Can bioidentical hormone replacement therapy can help many individuals dealing with pain and fatigue while regulating hormone function?
Introduction
Many individuals have dealt with pain and discomfort in their bodies due to environmental factors that can impact the various muscles, tissues, organs, and bones. However, environmental factors can also affect the body’s hormones. They can cause overlapping risk profiles that can cause disastrous issues like pain, fatigue, unexplained weight changes, and even visceral-somatic issues. However, many individuals can seek various treatments to replenish their hormones and start getting back to their normal selves. In this 2-part article series, we will look at what hormones are exactly, what hormone replacement therapy is, and what types of hormones are in our bodies. In part 2, we will go in-depth with hormone therapy and its beneficial properties. We talk with certified associated medical providers who inform our patients about hormone therapy and how it can help provide helpful results to reduce pain in the body. While asking their associated medical provider intricate questions, we advise patients to incorporate non-surgical treatments combined with hormone therapy to reduce pain and discomfort from returning to the body. Dr. Alex Jimenez, D.C., includes this information as an academic service. Disclaimer.
What Are Hormones?
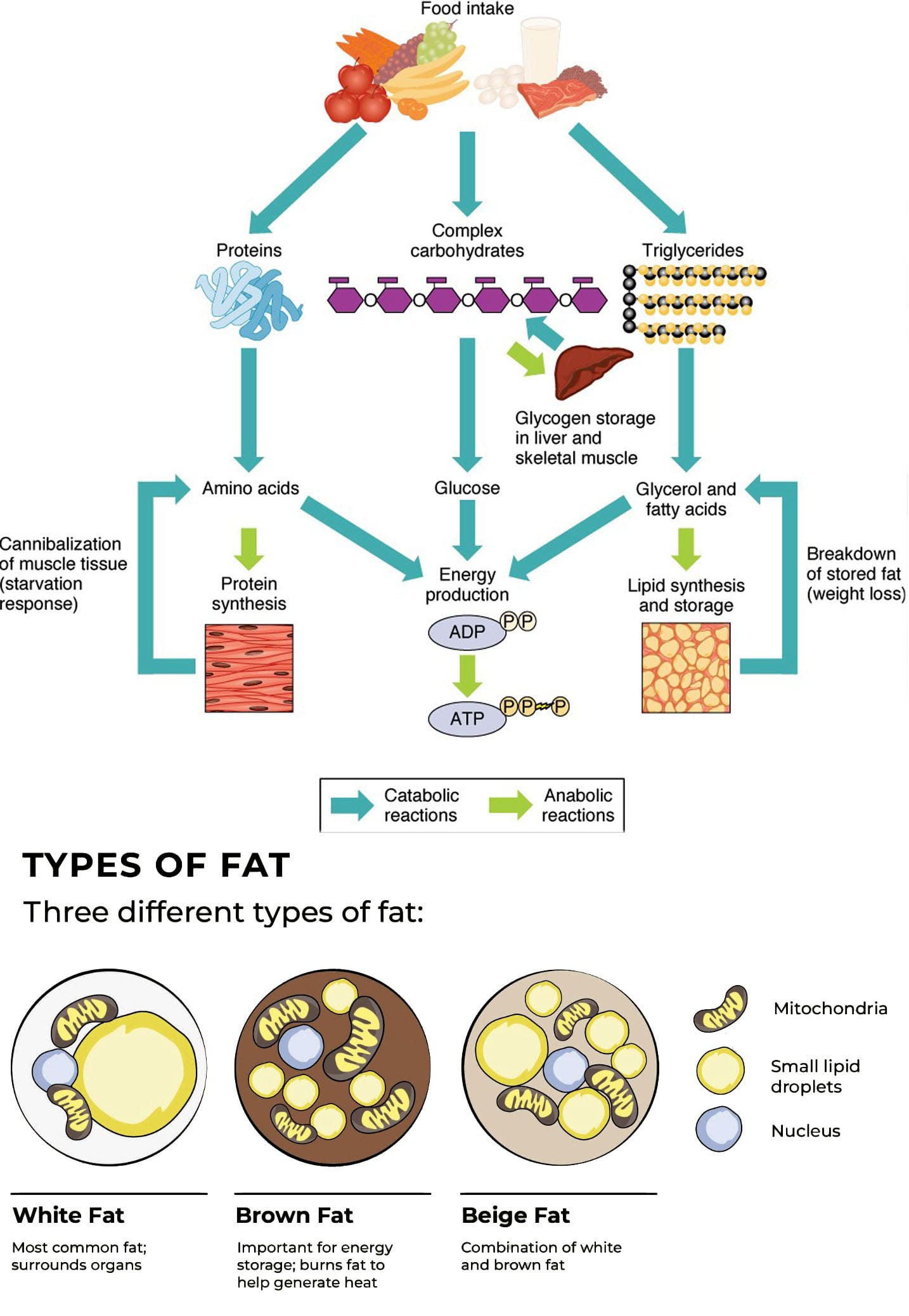
Do you experience an elevated blood sugar level more than usual? Do you experience changes in your heartbeat even though you are walking at a normal pace? Or have you noticed that you are more thirstier than usual? Many people who are experiencing these issues could be dealing with a hormone imbalance. Hormones are chemicals produced and released by specialized cells, many of which are found in endocrine glands. They are released into the bloodstream and affect the target cells’ biochemistry. The presence of hormone receptors, intracellularly in the target cells or on the cell surface, controls hormone activity. Hormones activating the cellular machinery result in higher metabolism, protein synthesis, improved cellular repair, and increased cell formation.

