Discover the connection between auto accidents and injuries like whiplash and Achilles tendinosis. Find insights and solutions.
Table of Contents
Introduction: The Impact of Whiplash and Ligamentous Injuries
Picture this: you’re driving along, singing to your favorite tune, when—bam!—a car rear-ends you. Your head snaps back and forth like a bobblehead on a bumpy road. Welcome to the world of whiplash, a not-so-fun injury that’s all too common in motor vehicle accidents (MVAs). Whiplash doesn’t just make your neck feel like it’s auditioning for a stiff role in a movie; it can cause serious damage to the ligaments in your neck and upper body, leading to pain that lingers like an unwanted guest.
Ligamentous injuries, particularly those from whiplash, are a big deal because they can affect your daily life, from turning your head to picking up your groceries. In El Paso, Texas, Dr. Alexander Jimenez, a chiropractor and board-certified family nurse practitioner, is a go-to expert for helping MVA victims recover. With over 25 years of experience, he combines advanced diagnostics with personalized treatments to help patients recover and supports them in personal injury cases with detailed medical reports. In this guide, we’ll explore what ligaments are, how they can be injured in motor vehicle accidents (MVAs), the symptoms and treatments, and why Dr. Jimenez is a trusted name in El Paso for those navigating the aftermath of a crash.
References
- Croft, A. C. (n.d.). Croft Whiplash Guidelines. Colorado Chiropractic Association.
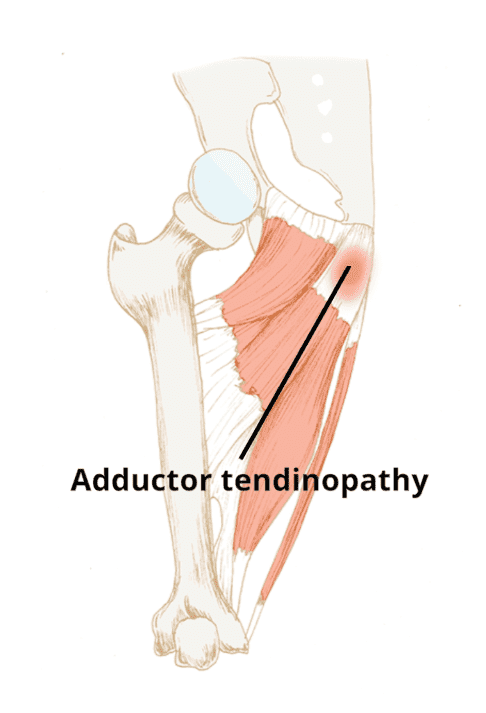
- Jimenez, A. (2016, June). Similarities between whiplash and Achilles tendonosis. El Paso Chiropractor Blog.
Understanding Ligaments: The Body’s Natural Duct Tape
Ligaments are like the duct tape of your body—tough, fibrous bands that hold your bones together and keep your joints from going rogue. Made up of about 75% collagen (type I), two-thirds water, elastin, and other components, ligaments are built to stabilize joints, guide movement, and provide proprioception (your body’s sense of where it is in space). In the upper body, they’re critical in areas like the cervical spine (neck), shoulders, elbows, and wrists, ensuring everything moves smoothly without falling apart.
Think of ligaments as the unsung heroes working behind the scenes. They’re not as flashy as muscles, but without them, your skeleton would be a wobbly mess. Their mechanical properties, such as viscoelasticity (the ability to stretch and return to their original shape), allow them to absorb energy during impacts, but they have limits. When an MVA pushes them beyond those limits, you’re in for a world of hurt.
References
- Jimenez, A. (n.d.). Musculoskeletal ligaments: What to know after a car accident. Sciatica Clinic.
Mechanisms of Injury in Motor Vehicle Accidents
So, how do ligaments get injured in MVAs? Imagine your car as a roller coaster, and your body as the rider who didn’t sign up for the ride. The sudden force of a collision—whether it’s a rear-end hit, side-impact, or frontal crash—can stretch or tear ligaments. Whiplash, which affects 83% of people in rear-end collisions, is the star of this painful show (Barnsley et al., 1994). The rapid back-and-forth motion of the head overstretches neck ligaments, such as the anterior longitudinal ligament, leading to sprains or even complete tears.
