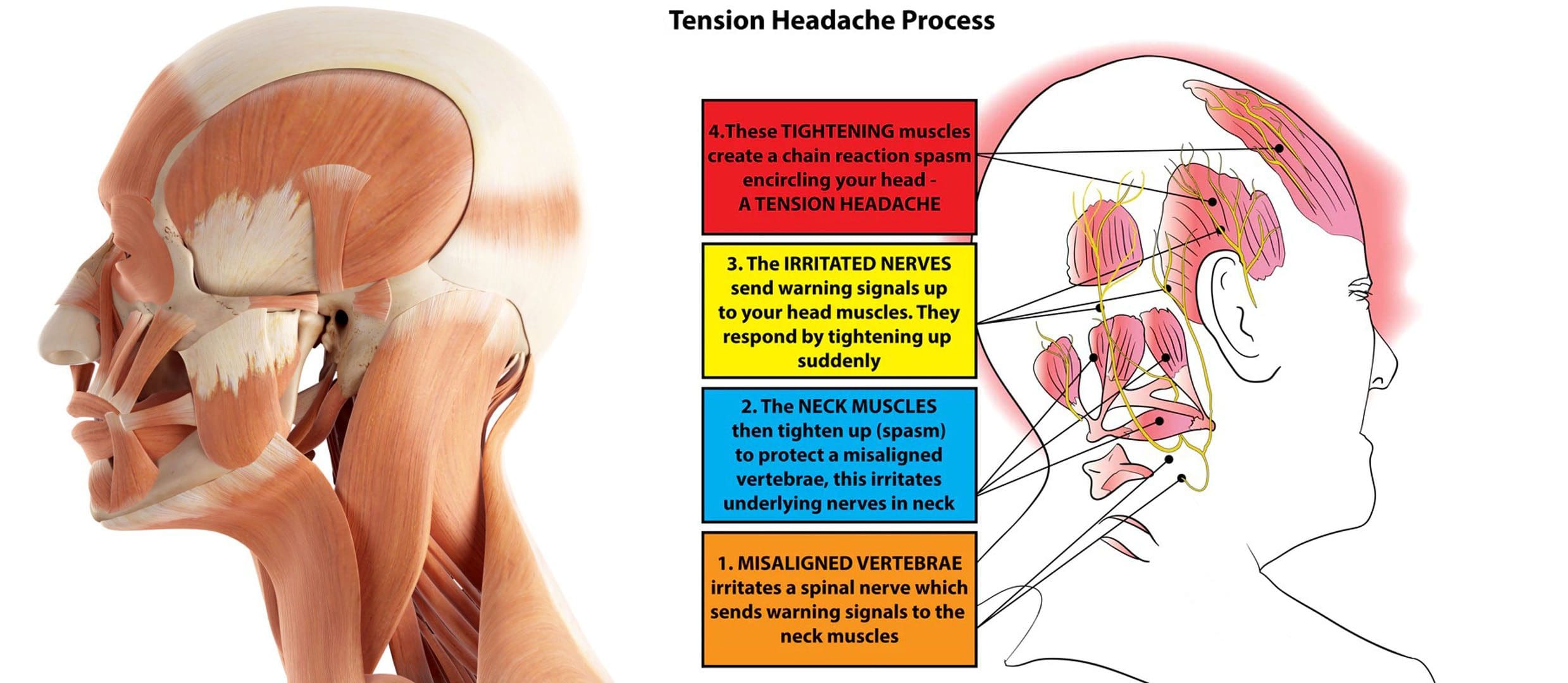
Table of Contents
Chronic Tension Headaches
Most individuals have experienced a tension-type headache. The pain is usually described as a dull tightening or pressure on both sides of the head, like having a tightening band around the head. Some individuals experience these headaches frequently, a condition known as chronic tension headaches. Chronic tension headaches are uncommon but can be debilitating, as they can interfere with a healthy quality of life and daily living.
- Tension headaches are typically caused by stress, anxiety, dehydration, fasting, or lack of sleep and usually resolve with over-the-counter medications. (Cleveland Clinic. 2023)
- This is a primary headache disorder that affects around 3% of the population.
- Chronic tension headaches can occur daily and negatively impact the quality of life and daily functioning. (Cleveland Clinic. 2023)
Symptoms
- Tension headaches can be referred to as stress headaches or muscle contraction headaches.
- They can present with dull, aching pain and include tightness or pressure across the forehead, sides, or back of the head. (Cleveland Clinic. 2023)
- Additionally, some individuals experience tenderness on the scalp, neck, and shoulders.
- Chronic tension headaches materialize 15 or more days a month on average for more than three months.
