“Can understanding moderate exercise and how to measure the amount of exercise help expedite individuals’ health goals and well-being?”

Table of Contents
Moderate Exercise
Various physical activity guidelines recommend regular, moderate exercise for achieving and maintaining health and wellness. Getting the minimum, moderate weekly physical activity can help prevent disease, increase mental well-being, support weight loss and maintenance, and improve quality of life.
What Is It?
- Anything that gets the heart pumping and beating faster is considered moderate exercise. (U.S. Department of Health and Human Services, 2018)
- Moderate-intensity cardiovascular exercise includes – brisk walking, yard work, mopping, vacuuming, and playing various sports that require consistent movement.
- When engaged in moderate exercise, individuals should breathe harder but still be able to carry a conversation. (American Heart Association, 2024)
- The talk test is a way to monitor whether the exercise is at moderate intensity.
Benefits
Regular moderate exercise can help (American Heart Association, 2024)
- Decrease the risk of developing conditions like heart disease, type 2 diabetes, and dementia.
- Improve sleep and help with sleep disorders.
- Improve brain functions like memory, focus, and processing.
- With weight loss and/or maintenance.
- Improve bone health.
- Reduce depression, anxiety, and other mental health symptoms.
How Much Exercise?
The prescription for moderate exercise includes:
- 30 minutes a day for five days a week, or two hours and 30 minutes per week. (U.S. Department of Health and Human Services, 2018)
- Physical activity needs to continue for at least 10 minutes to be considered an exercise session.
- Individuals can break up their 30 daily minutes into two to three shorter sessions, each 10 minutes long.
- As the ability to exercise increases, aim to increase moderate activities.
- Individuals will reap even more health benefits if they increase moderate aerobic exercise time to 300 minutes or five hours weekly. (U.S. Department of Health and Human Services, 2018)
Measuring Exercise
- A moderate level of activity noticeably increases heart and breathing rate.
- Individuals sweat but can still carry on a conversation.
- Individuals can talk but can’t sing.
- Individuals will feel the exercise but are not huffing and puffing.
- Individuals can use different scales to measure exercise intensity.
Heart Rate
- A moderate-intensity heart rate is 50% to 70% of an individual’s maximum heart rate. (Centers for Disease Control and Prevention, 2022)
- An individual’s maximum heart rate varies by age.
- A heart rate chart or calculator can determine an individual’s maximum heart rate.
- To measure heart rate mid-exercise, individuals can take their pulse or use a heart rate monitor, app, fitness tracker, or smartwatch to ensure they stay at a moderate intensity.
MET
- M.E.T. stands for Metabolic Equivalent for Task and refers to the amount of oxygen the body uses during physical activity.
- Assigning METs to an activity allows individuals to compare the amount of exertion an activity takes.
- This works for individuals with different weights.
- During moderate physical activity, breathing and heart rate increase, and the body burns around 3.5 to 7 calories a minute.
- The actual number burned depends on your weight and fitness level.
- The body uses 1 MET for basic functions like breathing.
- Grades of activity:
- 1 MET – Body at rest
- 2 METs – Light activity
- 3-6 METs – Moderate activity
- 7 or more METs – Vigorous activity
Perceived Exertion Scale
Individuals can also check their activity level using the Borg Rating of Perceived Exertion scale/RPE. (Centers for Disease Control and Prevention, 2022) Using this scale involves monitoring how an individual feels about how hard their body is working during physical activity. The scale starts at 6 and ends at 20. A perceived exertion between 11 and 14 is considered moderate physical activity.
- 6 – No exertion – sitting still or sleeping
- 7-8 – Extremely light exertion
- 9-10 – Very light exertion
- 11-12 – Light exertion
- 13-14 – Somewhat hard exertion
- 15-16 – Heavy exertion
- 17-18 – Very heavy exertion
- 20 – Maximum exertion
Examples
Many activities are counted as moderate-intensity exercise. Choose some appealing and learn to add them to a weekly routine.
- Ballroom dancing
- Line dancing
- Gardening
- House chores that get the heart pumping.
- Softball
- Baseball
- Volleyball
- Doubles tennis
- Brisk walking
- Light jogging
- Walking or jogging on a treadmill
- Using an elliptical trainer
- Bicycling under 10 miles an hour on ground level
- Leisurely swim
- Water aerobics
Mobility Challenges
- Individuals with mobility issues can achieve moderate intensity using a manual wheelchair or a handcycle and swimming or water aerobics.
