For individuals looking to improve their fitness health, can a fitness assessment test identify potential areas and help evaluate overall health and physical status?

Table of Contents
Fitness Assessment
A fitness test, also known as a fitness assessment, helps evaluate an individual’s overall and physical health. It comprises a series of exercises to design an appropriate exercise program for general health and fitness. (National Strength and Conditioning Association. 2017) Fitness assessment testing benefits include:
- Identifying areas that need improvement.
- Assisting professionals in understanding what types of exercise are safest and most effective.
- Helping measure fitness progress over time.
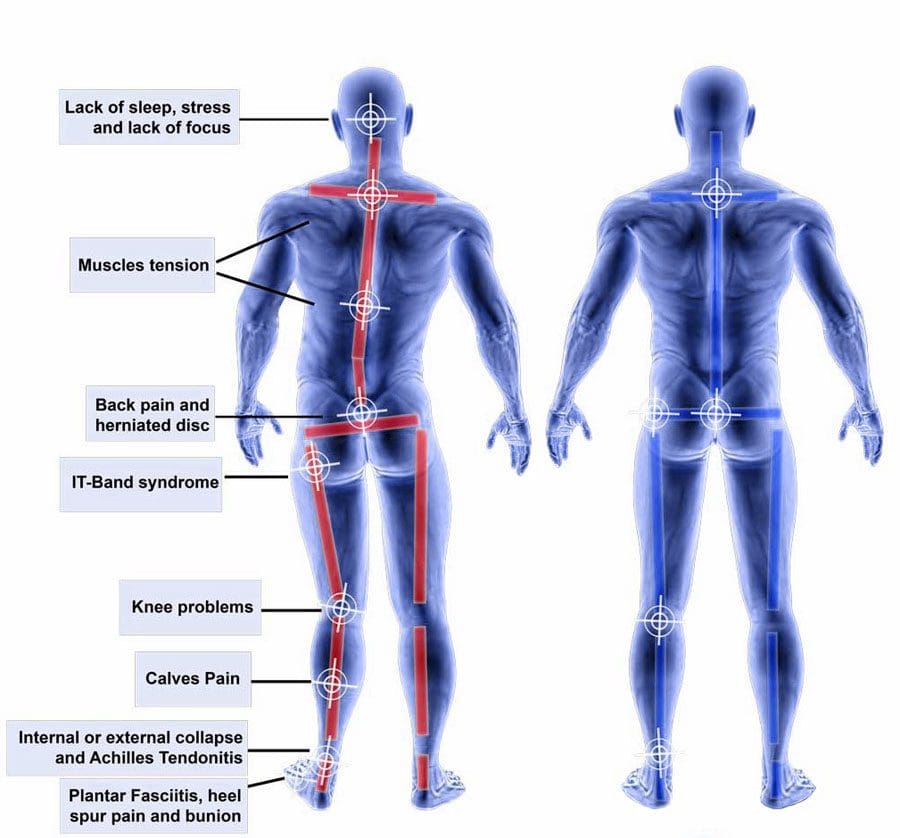
- Allowing for an individualized plan that can help prevent injuries and maintain the body’s overall health.
An assessment can comprise a wide range of tests, including:
- Body composition tests.
- Cardiovascular stress tests.
- Endurance tests.
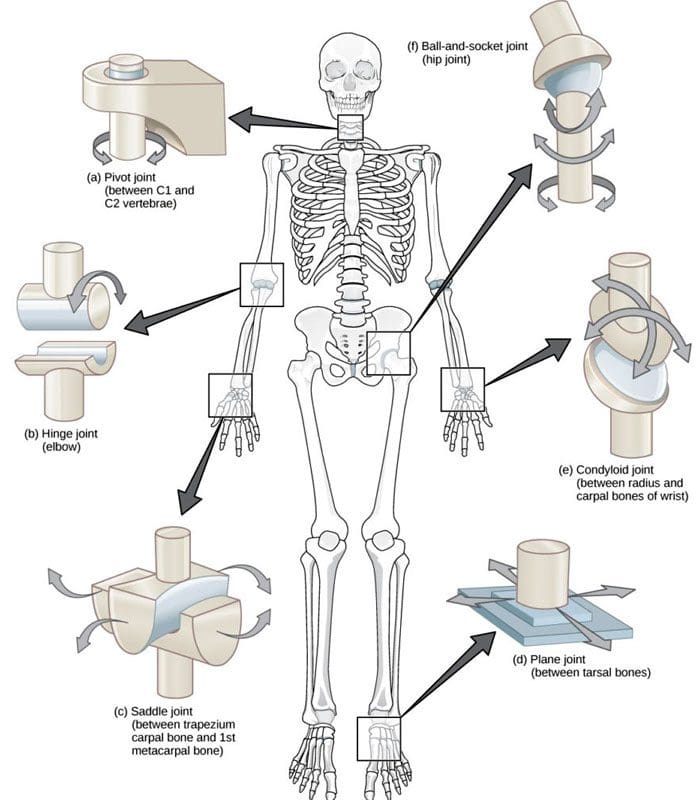
- Range of motion tests.
