How do healthcare professionals in a chiropractic clinic provide a clinical approach to recognizing impairment for individuals in pain?
Introduction
Any article you read about substance abuse among nurses will almost certainly repeat the claims made by the American Nurses Association, which states that, in line with the general public, 10% of nurses, or one in ten or about 300,000 Registered Nurses in the United States, are dependent on drugs of some kind. Impairment of any kind at work, particularly if it stems from substance misuse or usage, can have serious repercussions for the nurse and the nursing profession for several reasons. Preciseness, correctness, the capacity for critical thought, and observation are essential in the nursing profession. Because errors or accidents may occur, any inability to deliver these abilities puts patients, coworkers, and the nurse at risk. Additionally, people view nurses as trustworthy, dependable, and honest. Impairment can damage that perception, particularly if it is brought on by alcohol or drugs. In the following sections, we’ll examine impairment, its reasons, and your ethical and legal obligations if you believe a coworker is impaired. Today’s article focuses on the clinical approach to recognizing impairment in a clinical setting. We discuss with certified associated medical providers who consolidate our patients’ information to assess pain-like issues they are experiencing. We also inform and guide patients on various treatments and ask intricate questions to their associated medical providers to integrate a customized treatment plan. Dr. Jimenez, D.C., includes this information as an academic service. Disclaimer.
A Definition of Impairment
The fundamental definition of impairment is “The state of being decreased, weakened or harmed, especially mentally or physically” (“Impairment,” n.d.”) You’ll see that this is merely a description of a state of being and that no reason is given. This is a result of the abundance of possible reasons. While some causes might be simple to prove, others might not. Consequently, it is important to identify and consider the context and cause, if known, while talking about impairment. The impaired populace that surrounds us as nurses is: They are patients of ours. They are in a reduced, weakened, or damaged state, albeit they may be compromised by disease or injury. Similarly, you are compromised by illness if you have worked a shift with a bad cold. Symptoms of feeling slower, impaired thinking, and reviewing your work more frequently are examples of impairment in a clinical setting.
A disease or injury may have different consequences and affect how well you execute your job to varied degrees, but as the degree of impairment increases, so does the chance that you will make a mistake. The safety of both you and those around you, including your patients and coworkers, is inversely correlated with your degree of impairment. You, your patients, and your coworkers are less safe the more your performance is negatively impacted. Even though nurses know that the patients are vulnerable because they are compromised in some way. We also know that impairments can make it more likely for you to make mistakes. You are a responsible person and would never work if your impairment was severe enough to put your patients in danger. However, what if a coworker has a disability? Even worse, what if you think it was somehow self-inflicted? How do you proceed? Do you talk to them? Do you inform someone else about it? Do you hope nothing bad happens and ignore it?
Preserving patient safety is a top priority for nurses in their line of work. It is your responsibility to know what to do and how to do it if a colleague appears to be affected. But to achieve that, you must be able to spot potential impairment in both you and other people. Administrative and required reporting requirements must be known to you. You also need to be aware of the possible consequences for yourself if you do nothing.
Causes of Impairment
You might assume that we are discussing drug usage the moment you hear or read the phrase impairment in the workplace. However, there are other potential causes besides alcohol or drug abuse, and drawing the wrong conclusions can frequently have unanticipated results. You are not required to look into or determine what’s causing your colleague’s apparent disability. That is the task of others. You must identify impairment indicators and take the proper action. One of the things you should consider before reporting a coworker for drug addiction is whether or not you are witnessing real impairment. Everyone has occasional feelings of illness, irritability, or tension. Even if we might not be as effective as usual, nothing about our performance puts anyone at risk, and it doesn’t happen often. “Impairment in the healthcare system is defined as the inability or impending inability to practice, which is divided into two categories that can affect both the professional and the patient” (Baldisseri, 2007). This statement dismisses the previous scenario in which you might move more slowly than usual due to a severe cold.