- Individuals who can use their legs but can’t tolerate walking or jogging can try bicycling or swimming.
Getting More Exercise
There are different ways to incorporate and increase moderate physical activities. These include:
10-minute Activity Bursts
- Walk briskly for at least 10 minutes at a time.
- Walk at an easy pace for a couple of minutes.
- Pick up the pace for 10 minutes.
- Try to walk during work breaks or lunch and/or before or after work.
Walking Workouts
- Individuals can walk indoors, outdoors, or on a treadmill.
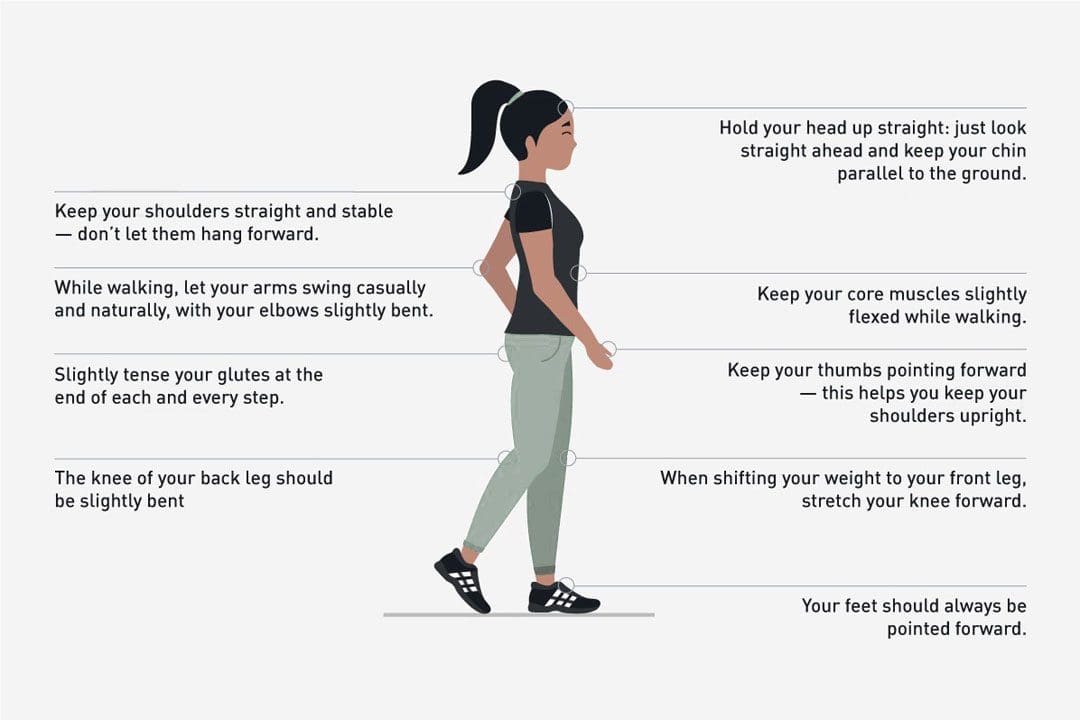
- Proper posture and walking techniques make it easier to achieve a brisk pace.
- Once comfortable walking briskly for 10 minutes, begin to extend walking time.
- Try different walking workouts that offer fast walks, jogging intervals, and/or adding hills or treadmill inclines.
New Activities
- Individuals are recommended to experiment with various exercises to find what works for them.
- Consider roller skating, blading, or skateboarding to increase heart rate.
Moderate physical activity will get and keep the body in shape. Individuals should not become distressed if they can only do a little at first. Allow time to build endurance and gradually make time each day for enjoyable physical activities.
Transform Your Body
References
U.S. Department of Health & Human Services. (2018). Physical Activity Guidelines for Americans, 2nd edition. Retrieved from https://health.gov/sites/default/files/2019-09/Physical_Activity_Guidelines_2nd_edition.pdf
American Heart Association. (2024). American Heart Association recommendations for physical activity in adults and kids. (Healthy Living, Issue. https://www.heart.org/en/healthy-living/fitness/fitness-basics/aha-recs-for-physical-activity-in-adults
Centers for Disease Control and Prevention. (2022). Target heart rate and estimated maximum heart rate. Retrieved from https://www.cdc.gov/physicalactivity/basics/measuring/heartrate.htm
Centers for Disease Control and Prevention. (2022). Perceived exertion (Borg Rating of Perceived Exertion Scale). Retrieved from https://www.cdc.gov/physicalactivity/basics/measuring/exertion.htm