Understand the benefits of physical therapy for managing auto injuries and whiplash, focusing on recovery and pain relief.
Car accidents can turn your life upside down faster than you can say “fender bender.” One of the most common injuries from motor vehicle accidents (MVAs) is whiplash, a pesky condition that can make your neck feel like it’s auditioning for a role as a rusty hinge. But don’t worry—there’s a light at the end of the tunnel, and it’s called physical therapy. In this comprehensive guide, we’ll explore why physical therapy is a game-changer for recovering from whiplash, how it works, and why Dr. Alexander Jimenez, a renowned chiropractor and nurse practitioner in El Paso, Texas, is a go-to expert for accident victims. So, buckle up (safely, of course!) as we dive into the world of whiplash recovery with a sprinkle of humor to keep things light.
Table of Contents
Introduction
Imagine this: you’re cruising down the highway, singing along to your favorite song, when bam!—a car rear-ends you. Suddenly, your neck feels like it’s been through a blender. Welcome to the world of whiplash, a common injury from MVAs that affects millions of people each year (Mayo Clinic, 2024). Whiplash happens when your head is suddenly jerked forward and backward, straining the muscles and ligaments in your neck. It’s not just a minor annoyance—it can lead to chronic pain if not treated properly.
That’s where physical therapy comes in, like a superhero swooping in to save the day. Physical therapy helps reduce pain, restore movement, and prevent long-term issues. In El Paso, Texas, Dr. Alexander Jimenez stands out as a leading expert in treating injuries related to motor vehicle accidents (MVAs). With over 30 years of experience as a chiropractor and a board-certified family nurse practitioner, he has helped countless patients return to their normal lives. This blog post will cover what whiplash is, its symptoms, how physical therapy can help, and why Dr. Jimenez is a trusted name in personal injury care. We’ll also throw in some humor to keep you smiling—because recovering from an accident is tough enough!
References
- Mayo Clinic. (2024). Whiplash. Retrieved from https://www.mayoclinic.org/diseases-conditions/whiplash/symptoms-causes/syc-20378919
- Cleveland Clinic. (2022). Whiplash (Neck Strain): What It Is, Symptoms & Treatment. Retrieved from https://my.clevelandclinic.org/health/diseases/11982-whiplash
What is Whiplash?
Whiplash is like your neck’s way of saying, “I didn’t sign up for this rollercoaster!” It’s an injury that occurs when your head is suddenly forced backward and then forward, typically during a rear-end car collision. This rapid motion can stretch or tear the muscles, ligaments, tendons, and even discs in your neck (Cleveland Clinic, 2022). The term “whiplash” comes from the whip-like motion of your head, and trust me, it’s not as fun as it sounds.
While MVAs are the most common cause, whiplash can also occur in sports (such as football tackles) or even on amusement park rides with sudden stops. Surprisingly, you don’t need a high-speed crash to get whiplash—research shows it can occur at speeds as low as 6 mph (Expert Court Reports, 2022). The severity of whiplash is graded from 0 (no symptoms) to 4 (fracture or dislocation), with most cases falling into grades 1 or 2, which involve pain and stiffness but no major structural damage (Physiopedia, n.d.).
Your car’s headrest can be a lifesaver here. If it’s adjusted properly—level with the top of your head and close to your neck—it can reduce the impact. So, next time you’re in the driver’s seat, give your headrest a quick check. It’s like giving your neck a hug before you hit the road.
References
- Cleveland Clinic. (2022). Whiplash (Neck Strain): What It Is, Symptoms & Treatment. Retrieved from https://my.clevelandclinic.org/health/diseases/11982-whiplash
- Physiopedia. (n.d.). Whiplash Associated Disorders. Retrieved from https://www.physio-pedia.com/Whiplash_Associated_Disorders
- Expert Court Reports. (2022). The importance of Physiotherapy after a Road Traffic Accident (RTA). Retrieved from https://www.expertcourtreports.co.uk/blog/the-importance-of-physiotherapy-after-a-road-traffic-accident-rta/
Symptoms of Whiplash
Whiplash symptoms can be as sneaky as a cat burglar. Sometimes they hit you right after the accident, but other times they creep up days or even weeks later. Here’s what you might experience:
- Neck pain and stiffness: Your neck might feel like it’s made of concrete, making it hard to turn your head.