Hormones affect every facet of aging and often decrease with age, resulting in many individuals having a higher hormone dosage to induce a change in cell function. For this very reason, people require ideal hormone levels. Additionally, even if their levels are normal, their bodies still require more hormones to function and feel better. These hormonal shifts impede tissue healing and repair of the body. Hormone shortages and endocrine dysfunction have been linked to the signs and symptoms of aging, as research has now demonstrated that hormone therapy is an effective way to enhance and extend quality of life.
Since aging cannot be stopped, hormones can halt the progression and support by keeping our health in check. Many individuals are trying to find the genetic location that can help regulate aging, and using genetic engineering to modify these genes is necessary for effective age reversal. Regretfully, no technology is currently available to reverse this age through genetic engineering. We must make the most of these changes by incorporating small changes like non-surgical treatments, avoiding risk factors for disease, eating a healthy diet, getting enough exercise, limiting our calorie intake, using antioxidant treatment, and replacing hormones at ideal levels. Slowing the aging process to have less disease and less degradation can provide a higher quality of life while improving feelings and functioning.
What Are Biologically Identical Hormones?
There is no structural difference between the hormone found naturally in the body and the natural hormone. Natural or bioidentical chemicals are not patentable to pharmaceutical corporations since they can patent very profitable chemically distinct compounds. A pharmaceutical company’s exclusive right to produce and profit from its product is ensured by a patent. While it makes sense that pharmaceutical corporations would want their investment protected with a unique, patented product after the enormous financial commitment that goes into researching and creating a pharmaceutical product. Natural hormones need to be better researched and marketed.
Teaching doctors how and when to administer a medication is a significant component of drug marketing. Physicians learn a great deal about medications from pharmaceutical corporations that are actively pushing their products. Since pharmaceutical firms do not produce natural hormones, most doctors only know them once they conduct independent studies on when they originate naturally. Either plants are used to extract the pure physiologically similar (human identical) hormone, or it is synthesized. The most crucial factor is that the final output should be a molecule like a hormone molecule the body naturally produces, which includes DHEA, progesterone, estrogen, thyroid, and progesterone.
Where can natural hormone prescriptions be filled? Many compounding pharmacies are a particular kind of pharmacy that are legitimate, licensed pharmacies can supply individuals with any medication from pharmaceutical manufacturers and are more capable. The traditional image of a pharmacy is that of using a motor and pestle, compared to a compounding pharmacist. They obtain pure pharmaceutical-grade hormones and mix them according to the doctor’s orders. The prescription for dosage and form varies for individuals in tablets, capsules, liquids, and lotions.
Many products in health food stores offer a range of natural solutions, typically derived from plants or herbs. People are turning more and more to herbalists, naturopaths, and folk medicine as alternatives to synthetic, conventional medications. Nevertheless, many compounding pharmacies offer unique products in a few different ways. Initially, a prescription is needed for a pharmacy’s medication, and products from health food stores typically have dosages so low that no prescription is required. According to lab tests, the dosage is normally so low that it is insufficient to cause a discernible change in the body. Second, the compounding pharmacy uses micronized, pure medicinal-grade components in its goods. When a product is micronized, it is a fine grain that absorbs readily. Third, long-acting or time-release prescriptions are available for the natural hormones from the compounding pharmacy. This helps the body avoid the highs and lows associated with rapidly acting, rapidly absorbed, or poorly absorbed goods and instead allows the body to have more balanced hormone levels. A compounding pharmacy offers various possibilities for customized hormone treatment. It even creates a single prescription from personalized dosages, lactose-free fillers, and administration methods such as sublingual triturates, pills, capsules, liquids, and creams. The hormone levels are evaluated and then regulated to maintain ideal amounts of each hormone to ensure appropriate replenishment. If HRT is monitored and adjusted, it may be useful.