Functional Medicine Influence Beyond Joints- Video
The Difference Between Impairment & A Bad Day
“Impairment is characterized by the inability to carry out the professional duties and responsibilities reasonably consistent with nursing standards.” Having a bad day can affect the individual’s mood and workflow. Sometimes, a faint impression that someone is not quite themselves leads to this discovery. Colleagues could experience unease or feel intimidated. Supervisors may notice a rise in the number of grievances lodged against an employee or by coworkers against that individual. Behavioral patterns suggest issues exist and can lead to the development of causing medical errors. Medical errors in healthcare organizations can create a serious health problem that can substantially threaten the patient’s safety. (Rodziewicz et al., 2024). Before examining these patterns, let’s consider some of the potential reasons other than drug or substance misuse that could be contributing to the decline in risky practices in nursing tasks.
Training & Education Deficits
A coworker’s risky activities could result from inadequate training, knowledge, or orientation to the current workplace. This is particularly valid for recently licensed nurses and nurses transitioning from one practice area to another. Nurses in refresher training may need to be more confident in how things have traditionally been done or need to be taught suggested modifications to policy or procedures. Refresher training may also encounter opposition or change and need to be successful. If the nurse is unwilling to acknowledge that their knowledge or abilities are not up to par, these educational deficiencies may appear as impairment. They might take much longer than other nurses to do jobs, among other indicators. Erroneous assumptions about which process is the most reasonable or accurate way to complete a task might lead to mistakes on the part of the nurse. Alternatively, they could be overly sensitive to criticism and try to maintain their composure by insisting they are competent.
Physical Illness
We have already discussed the issue of trying to work when you have a bad cold. For most of us, the experience of having a little illness or infection holding us back is probably known. Yet, increased chronic conditions could also lead to compromised performance days. Like many other ailments, diabetes, and arthritis can cause someone to feel less than 100% of themselves on certain days. It’s important to remember that you might not even be aware that your coworker has these ailments. For want of a better or more appropriate title to put this under, be sure the person you are about to accuse of abusing drugs is not pregnant before moving forward. Naturally, this is a partial list of all potential physical explanations. It’s merely a friendly reminder to consider the chance the incompetent nurse could be physically unwell.
Physical Injury
Like medical conditions, injuries can also hinder one’s ability to perform at work. Although it is more likely that there may be some overt signs of an injury—such as a limp or other unnatural movement, bandaged regions, or the use of a walking stick or other mechanical aid—this isn’t always the case. A person with a back strain or some different type of nerve entrapment could try to disguise their discomfort and their limits.
Stress & Fatigue
Since it is common for these causes to occur together or for one to manifest as a symptom of the other, they might be seen as a collective cause. They may also be the outcome of events outside the workplace, inside the workplace, or both. Someone who has recently gone through a divorce or someone who is the primary caregiver for a critically ill relative at home are two examples. Both scenarios are unpleasant, but what if these factors were secondary to financial difficulties? Both worrying about this and attempting to work more shifts due to their economic challenges may hurt their ability to sleep. Someone in these situations can easily get psychologically and physically fatigued very fast. Depending on their personality, it would also be unheard of for their colleagues to be unconscious of these difficulties. Alternatively, the cause might be as straightforward as stress at work, resulting in burnout and decreased motivation. Burnout and work dissatisfaction are, in fact, “common within the nursing profession” (Van Bogaert et al., 2017)
Mental Illness
Even though nurses like to think of themselves as resilient and unaffected by situations that others would see as weakness, the truth is that we are vulnerable to mental health issues like anxiety and depression, as well as drug use disorders, for many of the same reasons. In certain nursing specialties, we work with patients who are dying all the time—possibly even infant deaths—or we witness horrifying results from violent or accidental incidents. Circumstances like these may serve as antecedents to illnesses like Post Traumatic Stress Disorder (PTSD). Nurses are not superwomen or supermen—again, these are only a few examples. Healthcare professionals may be impacted if it impacts the broader public.