- Headaches: These often start at the base of your skull and can feel like a band tightening around your head.
- Shoulder and upper back pain: The impact can spread discomfort to your shoulders and upper back.
- Arm pain or numbness: If nerves are irritated, you might feel tingling or pain shooting down your arms.
- Dizziness or vertigo: This can occur if the accident affects your balance sensors.
- Cognitive issues: Some individuals report experiencing “whiplash brain,” characterized by trouble focusing or remembering things.
- Sleep problems: Pain can keep you tossing and turning all night.
- Visual disturbances: Blurred vision or light sensitivity may also occur.
Because symptoms can be delayed, it’s smart to see a doctor even if you feel okay after a crash. Ignoring whiplash is like ignoring a check engine light—it might seem fine now, but trouble could be brewing (Mayo Clinic, 2024).
References
- Mayo Clinic. (2024). Whiplash. Retrieved from https://www.mayoclinic.org/diseases-conditions/whiplash/symptoms-causes/syc-20378919
- Cleveland Clinic. (2022). Whiplash (Neck Strain): What It Is, Symptoms & Treatment. Retrieved from https://my.clevelandclinic.org/health/diseases/11982-whiplash
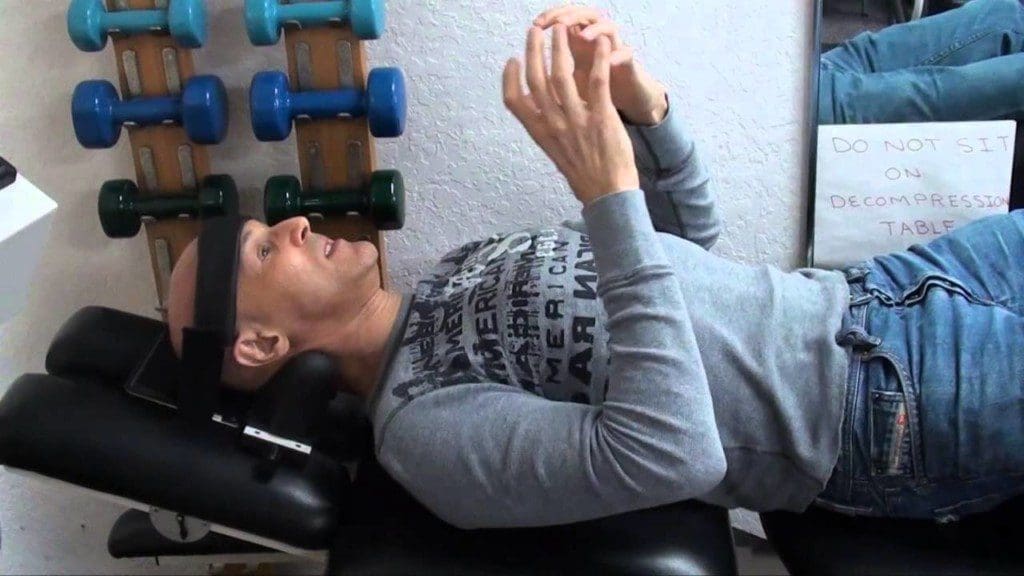
Discovering the Benefits of Chiropractic Care- Video

The Role of Physical Therapy in Treating Whiplash
Physical therapy is like a trusty sidekick for whiplash recovery—it’s got all the tools to help you bounce back. Here’s how it works its magic:
- Pain Relief: Therapists employ techniques such as manual therapy (gentle massage), ultrasound, and electrical stimulation to alleviate pain and reduce inflammation. It’s like giving your neck a spa day, but with science.
- Restoring Range of Motion: Whiplash can make your neck stiffer than a board. Gentle exercises and mobilization techniques help loosen up the muscles.
- Strengthening Muscles: Weak neck muscles can worsen pain. Physical therapy includes exercises to strengthen those muscles, providing your neck with better support.