- The headache can last for several hours or be continuous for several days.
Causes
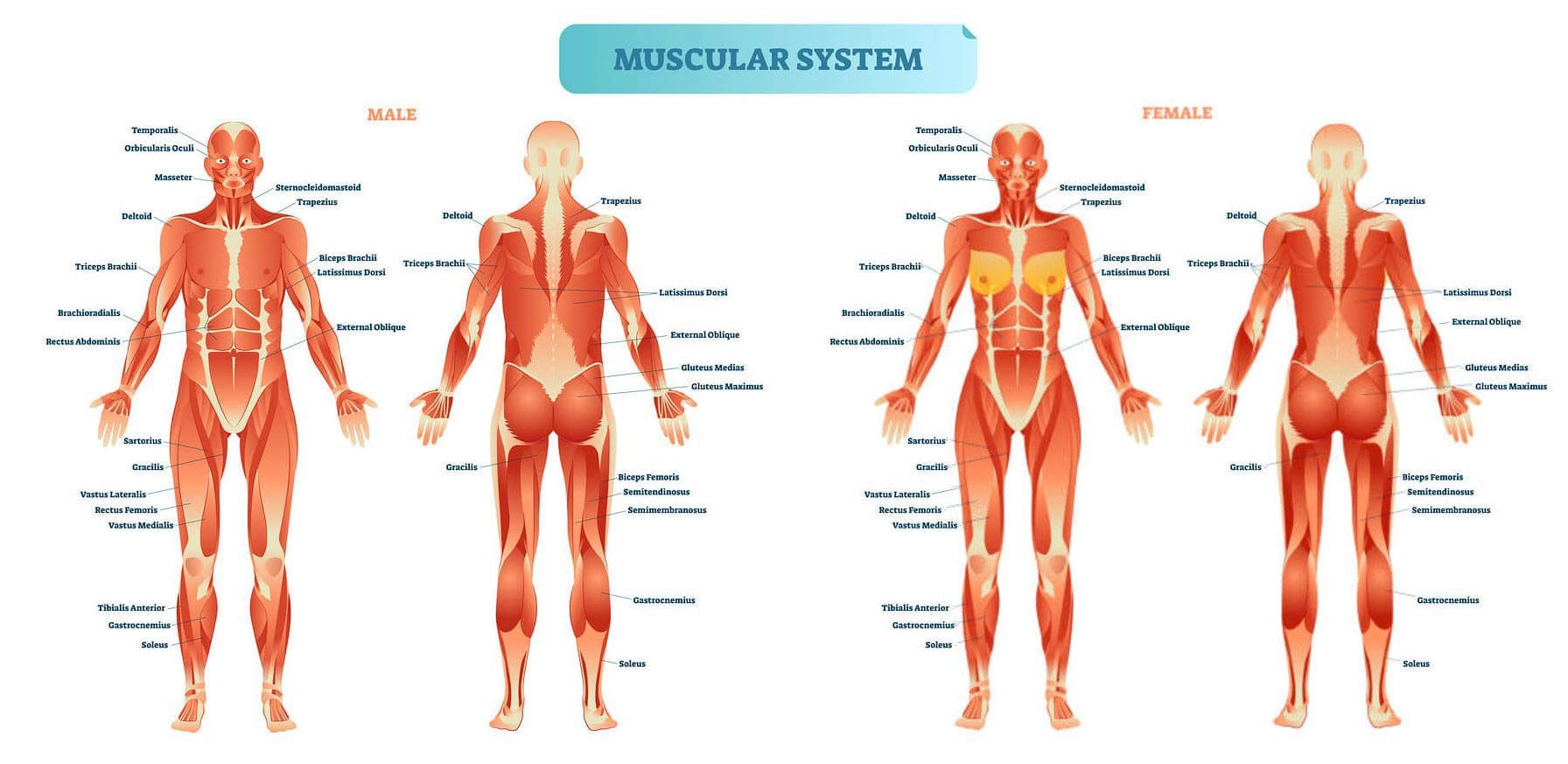
- Tension headaches are typically caused by tight muscles in the shoulders, neck, jaw, and scalp.
- Teeth grinding/bruxism and jaw clenching can also contribute to the condition.
- Headaches can be brought on by stress, depression, or anxiety and are more common in individuals who:
- Work long hours in stressful jobs.
- Don’t get enough sleep.
- Skip meals.
- Frequently consume alcohol. (Cleveland Clinic. 2023)
Diagnosis
Individuals experiencing headaches that interfere with daily life or need to take medication more than twice a week are recommended to consult a healthcare provider. Before the appointment, it can be helpful to keep a headache diary:
- Record the days
- Times
- Description of the pain, intensity, and other symptoms.