They are meant to ensure the individual won’t be at risk of injury and provide the trainer with the insights needed to establish clear and effective fitness goals. Individuals who wonder whether fitness testing would benefit them should consult their healthcare provider.
General Health
Before starting a fitness program, it is important to inform the trainer of individual medical history and get the necessary approval from a primary healthcare provider. (Harvard Health Publishing. Harvard Medical School. 2012) Fitness specialists usually use one or more screening tools to help determine individual baseline health.
This may include obtaining vital sign measurements like height and weight, resting heart rate/RHR, and resting blood pressure/RBP. Many trainers will also use a physical activity readiness questionnaire/PAR-Q comprising questions about general health. (National Academy of Sports Medicine. 2020) Among the questions, individuals may be asked about the medications being taken, any problems with dizziness or pain, or medical conditions that may impair their ability to exercise.
Body Composition
Body composition describes total body weight components, including muscles, bones, and fat. The most common methods for estimating body composition include:
Bioelectrical Impedance Analysis – BIA
- During BIA, electrical signals are sent from electrodes through the soles of the feet to the abdomen to estimate body composition. (Doylestown Health. 2024)
Body Mass Index – BMI
- BMI is a generalized calculation of body fat based on height and weight. (National Heart, Lung, and Blood Institute. N.D.)
Skinfold Measurements
- These measurements use calipers to estimate the amount of body fat in a fold of skin.
Cardiovascular Endurance
Cardiovascular endurance testing, also known as stress testing, measures how efficiently the heart and lungs work to supply oxygen and energy to the body during physical activity. (UC Davis Health, 2024) The three most common tests used include:
12-minute Run Tests
- Twelve-minute run tests are performed on a treadmill, and an individual’s pre-exercise heart and respiration rates are compared with post-exercise heart and respiration rates.
Exercise Stress
- Exercise stress testing is performed on a treadmill or stationary bike.
- It involves using a heart monitor and blood pressure cuff to measure vital signs during exercise.
VO2 Max Testing
- Performed on a treadmill or stationary bike.
- V02 max testing uses a breathing device to measure the maximum rate of oxygen consumption during physical activity (UC Davis Health, 2024)
- Some trainers will incorporate exercises like sit-ups or push-ups to measure response to specific exercises.
- These baseline results can be used later to see if health and fitness levels have improved.
Strength and Endurance
Muscle endurance testing measures the length of time a muscle group can contract and release before it fatigues. Strength testing measures the maximal amount of force a muscle group can exert. (American Council on Exercise, Jiminez C., 2018) The exercises used include:
- The push-up test.
- Core strength and stability test.
Sometimes, a trainer will use a metronome to measure how long the individual can keep up with the rhythm. The results are then compared to individuals of the same age group and sex to establish a baseline level. Strength and endurance tests are valuable as they help the trainer spot which muscle groups are stronger, vulnerable, and need focused attention. (Heyward, V. H., Gibson, A. L. 2014).
