Individuals dealing with symptoms like sudden pain, weakness, and tenderness in the back of the knee could have a hamstring injury. Can knowing the symptoms and performing self-care help bring relief?

Table of Contents
Hamstring Pain Behind The Knee
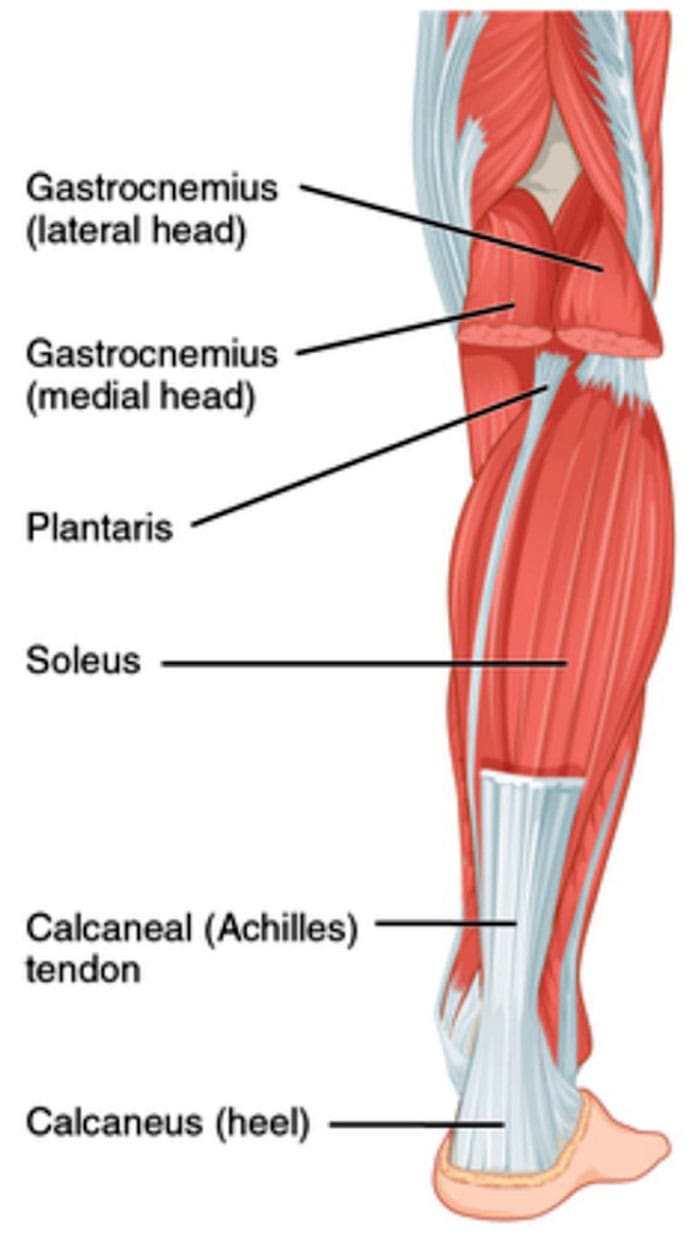
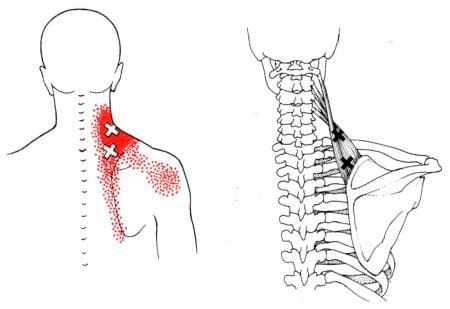
The hamstrings consist of three long muscles that run down the back of the thigh, cross over the back of the knee, and connect to bones in that area. A hamstring injury, such as a strain or tear, tendonitis, or biceps femoris tendinopathy, can cause pain in the back of the knee, difficulty bending the knee, swelling, and bruising. A hamstring strain occurs when the muscle is stretched too far or torn completely. This can happen from sudden, forceful movements or overstretching. Hamstring tendonitis develops over time, usually after a sudden increase in activity, when the hamstring tissue cannot recover from too much loading. Pain is often felt after physical activity and exercise and, in severe cases, during the activity or throughout the day. Biceps femoris tendinopathy can also cause pain in the back of the knee. Strains, tendonitis, bursitis, and muscle tears are all possible explanations for a hamstring injury that leads to pain behind the knee. Discussing pain symptoms with a healthcare provider is recommended, especially if it occurs suddenly during physical activity or exercise. They can help identify the exact cause and offer guidance for rehabilitation, including physical therapy referrals.