Substance Use
Substance addiction is perhaps the most chronic and damaging to the individual, the facility, and even the profession, even if it isn’t necessarily more common than the previously described causes of impairment. Substance abuse is not likely to go away on its own over time without assistance from coworkers and superiors, unlike medical conditions or injuries. This does not imply that interventions for other impairment causes are unnecessary or should be avoided. If you don’t act when something like low back pain is the cause of the impairment, you can end up addicted to painkillers in the first place. Included in the collection under this subject is disability brought on by the misuse or overuse of pharmaceuticals that have been prescribed to them or others. The impairment is frequently associated with the side effects of overuse or acute overdose. At the same time, it can also occasionally arise from adverse events associated with normal doses, such as nausea, sleepiness, or dizziness. The usage or misuse of “street drugs” or non-prescription substances like methamphetamine, ecstasy, or cannabis. The acute or chronic misuse or overuse of alcohol. The nurse may be severely intoxicated or experiencing a severe hangover, but both conditions would impede her abilities. Chronic use can also result in physical ailments or cognitive impairments that make it difficult for a nurse to perform at a high enough level. Since a nurse’s whole self-definition frequently centers around their work as a nurse, the entry of their abuse or addiction into their place of employment is often a sign of how far along their illness has evolved.
Because health workers identify with their line of work, evidence of disease sometimes points to a late stage of illness. Workplace issues are typically the last stage of a downhill spiral, and when a disease is discovered, coworkers are frequently astonished “(Washington State Department of Health, 2016, p.6). When the impairment is initially seen at work, coworkers and bosses may even deny or minimize the issue, offering justifications or avoiding confrontation in the hopes that the issue will magically disappear.
Unique Risk Factors For Nurses
The likelihood of having a drug use disorder is influenced by a variety of factors, including heredity, upbringing, parental and peer pressure, and so on. However, working as a nurse presents a few unique risk factors that are not present in other occupations. The main hour risk factors that nurses deal with in a healthcare facility are:
Acess & Attitude
Drugs that are lawful to obtain by prescription are more likely to be used by nurses than by the general public, even though substance use disorders do not affect nurses more frequently than the general population. The explanation is that nurses handle these medications daily, even without a prescription. To this, we add our knowledge of medicine administration, usage, and dosage and work in a setting where the benefits of medication use are evident. This indicates that we are self-assured in our capacity to diagnose and treat ourselves and in our ability to handle these medications.
Stress
Some of the indications that all nurses are sometimes a part of the stress factors that have caused them to be impaired include:
- Extended shifts
- Heavy workload
- Absence of personnel
- Extremely urgent patients while retaining composure under intensely sentimental circumstances.
These are presumably well-known to all nurses and can occasionally be attributed to role strain. They are all a necessary component of a very demanding line of work. Work schedules alone have demonstrated a beneficial relationship with substance usage. Pain or insomnia following a demanding shift are common and often serve as the primary justification for taking medication to help with aches and pains, promote relaxation, or fall asleep.
Lack of Education
Here, the term “lack of education” does not mean ignorance of drugs. As we’ve already mentioned, there is no shortage of schooling there. No. In this context, ignorance of substance use problems and associated warning signs and symptoms is meant. Many times, healthcare professionals are unable to identify these symptoms and indicators in both themselves and other people. Even if they do identify them, stigmatization results from a lack of information about these disorders—especially if the sufferer is a fellow healthcare worker—because we tend to hold healthcare professionals—including ourselves—to higher standards than we do non-healthcare workers.
Recognizing The Signs
When a nurse is caught using drugs or alcohol at work, the ideal course of action these days is assistance and therapy rather than immediate termination. The idea is that the nurse will eventually be able to go back to work following treatment and rehabilitation. However, early intervention is a key component of this strategy. As we’ve already mentioned, substance use may need to continue for a while before signs of impairment at work become apparent. Therefore, in pursuing a successful result, time itself becomes a threat. It is appropriate to remind ourselves that substance abuse may not be the only explanation for the impairment as we examine some of the indicators that substance use may cause. For the sake of the patients’ and the staff’s safety, intervention is required regardless of the cause. Searching for behavioral changes or changes from a baseline rather than specific activities is perhaps more beneficial. After all, we all know that a nurse who is not incompetent but has always appeared messy or moves a little more slowly than others when completing tasks. Perhaps it’s just a personal preference, but if a nurse who used to appear well-groomed and productive suddenly starts to act sluggish and careless, there may be a deeper issue at hand.
