Spinal decompression surgery could be a treatment option discussion with a doctor to relieve nerve pain brought on by a spinal condition or disorder. Everything to know about the procedures straight from the experts.
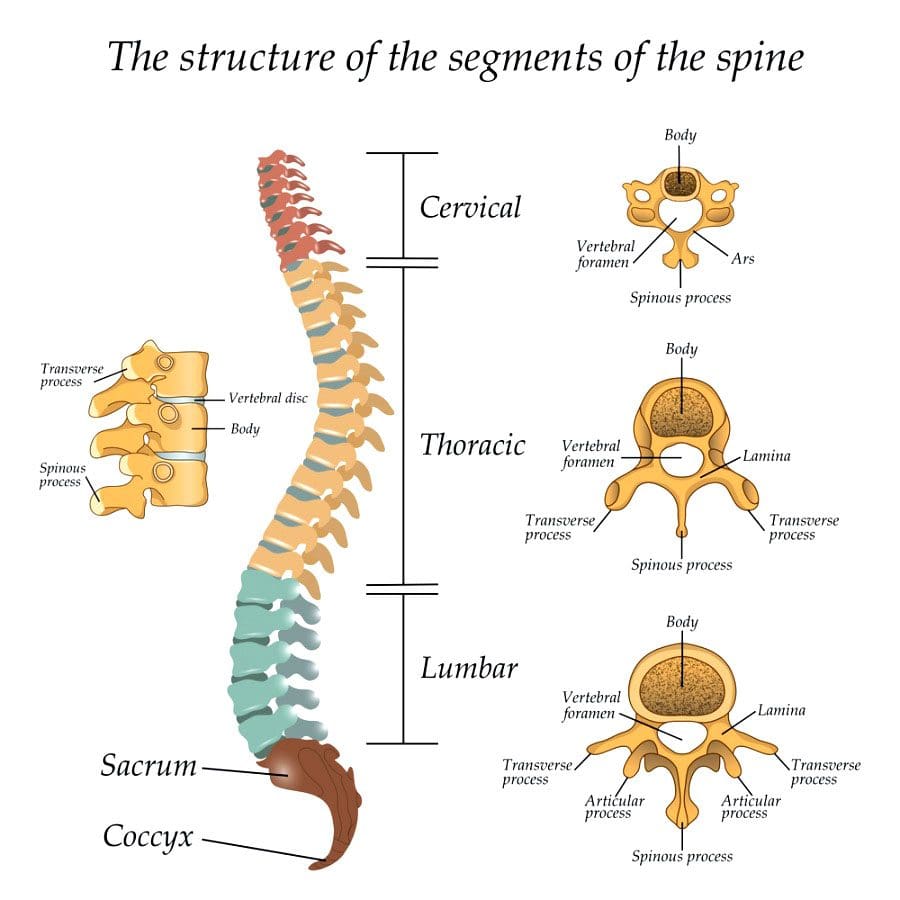
Table of Contents
Spinal Decompression Surgery Types: Laminectomy or Laminotomy
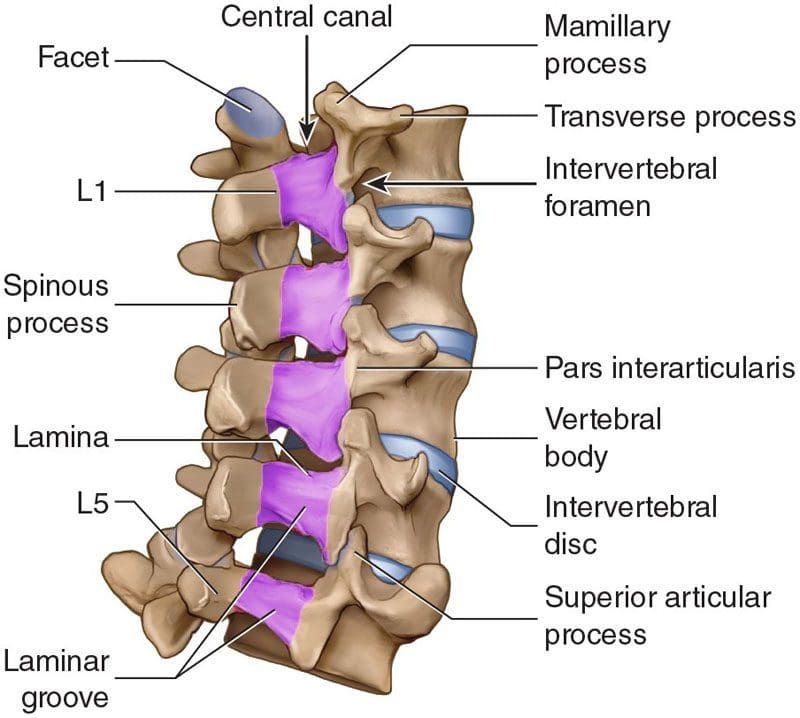
Both procedures involve the vertebrae’s lamina, which is an arch of bone that protects the spinal canal.
- In a laminectomy, the lamina is removed almost entirely.
- In a laminotomy, it is a partial removal.
Despite the removal, the large muscles of the back provide sustained protection for the nerves below. Therefore, the spinal nerves are still safe and secure following the procedures. Which one is right depends on the situation.
- A laminectomy is usually performed to treat an arthritic condition of the spinal canal like spinal stenosis.
- Laminotomy is used almost exclusively to remove a herniated disc.
- A laminectomy removes more bone and sometimes the inner edge of the facet joint.
- Ultimately, a surgeon will determine which of the two procedures is best for the individual’s needs and condition.
