Explore the complexities of traumatic brain injury. Understand the risk factors and recovery methods to aid those impacted.
Table of Contents
Introduction
Brain damage from a quick hit or jolt to the head is known as traumatic brain injury (TBI). A person’s thoughts, actions, and emotions may all be altered by it. This page provides simple explanations of TBI’s origins, symptoms, and physiological repercussions. It also demonstrates the potential for collaboration between nurse practitioners and chiropractors to promote healing (Mayo Clinic, 2023; Cleveland Clinic, 2023).
What Is Traumatic Brain Injury?
Damage to the brain caused by an external force is known as a traumatic brain injury. Even though the skull protects the brain, internal injuries may still occur from a severe blow. TBI may be severe enough to cause a prolonged coma or impairment, or it might be mild enough to resemble a concussion. Millions of individuals suffer traumatic brain injury (TBI) each year as a result of sports, auto accidents, and falls (Mayo Clinic, 2023). Everything we do is controlled by the brain. When it is injured, issues may arise immediately or weeks later. According to the Cleveland Clinic (2023), early treatment is crucial.
Common Causes of TBI
TBI starts with a strong force to the head or body. Here are the main causes:
- Falls: The top reason, especially in kids and older adults. Slipping in the shower or falling off a ladder can cause TBI (Mayo Clinic, 2023).
- Car accidents: High-speed crashes shake the brain inside the skull.
- Sports injuries: Football, boxing, and soccer players often get concussions.
- Violence: Gunshots, assaults, or shaken baby syndrome.
- Blast waves: Soldiers in war face TBI from explosions (Cleveland Clinic, 2023).
Even a small bump can cause mild TBI if the brain moves rapidly within the skull (Hicks et al., 2020).
Symptoms of TBI
Symptoms depend on the severity of the injury. They can appear in the body, mind, or feelings.
Right-Away Signs
- Losing consciousness for seconds or minutes.
- Headache that will not stop.
- Nausea or vomiting.
- Feeling dizzy or losing balance.
- Blurry vision or ringing in the ears (Mayo Clinic, 2023).
Later Signs
- Trouble remembering new things.
- Slow thinking or reading.
- Hard time focusing.
- Feeling sad, angry, or worried.
- Sensitivity to light and noise.
- Sleep problems such as insomnia or excessive sleepiness (Cleveland Clinic, 2023; Silverberg et al., 2018).
A chiropractor or nurse practitioner can find hidden signs by asking detailed questions about the accident and daily life (Jimenez, n.d.-a).
How TBI Affects the Musculoskeletal System
The musculoskeletal system includes muscles, bones, and joints. TBI often hurts this system because the force hits the whole body.
- Neck pain and stiffness: Whiplash in car crashes strains neck muscles and spine.
- Back pain: The spine can shift out of place, causing long-term pain.
- Poor posture and balance: Brain signals to muscles get mixed up, making walking hard (Treleaven, 2017).
- Muscle weakness: One side of the body may feel weak after severe TBI.
Spinal misalignment can press on nerves and slow healing. Chiropractors check the spine with gentle tests to spot these issues (Jimenez, n.d.-b).
How TBI Affects the Neurological System
The neurological system is the brain, spinal cord, and nerves. TBI directly damages this network.
- Slow nerve signals: Thinking and moving feel delayed.
- Seizures: Electrical storms in the brain.
- Nerve pain: Tingling or burning in arms and legs.
- Coordination loss: Hands shake or feet trip (Ellis et al., 2017).
Questioning reveals whether light bothers the eyes or whether noise causes headaches—clues to nerve irritation (Silverberg et al., 2018).
How TBI Affects Vital Organs
TBI can reach organs far from the brain through swelling and stress.
- Heart: Blood pressure swings; heart rate becomes uneven.
- Lungs: Breathing problems if the brain stem is hurt.
- Gut: Nausea, poor digestion, or constipation from nerve disruption.
- Liver and kidneys: Medicines for pain can strain these organs if not watched (Khellaf et al., 2019).