Causes and Triggers
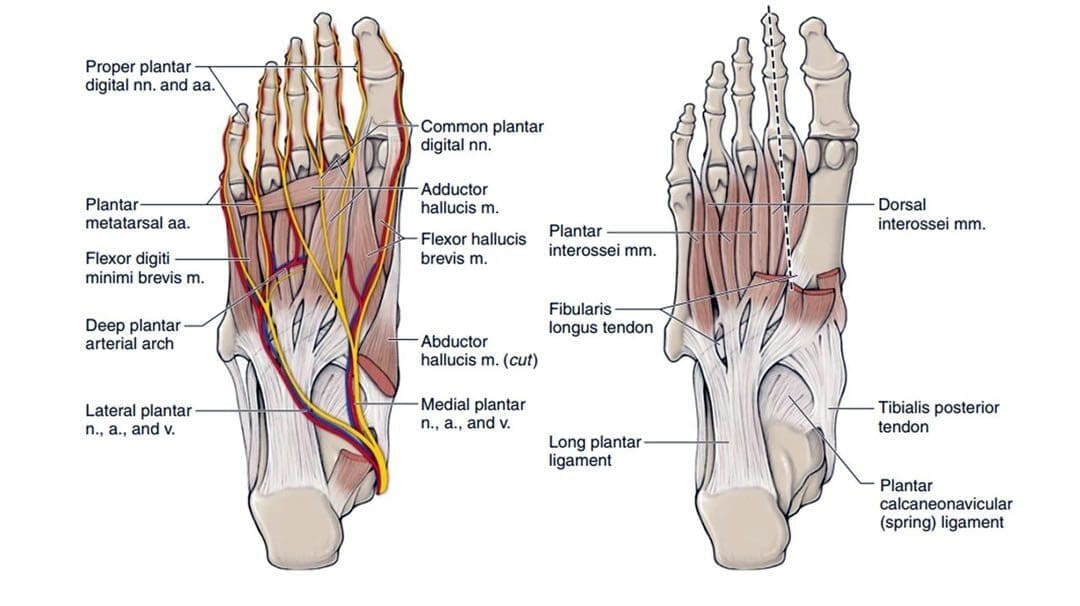
Individuals may experience hamstring pain behind the knee when the muscles in that area are overworked, inflamed, or injured, such as from activities like running, walking, dancing, soccer, or basketball. Possible types of injuries and their causes.