Optimize Your Wellness-Video
Hormone Replacement Therapy & Aging
Age causes a decrease in hormones in all people, from young and old. Many doctors believe that this is how things should naturally be. So when a younger person and an older person have hormone deficiencies, the younger individual would be promptly treated if detected with them, and the older individual is not. The term “normal” is relative; even though this low level is barely 20% of a 30-year-old’s level, labs describe it as “normal” even though many individuals do not want the hormone levels of an 80-year-old. Global research teams have now demonstrated that the age-related hormonal deficit should be replaced with a younger person’s hormone levels. Patients enthusiastically welcomed the improvement as soon as they could see and feel it. The damage that the absence of these hormones is causing to the body is realized once one tries this new therapy and feels the dramatically boosted vitality. Its health benefits are an additional bonus.
While progesterone, estrogen, and thyroid have long been administered, effective hormone replacement is a relatively recent development. Instead of maintaining lower or mid-normal levels, it has become a reasonable therapy to replace and balance all hormones simultaneously to an ideal physiological level. This is because when many individuals start to try out hormone replacement therapy, it can provide anti-inflammatory effects and regulate pathogenesis issues that are affecting the body. (Weare-Regales et al., 2022) This distinguishes the best possible hormone replacement from conventional medical treatment. Thankfully, many medical professionals and patients can understand the idea of perfect hormone replacement. With many doctors utilizing HRT training programs, the science underlying this new preventative medicine is reaching a wider audience of physicians.
Numerous aging-related changes, such as osteoporosis, muscle atrophy, sleep disturbances, and decreased sociability, have been demonstrated to be partially brought on by a drop in hormones. Some of the symptoms include reduced protein synthesis in the body, decreased lean body and bone mass, and increased body fat, which are all linked to human aging. The gradual decrease in hormone secretion is commensurate with the changes in body composition. It has been demonstrated that these age-related alterations can be lessened by replenishing these hormones to physiological levels, which are ideal but within reasonable bounds and not excessive. Our hormones’ inability to maintain the equilibrium they once did is a major contributing factor to many aging problems. The disorders like diabetes, heart disease, and hypertension that have come to be associated with normal aging are mostly caused by an imbalance in the proper balance of hormone levels. Immunity is restored by reestablishing the right hormone balance, which can fend against many age-related illnesses.
In conclusion, studies have demonstrated that a decrease in hormone levels can cause aging-related disorders, and the only treatment available at this time to address these symptoms is hormone replacement therapy. Numerous recently published publications about hormone replacement therapy are replete with patient endorsements of the treatment’s advantages. Many patients are middle-aged, healthy, normal persons who have gradually developed symptoms like low energy, low feelings of well-being, lethargy, and loss of interest in routine daily activities. Patients often have weak skin and hair, lose muscular tone, and develop fat around their midsections. Apart from the observable degenerative issues, they will also have elevated cholesterol levels, indications of heart disease, and arthritic changes. Patients have reported transformed bodies, fat disappearing, enhanced muscular tone, and youthful vigor within six to twelve months of starting hormone replacement therapy. Patients report feeling better about themselves and having a more positive attitude. There are amazing feel-good effects as well as fantastic health benefits.
Regretfully, around 90% of patients who come to us from other doctors taking “natural hormones” are not following a proper regimen. How are we aware? The blood levels are almost nil when we measure them. For a younger person, the blood hormone levels must be maintained within the ideal upper limit of normal values for the hormones to have therapeutic effects. The majority of doctors need to be educated to aim for optimal outcomes.
Many doctors need to learn how to prescribe the right amounts. They are unaware of the ideal levels based on blood tests—not saliva tests. They may not know that there are numerous ways to synthesize a natural hormone so that the patient can receive a form that is absorbed and processed in their own way.
To ensure that the therapy yields the greatest possible benefit, the patient must first and foremost urge the doctor to explain, monitor, and optimize the hormone levels. Menopausal women experience significant changes in their skin’s thickness, texture, and tightness from dehydration. The same unsettling changes are noticed by women who discontinue hormone medication. This is because many women who have started on hormone therapy can begin to see relief in their vasomotor symptoms, improve cardioprotection, and prevent other chronic diseases from developing over time. (Shufelt & Manson, 2021) Research published in journals dedicated to dermatology shows that the loss of thyroid, estrogen, and testosterone hormones causes this harmful effect on the skin. Hormone replacement therapy is the only effective treatment for and defense against changes in skin elastin and collagen and wrinkle prevention. The internal alterations, however, are more significant. Not only does the skin on the outside show obvious indications of aging, but there is also noticeable internal degradation. This could cause widespread complaints made by men and women in their midlife about not feeling as good as they would want. If taken care of early on, much of this can be helped. Rather than being afraid of how much you’ve aged, you’d rather hear, “Wow, you look great!” at that high school reunion.