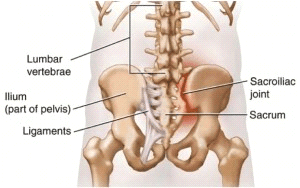
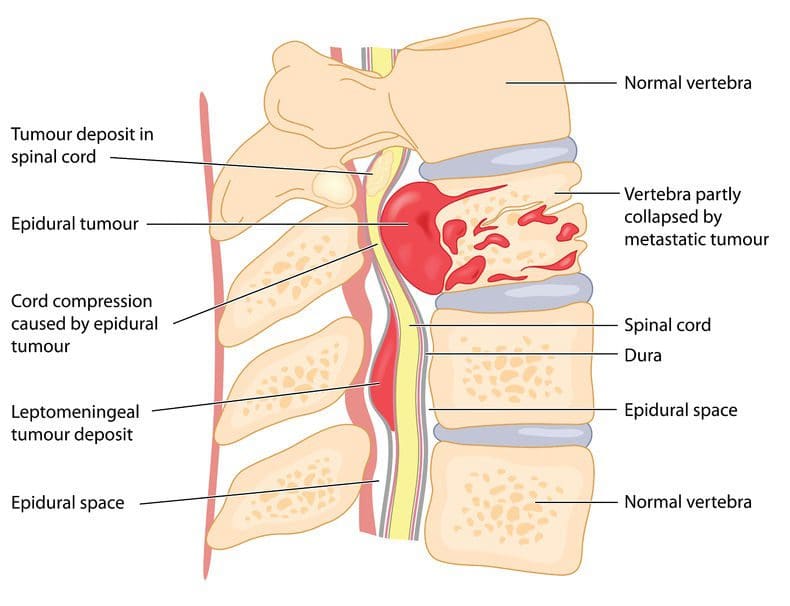
Other types of collisions can also cause significant damage. Side-impact crashes might damage shoulder ligaments, while rollovers can affect multiple areas. The biomechanics are brutal: rapid velocity changes create shearing forces that ligaments simply can’t handle, potentially disrupting spinal alignment and compressing nerves, which can lead to conditions like sciatica.
References
- Jimenez, A. (n.d.). Ligamentous injuries: Insights from an expert. Sciatica Clinic.
The Root Causes of Pain- Video

Grades of Severity and Stages of Injury
Not all whiplash injuries are created equal. The Croft Whiplash Guidelines classify cervical acceleration/deceleration (CAD) trauma into five grades, each with different symptoms and treatment needs:
| Grade | Severity | Symptoms | Treatment Duration | Treatment Number |
|---|---|---|---|---|
| I | Minimal | No range of motion limitation, no ligamentous injury, no neurological symptoms | Up to 10 weeks | Up to 21 visits |
| II | Slight | Limited range of motion, no ligamentous injury, no neurological findings | Up to 29 weeks | Up to 33 visits |
| III | Moderate | Limited range of motion, some ligamentous injury, neurological findings | Up to 56 weeks | Up to 76 visits |
| IV | Moderate to Severe | Limited motion, ligamentous instability, neurological findings, fracture, or disc issues | May require permanent care | Varies |
| V | Severe | Requires surgical treatment and stabilization | Post-surgical chiropractic care | Varies |
The healing process also follows distinct stages:
- Stage I (Acute Inflammatory): 0-72 hours, marked by swelling and pain.
- Stage II (Repair): 72 hours to 14 weeks, where the body starts rebuilding tissue.
- Stage III (Remodeling): 14 weeks to 12 months or more, as tissues strengthen.
- Stage IV (Chronic): Permanent changes if healing is incomplete.
Factors such as age, prior injuries, or underlying conditions like arthritis can complicate recovery, making personalized care essential.
References
- Croft, A. C. (n.d.). Croft Whiplash Guidelines. Colorado Chiropractic Association.
Clinical Presentation and Diagnosis
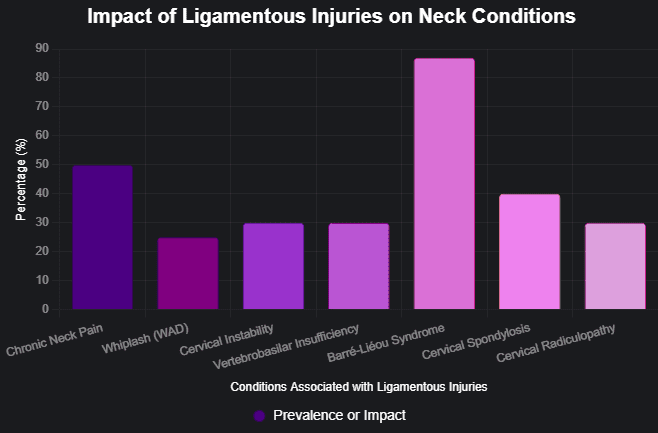
Ligamentous injuries are sneaky—like ninjas, they can cause trouble without being immediately obvious. Symptoms include pain, stiffness, swelling, reduced range of motion, and occasionally neurological issues such as tingling or radiating pain. In severe cases, these injuries can lead to chronic neck or back pain, or even sciatica, where pain shoots down the leg due to nerve compression.
