Individuals that experience frequent headaches can have sensitive headache trigger points. Every case is different and requires a thorough examination before a proper and personalized chiropractic treatment plan can begin. Headaches can be brought on from a variety of causes. This could be:
- Drug reactions
- Temporomandibular joint dysfunction (TMJ)
- Tightness in the neck muscles
- Low blood sugar
- High blood pressure
- Stress
- Fatigue
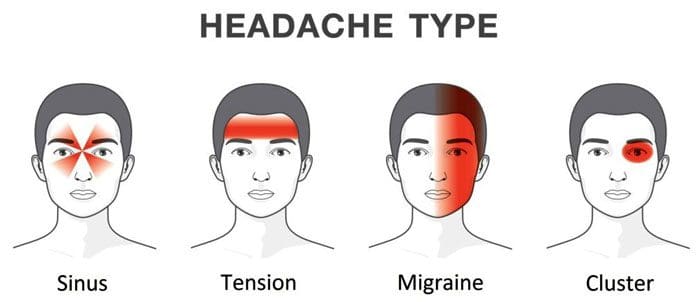
The majority of recurrent headaches fall into three types:
- Tension headaches, also known as cervicogenic headaches
- Migraine headaches
- Cluster headaches, which are related to migraines.
Table of Contents
Tension
Tension headaches are the most common and affect around 77% of individuals experiencing chronic headaches. Most individuals describe a tension headache as a consistent dull ache on one side of the head and sometimes both sides. They are often described as having a tight band/belt around the head or behind the eyes. These headaches usually start slowly, gradually and can last for a few minutes or days. They tend to start in the middle of the day or before the end of the day.
These headaches can be the result of stress and/or poor posture. The most common cause is subluxations in the upper back and neck, usually combined with active headache trigger points. This stresses the spinal muscles in the upper back and neck. A tension headache or stress headache can last 30 minutes to a few days. Chronic tension headaches can last for months. The pain can be severe; however, these headaches are typically not associated with symptoms like throbbing, nausea, or vomiting.
If the top cervical vertebrae shift out of their position and lose their normal motion, a small muscle called the rectus capitis posterior minor/RCPM begins to spasm. This small muscle has a tendon that slips between the upper neck and the base of the skull. It attaches to a thin, sensitive tissue called the dura mater that covers the brain. The dura mater is very pain-sensitive. When the RCPM muscle goes into spasm, the tendon pulls the dura mater causing a headache. Individuals that work at a desk station for long hours tend to experience headaches from this cause. Another cause comes from referred pain caused by headache trigger points in the Sternocleidomastoid/SCM or levator muscle on the side of the neck. This cause tends to happen more to individuals that have suffered a whiplash injury with muscle damage in the neck region.
Migraine Headaches
Migraines are intense and throbbing headaches that are associated with nausea and sensitivity to light or noise. They can last for a few hours to a few days. Many experience visual symptoms known as an aura just before they come on. This is described as seeing flashing lights or when things take on a dream-like appearance. However, even in individuals that don’t experience the aura, most can tell that a migraine is getting ready to present. Individuals usually have their first attack before age 30. They tend to run in families supporting a genetic component. Some have attacks several times a month, while others can have less than one a year. Most individuals find that migraines happen less and become less severe as they get older.
These headaches are caused by the constriction of blood vessels in the brain. During the constriction period, there is a decrease in blood circulation. This is followed by dilation/enlargening of the blood vessels. This is what leads to the visual symptoms. Then the blood vessels dilate, generating a rapid increase in blood pressure inside the head. This increased pressure is what leads to a pounding headache. Every time the heart beats, it sends another shock wave through the carotid arteries in the neck into the brain. There are different theories as to why the blood vessels constrict, but they are still unknown. What is known is that several factors can trigger a migraine. This includes:
- Lack of sleep
- Stress
- Flickering lights
- Strong smells
- Changing weather
- Foods that are high in an amino acid known as tyramine
Cluster
Cluster headaches are very short excruciating headaches. They are usually felt on one side of the head behind the eyes. These headaches affect about 1 million individuals and are more common in men. This type of headache tends to happen at night. They are called cluster headaches because they tend to happen one to four times a day over several days. After one cluster is over, it could be months or even years before they present again. Like migraines, cluster headaches cause the dilation of the blood vessels in the brain, increasing the pressure.