Flexibility
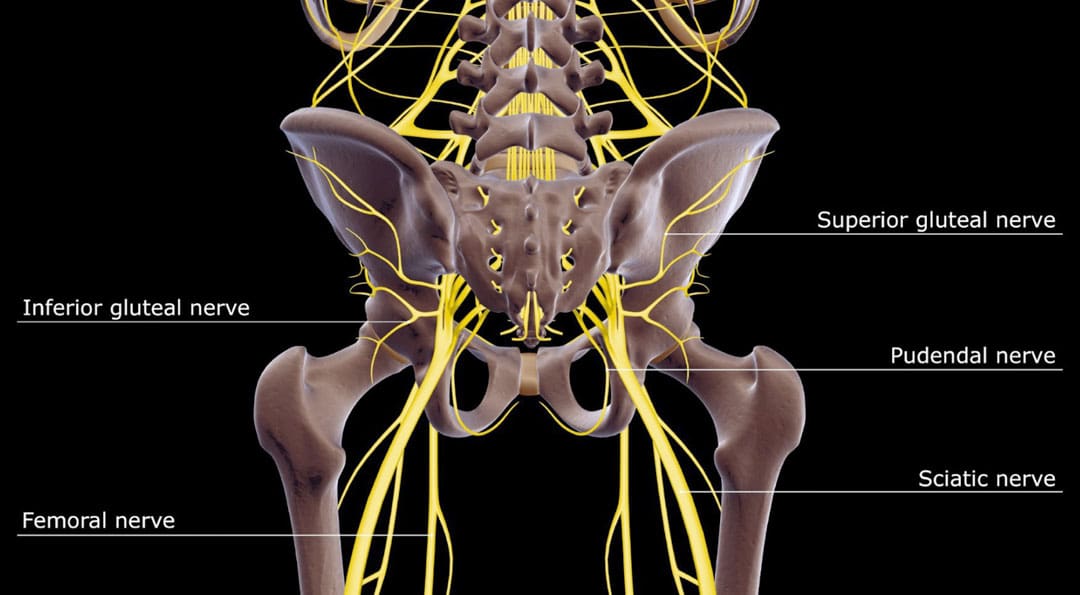
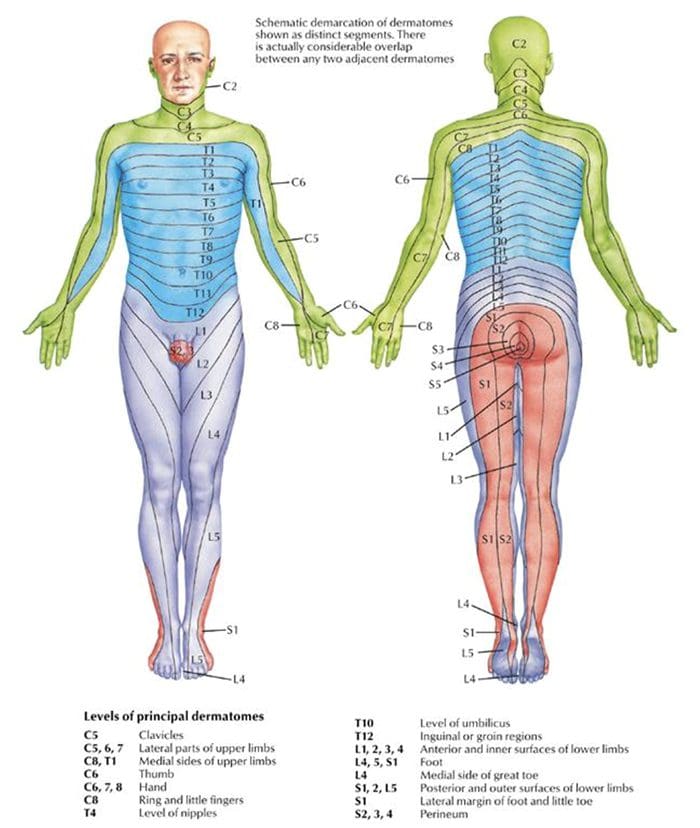
- Measuring the flexibility of joints is vital in determining whether individuals have postural imbalances, foot instability, or limitations in range of motion. (Pate R, Oria M, Pillsbury L, 2012)
Shoulder Flexibility
- Shoulder flexibility testing evaluates the flexibility and mobility of the shoulder joint.
- It is performed by using one hand to reach behind the neck, between the shoulders, and the other hand to reach behind the back, toward the shoulders, to measure how far apart the hands are. (Baumgartner TA, PhD, Jackson AS, PhD et al., 2015)
Sit-And-Reach
- This test measures tightness in the lower back and hamstring muscles. (American Council of Exercise, Metcalf A. 2014)
- The sit-and-reach test is performed on the floor with the legs fully extended.