- Education and Prevention: Therapists teach you how to sit, stand, and move without aggravating your injury. They’re like your personal neck coach.
Research supports this approach. A study found that early physical therapy for whiplash-associated disorders (WAD) leads to better outcomes, with patients recovering faster when treatment starts within weeks of the injury (Walton & Elliott, 2017). Another study showed that active mobilization—gentle neck movements—beats rest or neck collars, which can slow recovery (Physiopedia, n.d.). A study involving 216 people found that neck exercises resulted in significant pain reduction in 39-44% of participants after six months (El Paso Chiropractor Blog, 2016).
So, don’t let whiplash keep you down—physical therapy can help you get back to turning your head without wincing.
References
- Walton, D. M., & Elliott, J. M. (2017). An integrated model of chronic whiplash-associated disorder. Journal of Orthopaedic & Sports Physical Therapy, 47(7), 462–471. https://www.jospt.org/doi/pdf/10.2519/jospt.2017.7455
- Physiopedia. (n.d.). Whiplash Associated Disorders. Retrieved from https://www.physio-pedia.com/Whiplash_Associated_Disorders
- El Paso Chiropractor Blog. (2016). Whiplash and Exercise. Retrieved from https://www.elpasochiropractorblog.com/2016/05/whiplash-and-exercise.html
Clinical Insights from Dr. Alexander Jimenez
Dr. Alexander Jimenez is like the MacGyver of healthcare—armed with a chiropractic degree, a nurse practitioner certification, and over 30 years of experience, he’s ready to tackle whiplash like a pro. At his Injury Medical & Chiropractic Clinic in El Paso, he takes a holistic approach, combining chiropractic care, physical therapy, and functional medicine to help patients achieve optimal recovery.
Dr. Jimenez believes in treating the whole person, not just the injury. He uses functional medicine to delve into underlying issues, such as inflammation or nutritional deficiencies, that may slow healing. For whiplash, he often combines chiropractic adjustments to realign the spine with physical therapy exercises to strengthen neck muscles. He also emphasizes patient education, teaching folks how to care for their necks at home (Sciatica Clinic, 2025).
Take John, a 35-year-old accountant, who came to Dr. Jimenez after being involved in a rear-end collision. John had severe neck pain and headaches that made work impossible. Dr. Jimenez created a plan with weekly adjustments, including physical therapy exercises and dietary advice, to reduce inflammation. Within a month, John’s pain dropped significantly, and after two months, he was back to work full-time. That’s the kind of results Dr. Jimenez delivers.
His approach isn’t just about quick fixes—it’s about building long-term health so you can avoid future injuries. It’s like giving your body a tune-up, not just a patch job.
References
- Sciatica Clinic. (2025). Work Awareness and Injury Prevention Tips For Whiplash. Retrieved from https://sciatica.clinic/work-awareness-and-injury-prevention-tips-for-whiplash/amp/
- Dr. Alexander Jimenez LinkedIn Profile. (n.d.). Retrieved from https://www.linkedin.com/in/dralexjimenez/
Personal Injury Cases in El Paso
El Paso’s busy highways and border traffic make it a hotspot for car accidents, and whiplash is a frequent player in personal injury cases. These cases often involve medical bills, lost wages, and pain and suffering, which can add up quickly, much like a speeding ticket. That’s where Dr. Jimenez comes in, acting as a bridge between medical care and legal needs.
As a chiropractor and nurse practitioner, Dr. Jimenez provides detailed medical reports that are gold for personal injury claims. These reports document your injuries, treatments, and progress, helping lawyers and insurance companies understand the full extent of your accident’s impact. His thorough documentation—backed by physical exams, imaging, and functional assessments—ensures you have the evidence needed for fair compensation (Sciatica Clinic, 2025).
For patients, this means you can focus on healing while Dr. Jimenez handles the paperwork. It’s like having a personal assistant who’s also a medical genius. His reputation in El Paso makes his reports highly credible, giving accident victims a strong shot at justice.