Trigger Points
Headache trigger point therapy involves four muscles. These are the:
- Splenius muscles
- Suboccipitals
- Sternocleidomastoid – SCM
- Trapezius
The Splenius muscles involve two individual muscles, the Splenius Capitis and the Splenius Cervicis. These muscles run along the upper back to the skull base or the upper cervical/neck vertebrae. Trigger points in the Splenius muscles are a common contributor to pain that travels through the head to the back of the eye and top of the head.
The Suboccipitals are a group of four small muscles that maintain proper movement and positioning between the first cervical vertebra and the skull base. Trigger points in these muscles can cause pain that feels like it’s happening inside the head, from the back to the eye and forehead. Individuals report that the whole side of the head hurts. This is a pain pattern similar to a migraine.
The Sternocleidomastoid muscle runs along the base of the skull, behind the ear, down the side of the neck. It attaches to the top of the sternum/breastbone. Although most are not aware of this muscle’s trigger points, the effects are evident. This includes:
- Referred pain
- Balance issues
- Visual symptoms
Referred pain tends to be eye pain, headaches over the eye, and can even cause earaches. An unusual characteristic of SCM headache trigger points is that they can cause dizziness, nausea, and balance problems.
The trapezius muscle is the large, flat muscle in the upper and middle back. Pain can be felt in the temple and back of the head. A common trigger point is located at the top of the muscle. This particular point can activate secondary trigger points in the temple or jaw muscles, leading to jaw or tooth pain.
Headache Triggers
- Stress can be a trigger.
- Depression, anxiety, frustration, and even pleasant excitement can be associated with headache development.
- A headache diary can help determine whether factors like food, weather, and/or mood correlate with headache patterns.
- Repeated exposure to nitrite compounds can result in a dull headache accompanied by a flushed face. Nitrite dilates blood vessels and is found in products like heart medications, and is also used as a chemical to preserve meat. Processed meats containing sodium nitrite can contribute to headaches.
- Foods prepared with monosodium glutamate or MSG can result in headaches. Soy sauce, meat tenderizers, and various packaged foods contain this chemical as a flavor enhancer.
- Exposure to poisons, even household varieties like insecticides, carbon tetrachloride, and lead, can contribute.
- Contact with lead batteries or lead-glazed pottery.
- Foods that are high in the amino acid tyramine should be avoided. This could be ripened cheeses like cheddar, brie, chocolate, and pickled or fermented food.
Bio-Chiropractic
Chiropractic adjustments are highly effective for treating tension headaches, especially those that originate in the neck. Research has found that spinal manipulation resulted in almost immediate improvement and had fewer side effects and longer-lasting relief than taking common medications. There is a significant improvement by manipulating the upper two cervical vertebrae, combined with adjustments to the area between the cervical and thoracic spine.
Body Composition Testing
Vibration Exercise
Vibration exercise is believed to stimulate the muscle fibers without going to a gym or stressing the bones. One study broke up postmenopausal women into three groups: resistance training, vibration training combined with resistance training, or no exercise/training. Their body composition was measured before starting the study. After the study was completed, the findings included:
- Both the resistance group and the resistance group with vibration training increased lean tissue mass.
- The control group did not show an increase in lean tissue and, in fact, gained body fat.
- The combination group, using vibration training with resistance training, showed a drop in body fat.
Another study placed male athletes in a training program that included vibration training. The first group had lower-limb strength training combined with vibration training, and the other had lower-limb strength training without vibration training. The researchers found that the athletes in the vibration training group improved leg extension strength by five percent. In addition, the vibration training groups balancing ability and vertical lift/jumping test improved as well.
References
Bryans, Roland et al. “Evidence-based guidelines for the chiropractic treatment of adults with headache.” Journal of manipulative and physiological therapeutics vol. 34,5 (2011): 274-89. doi:10.1016/j.jmpt.2011.04.008
Chaibi, Aleksander et al. “Chiropractic spinal manipulative therapy for cervicogenic headache: a single-blinded, placebo, randomized controlled trial.” BMC research notes vol. 10,1 310. 24 Jul. 2017, doi:10.1186/s13104-017-2651-4
Bryans R, Descarreaux M, Duranleau M, et al. Evidence-based guidelines for the chiropractic treatment of adults with neck pain. J Manipulative Physiol Ther 2014; 37: 42-63.
Bryans R, Descarreaux M, Duranleau M, et al. Evidence-based guidelines for the chiropractic treatment of adults with headache. J Manipulative Physiol Ther 2011; 34: 274-89.
Professional Scope of Practice *
The information herein on "Headache Trigger Points and Bio-Chiropractic Treatment" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card