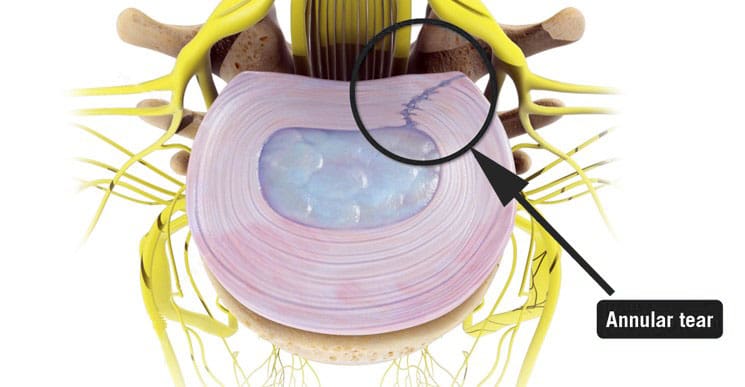
Tendonitis
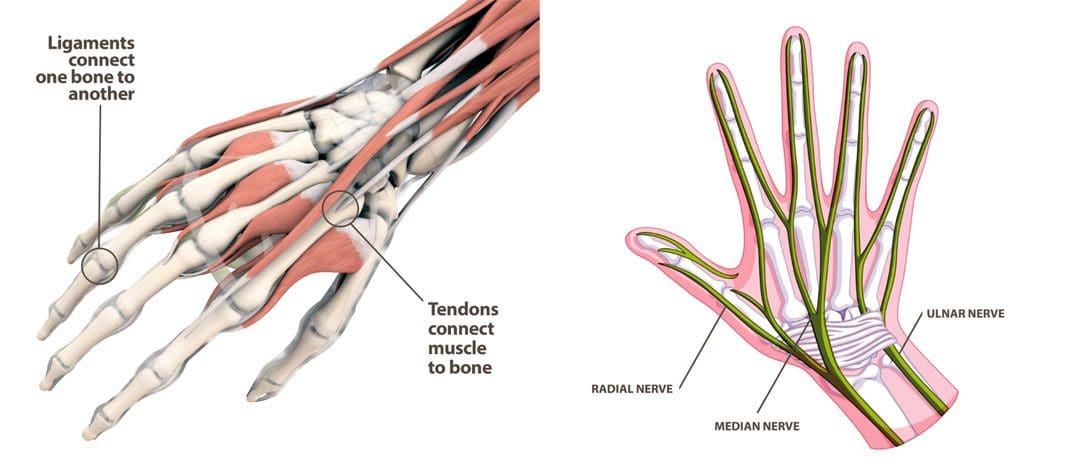
- The hamstring tendons connect behind the knee.
- When the tendons become inflamed due to overuse, they can lead to swelling and pain that worsen with activity. (National Library of Medicine, 2017) (American Academy of Orthopaedic Surgeons, 2020)
Strain or Tear
- A muscle strain occurs when the muscle is stretched too much, and the fibers tear.
- A hamstring strain is also called a pulled hamstring. (American Academy of Orthopaedic Surgeons, 2021)
Bursitis
- This is inflammation of tiny fluid-filled sacs that help cushion joints during movement.
- Inflammation from bursitis can affect the nerves within the hamstring, resulting in pain. (American Academy of Orthopaedic Surgeons, 2020)
Pes anserine
- This is a specific type of bursitis which affects the knee tendons. (American Academy of Orthopaedic Surgeons, 2021)
Muscle Overload
- A primary cause of muscle strain occurs when the muscle is stretched too far or has to handle a sudden force like sprinting or kicking. (American Academy of Orthopaedic Surgeons, 2021)
Severe Cases
Most causes of pain behind the knee are easily treatable at home with self-care and rest. However, it can be more severe, signaling a blood clot, infection, torn muscle or tendon/ligament. Hamstring knee pain may be serious if any of the following is experienced (American Academy of Orthopaedic Surgeons, 2021)
- Sudden pain during physical activity, often during a full stride.
- Feeling a pop or sharp pain that causes falling or limping.
- Pain that worsens over time and prevents or hinders walking or exercising as normal.
If pain is severe and does not improve with rest and anti-inflammatory medications, evaluation by a healthcare professional is necessary.
Assesses Hamstring Pain
A healthcare provider will ask about symptoms and injury, including what happened when the pain began. They will perform a physical examination, which may include pressing on the back of the thigh to look for swelling, bruising, tenderness, or bunched-up muscles. (American Academy of Orthopaedic Surgeons, 2021) The healthcare provider will ask the patient to perform specific resisted movements, such as the manual muscle test, and measure the range of motion. Diagnostic testing includes an X-ray or MRI to determine the degree of the injury and which soft tissues or bones may be involved.
Self-Care
The first line of treating hamstring knee pain is the RICE protocol, which includes: (Mount Siani, 2024)
Rest
- Stop any activity that causes symptoms and pain.
- A healthcare provider may recommend crutches or a knee scooter in severe cases.
Ice
- Apply cold packs to the swollen or painful area for 20 minutes throughout the day.