On the other hand, it is also noteworthy if the nurse, who has always been sluggish and sloppy but has always stayed within acceptable parameters, suddenly became unacceptable or extremely slow and messy. However, the noticeable shift might be outside the condition of their attire. Even someone who is usually upbeat can seem depressed, nervous, or afraid. A typically quiet individual can appear animated, talkative, and gregarious. It’s also possible that the shy person isolates themselves more than usual, or the ordinarily talkative and active person becomes even more talkative and active than normal. Recall that the behavior is less important in many cases than the change in pointing out a problem. It is similar to checking for deviations from normal blood pressure or temperature as a sign of an issue. Additional indicators of a change to watch out for include:
- Mood swings
- Irritability
- Drowsiness
- Crying or inappropriate laughing
- Suspicion or being extremely sensitive to criticism.
- Inflexibility or excessive adherence to procedures when they are not required.
- Bewilderment, or bad memory
When it comes to work performance, you could observe the following:
- A rise in tardiness and absences, particularly when they follow a pattern.
- Strange explanations for absences
- Longer or more regular pauses
- Uncharacteristic absences from the workplace,
- Previously, ordinary tasks required more time.
- Unusual or dubious “shortcuts” used in operations do not uphold the anticipated level of care.
- When the quality or content of the charting becomes shoddy or unique, there are greater inaccuracies and negligence.
- A rise in the nurse’s complaints or grievances.
Each of them points to a possible issue. They could be overtly apparent or strange enough to give you the impression that something is off. You may notice that they are using breath fresheners, mints, or chewing gum more frequently than they used to. They may mumble more than usual or exhibit more subtly stopped speech with longer silence while considering their response. “Were their pupils constricted (or dilated)?” or “Was that alcohol I smelled?” are some questions to ask yourself as you leave. As nurses, we may acquire hunches or intuition. Our innate ability to observe results from our extensive training and these instincts are frequently founded on observations we make unconsciously. Thus, please don’t ignore them. While you shouldn’t ignore them, you shouldn’t accept them as gospel.
Drug Diversion
Access to the drug of choice may be restricted for a nurse with a substance use disorder when they are not working. This could be for various reasons, such as the fact that their family is no longer prescribed that particular drug, their doctor or pharmacist becoming suspicious, or other reasons. They frequently attempt to supplement that access from the job in this kind of circumstance. And the nurse will need to be creative in hiding this behavior due to the precautions in place, particularly when it comes to banned substances.
Among the warning indicators to look out for are:
- Regularly or eagerly offering to be a pharmaceutical nurse.
- Patients continue to complain about discomfort even after receiving painkillers.
- Documents reveal that the patient was given more painkillers than necessary for their condition.
- There are more and more reports of drug spills and waste.
- When this nurse performs medication rounds relative to other nurses, an abnormally high number of controlled drugs are administered.
Drug counts are inaccurate; If you have yet to witness a drug given or dispensed, the nurse may ask you to co-sign for it. This is a partial list, just like the others. As with the other lists, nurses are very wise due to our education, training, and experiences, so sometimes it’s just a gut instinct that warns you of a possible issue. However, as a general guideline, anything that feels off should be looked into further. Your obligations to your patients and your coworkers require this.
Interventions
The Florida Nurse Practice Act is broken when a nurse practices while intoxicated. Both illness and substance use are listed as potential causes of this impairment in the paragraph that defines this as a violation and could result in disciplinary action. It would also be illegal to fail to disclose a nurse’s impairment or to put a patient’s safety in peril by permitting them to work while impaired. It is preferable for everyone if there is no attempt to cover for the nurse or if the issue is ignored in the hopes that it will go away. As an employee, you should be fully conversant with the regulations and procedures each facility has likely designed for just these scenarios. These will have been created to guarantee compliance with all legal and regulatory obligations. It is never appropriate for you to approach a coworker who is impaired. Always ask a supervisor or nursing manager for assistance. The manager or supervisor will probably contact the impaired nurse first; however, having multiple people present during the intervention will:
- Give the evidence given to the nurse more weight because she is likely to dispute impairment.