Thyroid Hormones
The thyroid gland secretes thyroid hormone, a metabolic hormone that helps regulate temperature, metabolism, and brain function in the body. Thyroid hormones are crucial for normal development in the body and are necessary for normal physiological functioning. (Babic Leko et al., 2021) The thyroid also lowers cholesterol and promotes weight loss by increasing fat breakdown, protecting against cardiovascular illnesses, avoiding cognitive deterioration, and enhancing cerebral metabolism. When environmental factors affect the thyroid, it can lead to overlapping risk profiles in the body.
Low thyroid function is associated with low levels of energy and exhaustion, slowness of thought and movement, depression, forgetfulness, mental disorientation, discomfort similar to that of arthritis, and an increased risk of infections and colds. Many of these features are thought to be typical of aging; however, many individuals will begin to notice that thyroid deficiency is the secondary cause. As we get older, our thyroid produces fewer hormones. So, regulating the hormone function in the body starts with the thyroid hormone. This is now understood to be thyroid insufficiency rather than actual hypothyroidism, which in the past was believed to necessitate hormone replacement therapy. Hypothyroidism occurs when the thyroid gland has inadequate hormone production, which causes nonspecific signs and symptoms and develops overlapping risk profiles that affect the body’s metabolism and function of many cells and vital organs. (Wilson et al., 2021) According to numerous research studies, raising thyroid levels can help the body system work more effectively and efficiently while relieving many symptoms associated with thyroid insufficiency.
Estrogen
Doctors have been giving estrogen for menopausal symptoms, including sleeplessness and hot flashes, to women for almost 40 years. Many ladies used estrogen for as long as they could because they felt so healthy and energized when taking it. Numerous studies witness estrogen’s remarkable impact on women’s health and well-being. A woman’s quality of life is greatly enhanced by estrogen, which makes them feel more youthful and invigorated. After menopause, women have more pleasurable, fulfilling sex lives, stronger, glossier hair, and greater muscle tone. Users of estrogen do not have the usual osteoporosis-related bone loss and instead stand taller and straighter. This is because even though estrogen’s main goal is to ascribe reproduction, it can help target non-reproductive tissues like skeletal muscle. (Critchlow et al., 2023) Those who utilize estrogen have a 50% lower risk of heart disease and stroke than those who do not. Alzheimer’s dementia and senility are incredibly rare among estrogen users. Users of estrogen are not susceptible to the potentially crippling conditions of urogenital atrophy, vaginal dryness, and concurrent infections. One of the few hormones that women ask their doctors for is estrogen. Estrogen was the most commonly prescribed medication in the U.S., with over 10 million women taking it. We have discovered the benefits of proper hormone supplementation and the synergy that results from restoring all hormone levels through estrogen supplementation.
In the past, doctors frequently performed hysterectomy, which involved removing a woman’s ovaries. This stopped the manufacturing of important hormones. Doctors now attempt to save ovaries wherever possible after realizing the pain and negative consequences of hormone loss. We would remove ovaries surgically at a young age if hormones were that bad. Rather, we aim to maintain ovarian function and the production of healthy hormones for as long as possible. Instead of using a whole separate hormone with a different molecular structure, we need to employ the same hormone to restore the lost hormones to pre-menopausal levels when menopause occurs and hormone levels drop. The human body is aware of a difference, even though the pharmaceutical business denies it.
The adrenal glands and ovaries both create estrogen. Men do produce a very tiny amount of estrogen through the conversion of testosterone. The body of a woman contains three different forms of estrogen. They are estriol, estradiol, and estrone. The symptoms and negative health effects of menopause are caused by a sharp decline in the levels of all these hormones at the beginning of menopause. Menopause symptoms include anxiety, vaginal dryness, hot flashes, sleeplessness, bladder issues, and trouble focusing. Unfortunately, the lack of estrogen makes the disease processes—such as Alzheimer’s, osteoporosis, stroke, and cardiovascular disease—worse. Incorporating hormone replacement therapy to replenish estrogen levels for females can ultimately enhance their reproductive health and overall well-being. (Moustakli & Tsonis, 2023)
Progesterone
Pro-gestational, or progesterone, is vitally essential for the onset and maintenance of pregnancy. Progesterone, which guards against osteoporosis, heart disease, breast cancer, and uterine cancer, is lost by women going through menopause. Regretfully, most clinicians utilize medroxyprogesterone, or Provera, a synthetic, chemically distinct medication, rather than progesterone to replace the lost progesterone. Despite having the same name as progesterone (medroxyprogesterone), Provera differs from progesterone in molecular and biological ways. This section discusses why progesterone is so safe and helpful and why Provera is so damaging, even though most doctors believe they are interchangeable.