- Flexibility is measured by how many inches the hands are from the feet when reaching forward.
Trunk Lift
- Trunk lift testing is used to measure tightness in the lower back.
- It is performed while lying face-down on the floor with arms at your side.
- The individual will be asked to lift their upper body with just the back muscles.
- Flexibility is measured by how many inches the individual can lift themselves off the ground. (Baumgartner TA, PhD, Jackson AS, PhD et al., 2015)
Fitness assessment testing has various benefits. It can help trainers design a personalized workout program, help individuals identify fitness areas that need improvement, measure progress, and add intensity and endurance to their routine, which can help prevent injuries and help maintain overall health. We focus on what works for you and strive to better the body through researched methods and total wellness programs. These natural programs use the body’s ability to achieve improvement goals. Ask a healthcare professional or fitness professional for guidance if you need advice.
PUSH Fitness
References
National Strength and Conditioning Association. (2017). Purposes of assessment. www.nsca.com/education/articles/kinetic-select/purposes-of-assessment/
Harvard Health Publishing. Harvard Medical School. (2012). Do you need to see a doctor before starting your exercise program? HealthBeat. www.health.harvard.edu/healthbeat/do-you-need-to-see-a-doctor-before-starting-your-exercise-program
National Academy of Sports Medicine. (2020). PAR-Q-+ The Physical Activity Readiness Questionnaire for Everyone. www.nasm.org/docs/pdf/parqplus-2020.pdf?sfvrsn=401bf1af_24
Doylestown Health. (2024). Bio-Electrical Impedance Analysis (BIA)-Body Mass Analysis. www.doylestownhealth.org/service-lines/nutrition#maintabbed-content-tab-2BDAD9F8-F379-403C-8C9C-75D7BFA6E596-1-1
National Heart, Lung, and Blood Institute. U.S. Department of Health and Human Services. (N.D.). Calculate your body mass index. Retrieved from www.nhlbi.nih.gov/health/educational/lose_wt/BMI/bmicalc.htm
UC Davis Health. (2024). VO2max and Aerobic Fitness. health.ucdavis.edu/sports-medicine/resources/vo2description
American Council on Exercise. Jiminez C. (2018). Understanding 1-RM and Predicted 1-RM Assessments. ACE Fitness. www.acefitness.org/fitness-certifications/ace-answers/exam-preparation-blog/2894/understanding-1-rm-and-predicted-1-rm-assessments/
Heyward, V. H., Gibson, A. L. (2014). Advanced Fitness Assessment and Exercise Prescription. United Kingdom: Human Kinetics. www.google.com/books/edition/Advanced_Fitness_Assessment_and_Exercise/PkdoAwAAQBAJhl=en&gbpv=1&dq=Strength+and+endurance+tests+muscle+groups+are+stronger+and+weaker&pg=PA173&printsec=frontcover#v=onepage&q=Strength%20and%20endurance%20tests%20muscle%20groups%20are%20stronger%20and%20weaker&f=false
Pate R, Oria M, Pillsbury L, (Eds). (2012). Health-related fitness measures for youth: Flexibility. In R. Pate, M. Oria, & L. Pillsbury (Eds.), Fitness Measures and Health Outcomes in Youth. doi.org/10.17226/13483
Baumgartner, T. A., Jackson, A. S., Mahar, M. T., Rowe, D. A. (2015). Measurement for Evaluation in Kinesiology. United States: Jones & Bartlett Learning. www.google.com/books/edition/Measurement_for_Evaluation_in_Kinesiolog/_oCHCgAAQBAJ?hl=en&gbpv=1&dq=Measurement+for+Evaluation+in+Kinesiology+(9th+Edition).&printsec=frontcover#v=onepage&q&f=false
American Council of Exercise. Metcalf A. (2014). How to improve flexibility and maintain it. ACE Fitness. www.acefitness.org/resources/everyone/blog/3761/how-to-improve-flexibility-and-maintain-it/


























 Shoe Types and Their Impact on The Back
Shoe Types and Their Impact on The Back

 Ability
Ability