- Present witnesses for incidents that might be needed in hearings or meetings later.
- Provide strength to the message, emotional support, and uphold safety if the nurse exhibits agitation or aggression when contacted.
- Never should the initial intervention be accusatory or involve attempting to identify the nurse’s issue.
It should be fact-based and provide written evidence of observations and concerns to make the nurse realize why you are requesting them to stop working now. The impairment and any subsequent intervention might be reported in one of two ways. The Florida State Board of Nursing is the first of them. More precisely, the Department of Health would receive the report, investigate the complaints, and take appropriate action. The second action would be to send the report to the Intervention Project for Nurses (IPN). The IPN was created in 1983 by legislative action to protect the public’s health and safety (Chan et al., 2019). It does this by offering close supervision to nurses who are deemed unsafe to practice because of impairments brought on by drug or alcohol abuse, misuse, or both, or because of a physical or mental illness that may impair the licensee’s capacity to practice safely and skillfully.
These alternative-to-discipline programs have been developed across the nation, and in Florida, they are part of the Integrated Patient Network (IPN) because of the recognition that a nurse with a substance use disorder should receive the same care and treatment as anyone else. Through its programs, nurses can obtain non-punitive treatment and rehabilitation. The IPN will assist the nurse’s successful return to practice if she consents to step away from the profession and finish the program while maintaining confidentiality—even from the Board of Nursing. The IPN will send the file to the Department of Health if a nurse accepts these terms but then changes their mind. Certain cases might be reported to the Department of Health and the IPN, where treatment AND disciplinary action might be started. The Department of Health’s participation might lead to the nurse’s license being suspended or revoked, making it more difficult for her to return to work. It is envisaged that by offering non-punitive routes, nurses will be encouraged to seek assistance before facing disciplinary action and may eventually be able to return to practice.
Conclusion