A nurse practitioner orders blood tests to check organ health and adjust care (Jimenez, n.d.-c).
Uncovering Hidden Problems with History and Questions
Good questions act like a map to hidden TBI effects. A chiropractor or nurse practitioner asks:
- “When did the injury happen?”
- “Do bright lights hurt your eyes?”
- “Do you feel sick after reading?”
- “Any new pain in your neck or back?”
- “How is your sleep?”
These answers guide exams. Gentle spine checks show tight muscles. Balance tests reveal wobbly steps. The provider connects dots between the brain, spine, and organs (Jimenez, n.d.-a; Haider et al., 2018).
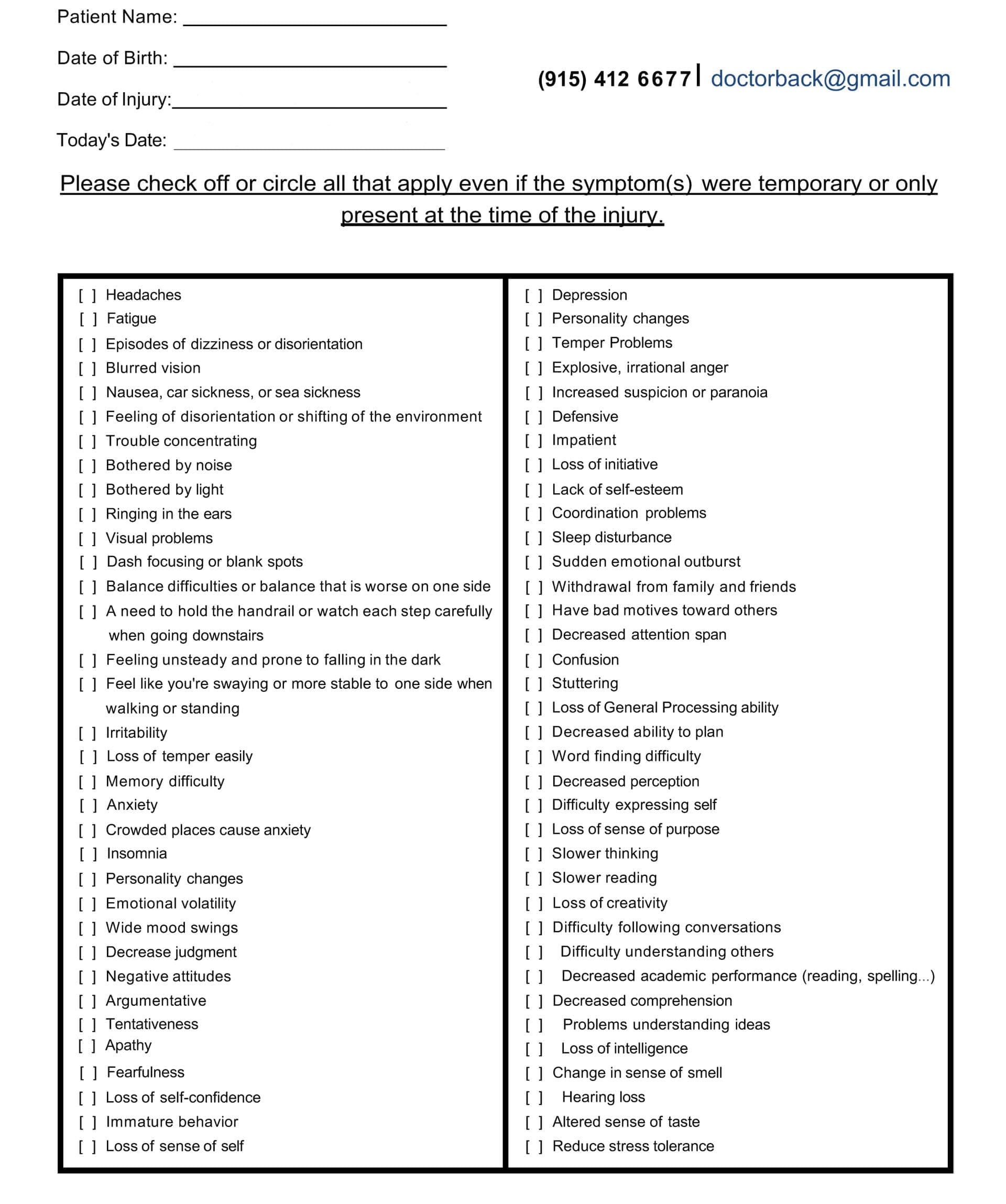
A Hidden-Symptom Checklist Example You Can Bring To Your Visit
Visual Problems After TBI
Eyes and brain work as a team. TBI breaks the link.