Diagnosing these injuries isn’t always straightforward. Standard X-rays may miss ligament damage, so advanced imaging techniques like MRI, CT, or dynamic X-rays are often necessary. Dr. Alexander Jimenez utilizes these tools, along with electromyography (EMG), to precisely assess the extent of the injury. His dual expertise as a chiropractor and nurse practitioner allows him to interpret these diagnostics with precision, ensuring patients get the right treatment plan.
References
- Jimenez, A. (n.d.). Ligamentous injuries and chronic neck pain: Causes and effects. Sciatica Clinic.
Treatment Protocols and Rehabilitation
Treating ligamentous injuries is like fixing a car after a crash—you need the right tools and a skilled mechanic. For mild injuries (Grade I or II), conservative treatments such as rest, ice, compression, and elevation (RICE), combined with physical therapy, can be highly effective. Chiropractic adjustments, soft tissue therapies, and massages help restore mobility and reduce pain. For more severe cases (Grade III or IV), advanced interventions, such as corticosteroid injections or regenerative therapies like platelet-rich plasma (PRP), may be necessary. Grade V injuries often require surgical stabilization, followed by chiropractic care.
Dr. Jimenez’s approach is comprehensive, combining chiropractic adjustments with physical therapy, core strengthening, and postural training. Early intervention is key to preventing chronic pain, and his clinic emphasizes rehabilitation to restore function and prevent recurrence. For example, a patient with a Grade II whiplash injury might start with daily treatments for a week, then taper to weekly sessions over several months, as outlined in the Croft Guidelines.
References
- Croft, A. C. (n.d.). Croft Whiplash Guidelines. Colorado Chiropractic Association.
- Jimenez, A. (n.d.). Musculoskeletal ligaments: What to know after a car accident. Sciatica Clinic.
Dr. Alexander Jimenez’s Role in Personal Injury Cases
In El Paso, where MVAs are all too common, Dr. Alexander Jimenez stands out as a beacon of hope for personal injury victims. With dual licensure as a Doctor of Chiropractic (DC) and Family Nurse Practitioner (FNP-BC), he brings a unique perspective to patient care. His clinic, Injury Medical & Chiropractic Clinic, utilizes advanced diagnostics, including MRI, CT, and EMG, to accurately assess injuries. His treatments range from conservative options like chiropractic adjustments to advanced therapies like radiofrequency ablation, tailored to each patient’s needs.
Beyond medical care, Dr. Jimenez plays a critical role in personal injury cases. He provides detailed medical reports that document injuries and treatments, serving as a vital link between healthcare and legal proceedings. These reports help ensure victims receive fair compensation for their injuries. His 25 years of experience and patient-centered approach make him a trusted provider in El Paso, as evidenced by testimonials praising his thorough care.
References
- Jimenez, A. (n.d.). Ligamentous injuries: Insights from an expert. Sciatica Clinic.
- Jimenez, A. (2024). Dr. Alexander Jimenez’s professional profile. LinkedIn.
Conclusion and Disclaimer
Ligamentous injuries from MVAs, particularly whiplash, can have a profound impact on your health and quality of life. Understanding their structure, how they’re injured, and the importance of early treatment is essential for recovery. In El Paso, Dr. Alexander Jimenez offers expert care, combining advanced diagnostics with personalized treatment plans to help patients heal and navigate personal injury claims. His dual expertise ensures comprehensive care, making him a trusted resource for MVA victims.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider for medical concerns related to ligamentous injuries or whiplash.
References
- Croft, A. C. (n.d.). Croft Whiplash Guidelines. Colorado Chiropractic Association.
- Jimenez, A. (2016, June). Similarities between whiplash and Achilles tendonosis. El Paso Chiropractor Blog.
- Jimenez, A. (n.d.). Musculoskeletal ligaments: What to know after a car accident. Sciatica Clinic.
- Jimenez, A. (n.d.). Ligamentous injuries: Insights from an expert. Sciatica Clinic.
- Jimenez, A. (n.d.). Ligamentous injuries and chronic neck pain: Causes and effects. Sciatica Clinic.
Key Citations
- Croft Whiplash Guidelines by Arthur C. Croft
- Similarities between whiplash and Achilles tendonosis by Dr. Jimenez
- Musculoskeletal ligaments: What to know after a car accident
- Ligamentous injuries: Insights from an expert by Dr. Jimenez
- Ligamentous injuries and chronic neck pain: Causes and effects
- Dr. Alexander Jimenez’s professional profile on LinkedIn