Because of the unique circumstances surrounding our education and training, the way we are perceived, and the fact that we perceive ourselves as somehow stronger than others, the issue of disability in the workplace for nurses is particularly complicated. In the past, if an employee was impaired at work, disciplinary action might have been taken because of the impairment itself or the mistakes made. This was particularly valid in cases where it was discovered that the nurse was intoxicated or impaired by another substance. You were out the door and never came back after that. You would also lose your license, preventing you from ever returning to work as a nurse. Thankfully, non-disciplinary initiatives have been sparked by recognizing that we are not immune to the same stressors as others. The idea behind these initiatives is to identify problems, including substance use disorders, early on so that the best possible outcome may be achieved for all parties.
References
Baldisseri, M. R. (2007). Impaired healthcare professional. Crit Care Med, 35(2 Suppl), S106-116. https://doi.org/10.1097/01.CCM.0000252918.87746.96
Chan, C. W. H., Ng, N. H. Y., Chan, H. Y. L., Wong, M. M. H., & Chow, K. M. (2019). A systematic review of the effects of advance care planning facilitators training programs. BMC Health Serv Res, 19(1), 362. https://doi.org/10.1186/s12913-019-4192-0
Hakim, A. (2023). Investigating the challenges of clinical education from the viewpoint of nursing educators and students: A cross-sectional study. SAGE Open Med, 11, 20503121221143578. https://doi.org/10.1177/20503121221143578
Impairment. (n.d.). In Dictionary.com Unabridged. Retrieved from http://www.dictionary.com/browse/impairment
Rodziewicz, T. L., Houseman, B., & Hipskind, J. E. (2024). Medical Error Reduction and Prevention. In StatPearls. https://www.ncbi.nlm.nih.gov/pubmed/29763131
Van Bogaert, P., Peremans, L., Van Heusden, D., Verspuy, M., Kureckova, V., Van de Cruys, Z., & Franck, E. (2017). Predictors of burnout, work engagement and nurse reported job outcomes and quality of care: a mixed method study. BMC Nurs, 16, 5. https://doi.org/10.1186/s12912-016-0200-4
Washington State Department of Health. (2016). A guide for assisting colleagues who demonstrate impairment in the workplace. Retrieved from http://www.doh.wa.gov/portals/1/Documents/Pubs/600006.pdf
Disclaimer








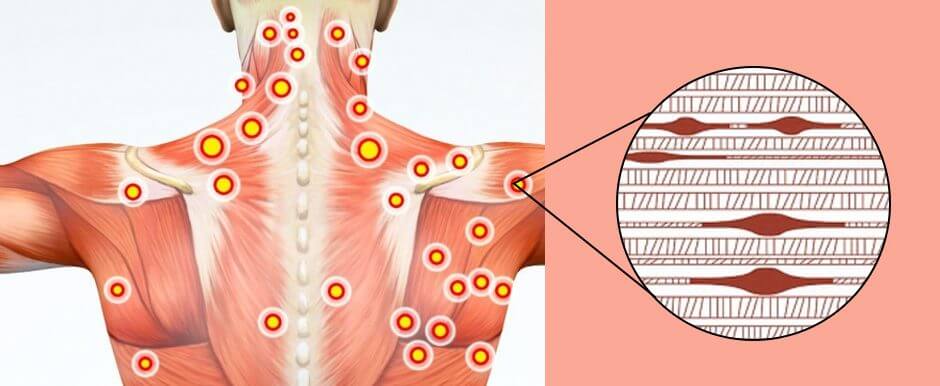
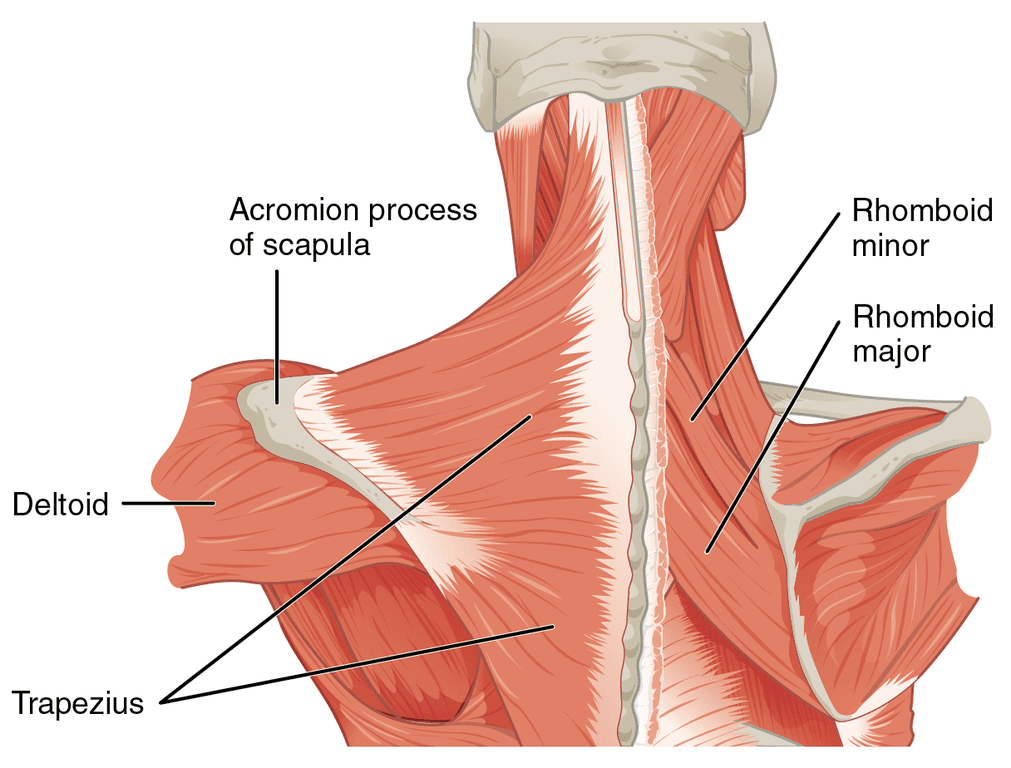
 Causes
Causes