References
- Sciatica Clinic. (2025). Work Awareness and Injury Prevention Tips For Whiplash. Retrieved from https://sciatica.clinic/work-awareness-and-injury-prevention-tips-for-whiplash/amp/
Advanced Diagnostic Techniques
Dr. Jimenez doesn’t mess around when it comes to figuring out what’s wrong. He uses advanced diagnostic tools to get a clear picture of your injury. Through his partnership with Diagnostic Outpatient Imaging (DOI) in El Paso, he has access to state-of-the-art X-rays, CT scans, and MRIs. These images can reveal hidden issues, such as ligament tears or disc bulges, that may not be visible during a regular exam (Diagnostic Outpatient Imaging, n.d.).
He also uses functional assessments, such as range of motion and strength tests, to evaluate how your body is functioning. Blood tests might be ordered to check for inflammation or nutritional issues that could be slowing your recovery. For example, if you have high inflammation, he might suggest incorporating anti-inflammatory foods into your diet alongside your physical therapy.
This combo of high-tech imaging and functional medicine is like having a GPS for your recovery—it helps Dr. Jimenez navigate exactly what you need to heal.
References
- Diagnostic Outpatient Imaging. (n.d.). Retrieved from https://dralexjimenez.com/diagnostic-outpatient-imaging/
Preventing Whiplash and What to Do After an Accident
You can’t always avoid accidents, but you can take steps to lower your whiplash risk:
- Adjust Your Headrest: Position it level with your head and close to your neck. It’s like a helmet for your neck.
- Wear Your Seatbelt: It’s your best defense against serious injuries.
- Drive Defensively: Stay alert and avoid distractions, such as texting.
If you’re in an accident, see a doctor right away, even if you feel fine. Whiplash symptoms can be sneaky. Describe all your symptoms, keep records of treatments, and save receipts for expenses—they’re crucial for insurance claims or lawsuits (National Safety Council, n.d.).
References
- National Safety Council. (n.d.). Whiplash Prevention. Retrieved from https://www.nsc.org/road-safety/safety-topics/whiplash-prevention
Conclusion
Physical therapy is a cornerstone of recovery for whiplash after an MVA, helping reduce pain, restore movement, and prevent chronic issues. Dr. Alexander Jimenez, with his extensive experience and integrative approach, is a leading figure in El Paso for treating these injuries. His use of advanced diagnostics and holistic care ensures patients get personalized, effective treatment. If you’ve been in an accident, don’t wait—seek professional care early to improve your recovery chances.
Disclaimer: This blog post is for informational purposes only and should not be taken as medical advice. Always consult with a healthcare professional for diagnosis and treatment of any medical condition.
Key Citations
- Mayo Clinic: Whiplash Symptoms and Causes https://www.mayoclinic.org/diseases-conditions/whiplash/symptoms-causes/syc-20378919
- Cleveland Clinic: Whiplash (Neck Strain) Information https://my.clevelandclinic.org/health/diseases/11982-whiplash
- Physiopedia: Whiplash Associated Disorders https://www.physio-pedia.com/Whiplash_Associated_Disorders
- Expert Court Reports: Importance of Physiotherapy After RTA https://www.expertcourtreports.co.uk/blog/the-importance-of-physiotherapy-after-a-road-traffic-accident-rta/
- Walton & Elliott: Integrated Model of Chronic WAD https://www.jospt.org/doi/pdf/10.2519/jospt.2017.7455
- El Paso Chiropractor Blog: Whiplash and Exercise https://www.elpasochiropractorblog.com/2016/05/whiplash-and-exercise.html
- Sciatica Clinic: Work Awareness and Whiplash Prevention https://sciatica.clinic/work-awareness-and-injury-prevention-tips-for-whiplash/amp/
- Dr. Alexander Jimenez LinkedIn Profile https://www.linkedin.com/in/dralexjimenez/
- Diagnostic Outpatient Imaging Services https://dralexjimenez.com/diagnostic-outpatient-imaging/
- National Safety Council: Whiplash Prevention Tips https://www.nsc.org/road-safety/safety-topics/whiplash-prevention