Some questions the healthcare provider may ask include:
- Is the pain pulsating, sharp, or stabbing, or is it constant and dull?
- Where is the pain most intense?
- Is it all over the head, on one side, on the forehead, or behind the eyes?
- Do the headaches interfere with sleep?
- Is working or doing tasks difficult or impossible?
A healthcare provider will likely be able to diagnose the condition based on symptoms alone. However, if the headache pattern is unique or different, the provider may order imaging tests, like MRI or CT scans, to rule out other diagnoses. Chronic tension headaches can be confused with other chronic daily headache disorders like chronic migraine, hemicrania continua, temporomandibular joint dysfunction/TMJ, or cluster headaches. (Fayyaz Ahmed. 2012)
Treatment
Pharmacological therapy for chronic tension headaches usually involves preventive medication.
- Amitriptyline is one medication that has been found to be beneficial in chronic tension headache prevention.
- A tricyclic antidepressant is a sedating medication and is usually taken before sleeping. (Jeffrey L. Jackson et al., 2017)
- According to a meta-analysis of 22 published studies in the Journal of General Internal Medicine, these medications are superior to placebo in reducing headache frequency, with an average of 4.8 fewer headache days per month.
Additional preventive medications may include other antidepressants like:
- Remeron – mirtazapine.
- Anti-seizure medications – like Neurontin – gabapentin, or Topamax – topiramate.
A healthcare provider may also prescribe medication to treat headache episodes, which include:
- Prescription non-steroidal anti-inflammatory drugs or NSAIDs, including acetaminophen, naproxen, indomethacin, or ketorolac.
- Opiates
- Muscle relaxants
- Benzodiazepines – Valium
Non-Medication Treatment
Behavioral therapies are sometimes used on their own or in combination with medication to prevent and manage chronic tension headaches. Examples include:
Acupuncture
- An alternative therapy that involves using needles to stimulate specific points on the body believed to connect with certain pathways/meridians that carry vital energy/chi throughout the body.
Biofeedback
- In Electromyography – EMG biofeedback, electrodes are placed on the scalp, neck, and upper body to detect muscle contraction.
- The patient is trained to control muscle tension to prevent headaches. (William J. Mullally et al., 2009)
- The process can be costly and time-consuming, and there is little evidence to support its effectiveness.
Physical Therapy
- A physical therapist can work out stiff and tight muscles.
- Train individuals on stretches and targeted exercises for loosening tight head and neck muscles.
Cognitive Behavioral Therapy/CBT
- Involves learning how to identify headache triggers and cope in a less stressful and more adaptive way.
- Headache specialists often recommend CBT in addition to medication when developing a treatment plan. (Katrin Probyn et al., 2017)
- Teeth-grinding and jaw-clenching training/treatment can help when they are contributors.
- Regular exercise, as well as practicing healthy sleep hygiene, can be beneficial in prevention.
Supplements
Some individuals with chronic tension headaches may find relief using supplements. The American Academy of Neurology and the American Headache Society report the following supplements can be effective: (National Center for Complementary and Integrative Health. 2021)
- Butterbur
- Feverfew
- Magnesium
- Riboflavin
If the headaches come on suddenly, cause waking up from sleep, or last for days, it’s important to consult a healthcare provider to rule out any underlying causes and develop a personalized treatment plan.
Tension Headaches
References
Cleveland Clinic. (2023). Tension Headaches.
Ahmed F. (2012). Headache disorders: differentiating and managing the common subtypes. British journal of pain, 6(3), 124–132. https://doi.org/10.1177/2049463712459691
Jackson, J. L., Mancuso, J. M., Nickoloff, S., Bernstein, R., & Kay, C. (2017). Tricyclic and Tetracyclic Antidepressants for the Prevention of Frequent Episodic or Chronic Tension-Type Headache in Adults: A Systematic Review and Meta-Analysis. Journal of general internal medicine, 32(12), 1351–1358. https://doi.org/10.1007/s11606-017-4121-z
Mullally, W. J., Hall, K., & Goldstein, R. (2009). Efficacy of biofeedback in the treatment of migraine and tension type headaches. Pain physician, 12(6), 1005–1011.
Probyn, K., Bowers, H., Mistry, D., Caldwell, F., Underwood, M., Patel, S., Sandhu, H. K., Matharu, M., Pincus, T., & CHESS team. (2017). Non-pharmacological self-management for people living with migraine or tension-type headache: a systematic review including analysis of intervention components. BMJ open, 7(8), e016670. https://doi.org/10.1136/bmjopen-2017-016670
National Center for Complementary and Integrative Health. (2021). Headaches: What You Need To Know.