Compression
- A knee brace, wrap, or bandage that applies gentle pressure to the injured area can help reduce and prevent swelling.
Elevation
- Lifting the leg higher than the heart will help reduce swelling and blood accumulation.
- Individuals may need to lie on a bed or sofa and elevate their legs with pillows.
Individuals can use at-home pain relievers like acetaminophen or NSAIDs like ibuprofen or naproxen. Over time, and depending on the severity of the injury, a healthcare provider will advise on gentle hamstring stretches and how to ease back into physical activity.
Professional Therapy and Surgical Treatments
Depending on the severity of the condition, a healthcare provider may recommend additional interventions, that include (American Academy of Orthopaedic Surgeons, 2021)
Immobilization
- A healthcare provider will advise immobilizing the knee to help with muscle healing, which could involve wearing a knee brace or using crutches.
Physical therapy
- A healthcare provider may refer the patient to a physical therapist, who will perform a personalized evaluation and prescribe targeted exercises to heal the injury and regain strength, flexibility, and movement.
Surgery
- Tendon avulsion injuries are when the hamstring tendon completely tears away from the bone, and surgery is required to reattach the tendon.
Platelet-rich plasma – PRP
- Platelet-rich plasma has become an additional treatment for hamstring muscle strain or tendonitis. (Seow D. et al., 2021)
- The treatment involves injecting a solution from the patient’s blood into the muscle to heal the injury.
Recovery
Predicting how long a hamstring injury takes to heal and how long the pain will linger depends on the type, location, and severity. The most severe type is the hamstring coming unattached around the knee. This surgical repair and rehabilitation take at least three months before returning to sports and exercise (American Academy of Orthopaedic Surgeons, 2021). Lesser injuries like tendonitis or a mild strain can take less time to heal. However, it’s essential to avoid reinjuring the area so the condition does not become chronic. This includes: (American Academy of Orthopaedic Surgeons, 2021)
- Stretching to encourage and maintain flexibility.
- Fixing muscle imbalances between the quadriceps and hamstring.
- Endurance and conditioning.
- Avoiding overuse.
Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to develop personalized treatment programs. We focus on what works for you and use an integrated approach to treating injuries and chronic pain syndromes to improve flexibility, mobility, and agility, relieving pain and helping individuals return to normal activities. If other treatments are needed, Dr. Jimenez has teamed up with top surgeons, clinical specialists, medical researchers, and rehabilitation providers. Our providers use Functional Medicine, Acupuncture, Electro-Acupuncture, and Sports Medicine principles.
Chiropractic Care for Leg Instability
References
National Library of Medicine. (2017). Tendinitis Also called: Tendonitis. Retrieved from https://medlineplus.gov/tendinitis.html
American Academy of Orthopaedic Surgeons. OrthoInfo. (2020). Sprains, strains, and other soft tissue injuries. https://orthoinfo.aaos.org/en/diseases–conditions/sprains-strains-and-other-soft-tissue-injuries/
American Academy of Orthopaedic Surgeons. OrthoInfo. (2021). Hamstring muscle injuries. https://orthoinfo.aaos.org/en/diseases–conditions/hamstring-muscle-injuries/
American Academy of Orthopaedic Surgeons. OrthoInfo. (2021). Pes aserine (knee tendon) bursitis. https://orthoinfo.aaos.org/en/diseases–conditions/pes-anserine-knee-tendon-bursitis/
Mount Siani. (2024). Hamstring strain – aftercare. https://www.mountsinai.org/health-library/selfcare-instructions/hamstring-strain-aftercare
Seow, D., Shimozono, Y., Tengku Yusof, T. N. B., Yasui, Y., Massey, A., & Kennedy, J. G. (2021). Platelet-Rich Plasma Injection for the Treatment of Hamstring Injuries: A Systematic Review and Meta-analysis With Best-Worst Case Analysis. The American journal of sports medicine, 49(2), 529–537. https://doi.org/10.1177/0363546520916729









 Extensor Tendonitis
Extensor Tendonitis