Despite being disregarded frequently, progesterone is another female hormone that is just as important for aging women as estrogen. The ovaries create the hormone progesterone, which the body uses to balance estrogen. Additionally, progesterone can prevent numerous chronic conditions like osteoporosis and cancer, alleviate menopausal symptoms, and enhance general health. Doctors have historically been used to prescribing the synthetic progestin, which is marketed under the name Provera. These synthetic progestins lack the advantages of natural progesterone and have the same serious side effects and issues as synthetic estrogens. This is because hormones like progesterone and estrogen play a different role in any pain-related conditions that can affect anyone. (Athnaiel et al., 2023) More significantly, new research continuously shows that progesterone prevents breast cancer.
Since the two hormones were designed to cooperate to preserve a healthy hormonal balance, natural progesterone can amplify the effects of estrogen. When a person is dealing with low progesterone, it can bring on similar illness processes as low estrogen. These include heart disease, osteoporosis, a decline in libido, and a markedly reduced quality of life. Natural progesterone and estrogen can stop this downward spiral by maintaining women’s vitality, strength, and health.
Additionally, natural progesterone raises HCL, or good cholesterol, and lowers cholesterol levels more. Synthetic progestin, on the other hand, has the opposite effect. Regrettably, many doctors who prescribe progestin are ignorant of the existence of a safer, more well-tolerated alternative. Furthermore, it has been demonstrated that natural progesterone can stop the advancement of osteoporosis by stimulating osteoblasts. These cells produce new bones, while only estrogen can prevent bone loss.
Conclusion
Overall, it is important to replenish lost hormones in the body by reducing numerous environmental factors that can enhance the overlapping risk profiles that cause pain and discomfort. When many start thinking about their health, they can make small changes in their habits like eating right, utilizing non-surgical treatments, exercising, and being mindful of their stress to live healthier lives. In part 2, we will explore hormone therapy and its beneficial properties more in-depth.
References
Athnaiel, O., Cantillo, S., Paredes, S., & Knezevic, N. N. (2023). The Role of Sex Hormones in Pain-Related Conditions. Int J Mol Sci, 24(3). https://doi.org/10.3390/ijms24031866
Babic Leko, M., Gunjaca, I., Pleic, N., & Zemunik, T. (2021). Environmental Factors Affecting Thyroid-Stimulating Hormone and Thyroid Hormone Levels. Int J Mol Sci, 22(12). https://doi.org/10.3390/ijms22126521
Critchlow, A. J., Hiam, D., Williams, R., Scott, D., & Lamon, S. (2023). The role of estrogen in female skeletal muscle aging: A systematic review. Maturitas, 178, 107844. https://doi.org/10.1016/j.maturitas.2023.107844
Moustakli, E., & Tsonis, O. (2023). Exploring Hormone Therapy Effects on Reproduction and Health in Transgender Individuals. Medicina (Kaunas, Lithuania), 59(12). https://doi.org/10.3390/medicina59122094
Shufelt, C. L., & Manson, J. E. (2021). Menopausal Hormone Therapy and Cardiovascular Disease: The Role of Formulation, Dose, and Route of Delivery. J Clin Endocrinol Metab, 106(5), 1245-1254. https://doi.org/10.1210/clinem/dgab042
Weare-Regales, N., Chiarella, S. E., Cardet, J. C., Prakash, Y. S., & Lockey, R. F. (2022). Hormonal Effects on Asthma, Rhinitis, and Eczema. J Allergy Clin Immunol Pract, 10(8), 2066-2073. https://doi.org/10.1016/j.jaip.2022.04.002
Wilson, S. A., Stem, L. A., & Bruehlman, R. D. (2021). Hypothyroidism: Diagnosis and Treatment. American Family Physician, 103(10), 605-613. https://www.ncbi.nlm.nih.gov/pubmed/33983002
https://www.aafp.org/pubs/afp/issues/2021/0515/p605.pdf
Disclaimer