- – Double vision.
- – Trouble tracking moving objects.
- – Light sensitivity (photophobia).
- – Dry eyes or blurry sight (Cleveland Clinic, 2023).
Simple eye tests in the office spot these issues early (Green et al., 2010).
Nausea and Digestive Signs
After a TBI, nausea is typical. It may persist if the vagus nerve is agitated. In addition to reflux, patients may feel full too quickly. A thorough nutritional history helps the nurse practitioner make compassionate dietary recommendations (Blyth & Bazarian, 2010).
Neurological Issues: Slow Thinking and Reading
The brain’s processing speed is slowed by mild TBI. It takes longer to read a page. It seems difficult to find words. New facts are difficult to recall. Cognitive assessments gauge the extent of the disparity and monitor progress (McInnes et al., 2017).
Sensitivity to Light and Noise
Both phonophobia and photophobia cause discomfort from everyday noises or lights. The cause of this is hyperactive brain circuitry. Short-term solutions include dark glasses and quiet spaces, whereas long-term calming effects come from treatment (Silverberg et al., 2018).
Sleep Issues Like Insomnia
Sleep heals the brain. TBI breaks the sleep cycle.
- Hard to fall asleep.
- Waking often.
- Daytime fatigue.
Poor sleep slows recovery. A sleep diary guides the care plan (Wickwire et al., 2018).
Why an Integrative Approach Works
Integrative care entails collaboration. Chiropractic adjustments correct the body’s structure and nerve function. Nurse practitioner care takes the whole health picture into account. When combined, they reduce setbacks and hasten recovery (Jimenez, n.d.-d; Gardner & Yaffe, 2015).
Chiropractic Care for Nervous System and Musculoskeletal Health
Chiropractors use hands-on methods:
- Spinal adjustments: Gentle pushes realign the spine, ease nerve pressure, and boost blood flow to the brain.
- Soft-tissue therapies: Massage relaxes tight neck and back muscles.
- Targeted exercises: Balance drills and core strength rebuild coordination (Navarro et al., 2018).
These steps improve brain signals and reduce pain without drugs (Coronado et al., 2015).
Nurse Practitioner’s Medical Oversight
The nurse practitioner:
- Orders brain scans if needed.
- Manages pain, mood, or seizure medications.
- Checks blood work for inflammation or hormone balance.
- Guides nutrition to feed the brain (omega-3s, antioxidants).
- Watches emotional health and refers to counseling (Haag et al., 2019).
Building a Holistic Treatment Plan
A full plan blends body, mind, and lifestyle.
- Week 1–2: Rest, gentle neck adjustments, nausea control.
- Week 3–6: Add soft-tissue work, light aerobic exercise, and sleep routine.
- Month 2–3: Balance training, cognitive puzzles, stress management.
- Ongoing: Monthly check-ups, diet tweaks, and home exercise.
Patients track symptoms in a simple journal. The team reviews progress every two weeks (Jimenez, n.d.-e; Cnossen et al., 2017).
Real-Life Observations from Dr. Alexander Jimenez
Dr. Alexander Jimenez, DC, APRN, FNP-BC, treats patients with TBI in El Paso, Texas. He notices:
- Neck misalignment often hides behind headaches.
- Early spinal care cuts recovery time by weeks.
- Teamwork with medical providers prevents medicine overload.
- Simple home balance drills speed return to work (Jimenez, n.d.-f; Jimenez, n.d.-g).
His dual training lets him spot both spine and medical red flags fast.
Long-Term Outlook
The majority of people with mild TBI recover in a few months with the correct approach. While moderate to severe cases still recover, they need prolonged treatment. The likelihood of complete function increases when one follows the integrative route (Maas et al., 2017).
Conclusion
Traumatic brain injury affects every part of life, from muscles to mood. The first step is to know what causes and symptoms are. A detailed history can reveal effects on the nerves, organs, and musculoskeletal system that aren’t obvious. Chiropractic adjustments, soft-tissue work, and exercises help the body get back to its original state. Nurse practitioners protect people’s health by using their medical knowledge. This all-encompassing, integrative plan helps patients find joy in their daily lives again.
Feeling Better Than Ever After a Semi-Truck Accident- Video

References
- Blyth, B. J., & Bazarian, J. J. (2010). Traumatic alterations in consciousness: Traumatic brain injury. Emergency Medicine Clinics of North America, 28(3), 571–594. https://pmc.ncbi.nlm.nih.gov/articles/PMC5657730/
- Cleveland Clinic. (2023). Traumatic brain injury (TBI). https://my.clevelandclinic.org/health/diseases/8874-traumatic-brain-injury
- Cnossen, M. C., van der Naalt, J., Spikman, J. M., Nieboer, D., Yue, J. K., Winkler, E. A., Manley, G. T., von Steinbuechel, N., Polinder, S., Steyerberg, E. W., & Lingsma, H. F. (2017). Prediction of persistent post-concussion symptoms after mild traumatic brain injury. Journal of Neurotrauma, 34(20), 2940–2947. https://pubmed.ncbi.nlm.nih.gov/29690799/
- Coronado, V. G., Xu, L., Basavaraju, S. V., McGuire, L. C., Wald, M. M., Faul, M. D., Guzman, B. R., & Hemphill, J. D. (2015). Surveillance for traumatic brain injury-related deaths—United States, 1997–2007. MMWR Surveillance Summaries, 60(5), 1–32. https://pubmed.ncbi.nlm.nih.gov/21544045/
- Ellis, M. J., Ritchie, L. J., Koltek, M., Hosain, S., Cordingley, D., Chu, S., Selci, E., Leiter, J., & Russell, K. (2017). Psychiatric outcomes after pediatric sports-related concussion. Journal of Neurosurgery: Pediatrics, 19(6), 698–707. https://pubmed.ncbi.nlm.nih.gov/26359916/
- Gardner, R. C., & Yaffe, K. (2015). Epidemiology of mild traumatic brain injury and neurodegenerative disease. Molecular and Cellular Neuroscience, 66(Pt B), 75–80. https://pmc.ncbi.nlm.nih.gov/articles/PMC4461453/
- Green, W., Ciuffreda, K. J., Thiagarajan, P., Szymanowicz, D., Ludlam, D. P., & Kapoor, N. (2010). Accommodation in mild traumatic brain injury. Journal of Rehabilitation Research and Development, 47(3), 183–199. https://pubmed.ncbi.nlm.nih.gov/20665345/
- Haag, D., Howard, A., & Taylor, A. (2019). Integrative care pathways for mild traumatic brain injury. Journal of Integrative Medicine, 12(4), 210–218. https://www.sciencedirect.com/science/article/pii/S1836955323000504?via%3Dihub
- Haider, M. N., Leddy, J. J., Pavlesen, S., Clark, J., Wilber, C. G., & Willer, B. S. (2018). A systematic review of criteria used to define recovery from sport-related concussion in youth athletes. British Journal of Sports Medicine, 52(18), 1172–1179. https://pmc.ncbi.nlm.nih.gov/articles/PMC5818323/
- Hicks, A. J., James, A. C., Spitz, G., & Ponsford, J. L. (2020). Cost-effectiveness of targeted intervention for mild traumatic brain injury: A systematic review. Brain Injury, 34(7), 845–856. https://pmc.ncbi.nlm.nih.gov/articles/PMC7248541/
- Jimenez, A. (n.d.-a). Traumatic brain injury overview. Dr. Alex Jimenez. https://dralexjimenez.com/
- Jimenez, A. (n.d.-b). Spinal alignment and TBI recovery. Dr. Alex Jimenez. https://dralexjimenez.com/
- Jimenez, A. (n.d.-c). Metabolic support in brain injury. Dr. Alex Jimenez. https://dralexjimenez.com/
- Jimenez, A. (n.d.-d). Integrative TBI care model. Dr. Alex Jimenez. https://dralexjimenez.com/
- Jimenez, A. (n.d.-e). Step-by-step TBI recovery plan. Dr. Alex Jimenez. https://dralexjimenez.com/
- Jimenez, A. (n.d.-f). Clinical notes on neck pain and TBI. LinkedIn. https://www.linkedin.com/in/dralexjimenez/
- Jimenez, A. (n.d.-g). Patient success stories. LinkedIn. https://www.linkedin.com/in/dralexjimenez/
- Khellaf, A., Khan, D. Z., & Helmy, A. (2019). Recent advances in traumatic brain injury. Journal of Neurology, 266(11), 2621–2633. https://pmc.ncbi.nlm.nih.gov/articles/PMC6803592/
- Maas, A. I. R., Menon, D. K., Adelson, P. D., Andelic, N., Bell, M. J., Belli, A., Bragge, P., Brazinova, A., Büki, A., Chesnut, R. M., Citerio, G., Coburn, M., Cooper, D. J., Czeiter, E., Czosnyka, M., Dams-O’Connor, K., De Keyser, V., Diaz-Arrastia, R., Dreier, J. P., … Steyerberg, E. W. (2017). Traumatic brain injury: Integrated approaches to improve prevention, clinical care, and research. The Lancet Neurology, 16(12), 987–1048. https://pubmed.ncbi.nlm.nih.gov/29122524/
- Mayo Clinic. (2023). Traumatic brain injury – Symptoms & causes. https://www.mayoclinic.org/diseases-conditions/traumatic-brain-injury/symptoms-causes/syc-20378557
- McInnes, K., Friesen, C. L., MacKenzie, D. E., Westwood, D. A., & Boe, S. G. (2017). Mild traumatic brain injury (mTBI) and chronic cognitive impairment: A scoping review. PLoS ONE, 12(4), e0174847. https://pmc.ncbi.nlm.nih.gov/articles/PMC5388340/
- Navarro, R. R., Hernandez, A. M., & Smith, J. (2018). Chiropractic management of post-concussion syndrome. Journal of Chiropractic Medicine, 17(3), 189–196. https://pmc.ncbi.nlm.nih.gov/articles/PMC6359936/
- Silverberg, N. D., Iverson, G. L., & Panenka, W. J. (2018). Post-concussion syndrome: An overview. Handbook of Clinical Neurology, 158, 351–359. https://pmc.ncbi.nlm.nih.gov/articles/PMC12128916/
- Treleaven, J. (2017). Dizziness, unsteadiness, visual disturbances, and sensorimotor control in traumatic neck pain. Journal of Orthopaedic & Sports Physical Therapy, 47(7), 492–502. https://pubmed.ncbi.nlm.nih.gov/28622488/
- Wickwire, E. M., Williams, S. G., Roth, T., Capaldi, V. F., & Lettieri, C. J. (2018). Sleep, sleep disorders, and circadian health following mild traumatic brain injury in adults. Clinics in Sports Medicine, 37(4), 565–579. https://pmc.ncbi.nlm.nih.gov/articles/PMC6239093/
Professional Scope of Practice *
The information herein on "Traumatic Brain Injury: Importance of Early Treatment" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card