Decompression Surgery
Spinal stenosis or the narrowing of the spinal canal is usually caused by arthritis and overgrowth of the discs and joints. Similar compression issues respond well to non-surgical treatment. But sometimes surgery is necessary to treat uncommon but potentially severe cases. These include patients with:
- Bowel or bladder problems caused by the pressure on the spinal nerves
- Leg weakness that gets worse
- Inability to walk or move for long periods and distance
The objective of spinal decompression surgery is to create space around the spinal cord and surrounding nerves by removing the compressing structure/s. When the cord and/or nerve/s are compressed, physical and neurological symptoms are experienced down the nerve’s pathway. This includes:
- Tingling
- Numbness
- Electric shock sensations
- Radiating/spreading pain
- Weakness
Once the compressed nerves have space to relax and move around symptoms subside.
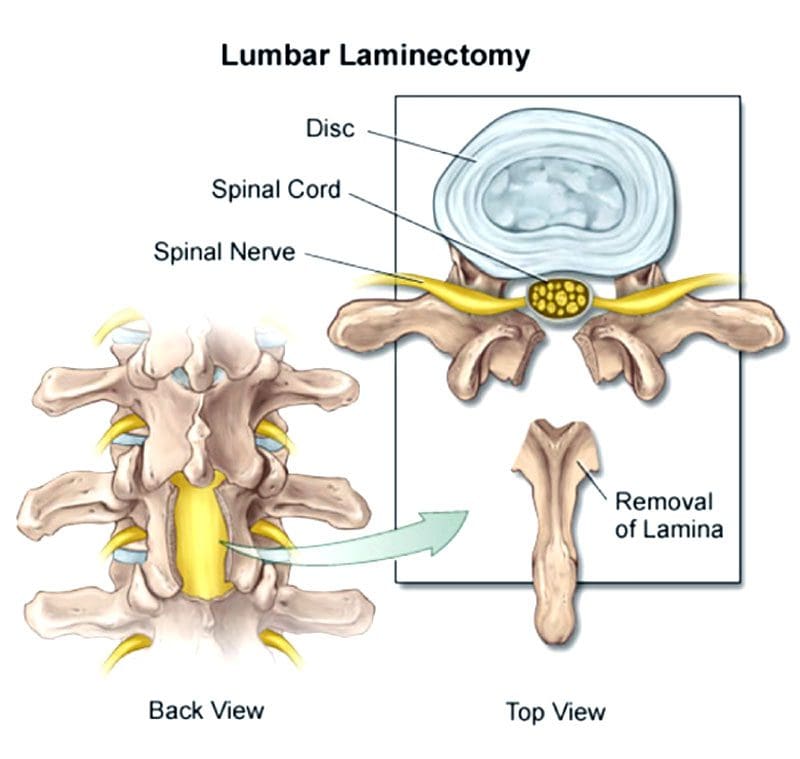
Laminectomy process
- Lumbar laminectomy is the most common procedure to treat spinal stenosis in the low back.
- It also helps treat herniated discs by allowing the surgeon to easily access the discs to repair any damage.
- The surgeon removes the lamina and ligaments that have thickened and are causing problems to create more space in the canal.
- The surgery enlarges the spinal canal so that pressure is relieved.
- By removing the source of the pressure, the pain caused by the compressed nerves is alleviated.
- An open laminectomy creates an incision of a couple of inches and exposes the spine.
- The muscles of the spine and back are cut through to expose the bone.
- Another technique that surgeons utilize is operating through a tube.
- They’ve adapted these techniques to be able to decompress both the right and the left sides although they are only operating on one side.
- Both procedures, minimal and traditional accomplish the same goals.
- The difference is the minimally invasive approach involves one or more tiny incisions also known as skin punctures and small instruments designed to separate muscles and soft tissues instead of cutting through them.
- The traditional approach requires a larger incision and instruments that retract, separate and cut tissues.

Laminectomy surgery
- Laminectomies are performed under general anesthesia using a posterior approach/lying face down during the procedure.
- It can be open or minimally invasive sometimes called a microlaminectomy.
- In an open laminectomy, the surgeon makes an incision near the affected spinal area.
- Once the incision is made, a retractor will move the skin, fat, and muscles to the side so the surgeon can access the spine.
- Next, they remove or trim the lamina and thickened ligaments to enlarge the space surrounding the compressed nerves.
- Once done, the retractor is removed and the incision is closed with sutures.
- Minimally invasive surgery or MIS is performed using special instruments like endoscopes and tubular retractors.
- These instruments allow for smaller incisions and less cutting.
- They will also use special eyewear to have a detailed view of the surgical field.
- Sometimes, the surgeon uses an endoscope or a microscope focused down the tube to perform the surgery.
- The portion of the lamina is removed, along with any bone overgrowths/osteophytes and ligament tissue.
- The tubular retractors are taken out so the soft tissue moves back into place, and the incision is closed with dissolving sutures.
Other spinal procedures performed alongside
Laminectomies and laminotomies are typically not performed together. However, a surgeon could perform both if the surgery affects multiple levels of the spine. They can also be combined with other spinal surgeries, that include:
Foraminotomy
- A foraminotomy is also a decompression procedure. But instead of removing part or all the lamina, the surgeon accesses the nerves through the spine’s foramen or the passageway that nerves pass through on both sides.
Discectomy
- This decompression surgery involves the removal of all or part of the damaged intervertebral disc and is utilized for herniated discs.
Spinal fusion
- Fusion is often performed after spinal decompression surgery, as the space that was created by removing spinal structure/s can cause instability to the spine.
Candidates for spinal decompression surgery
Both are common procedures performed by neurosurgeons and orthopedic spine surgeons. Laminectomies are considered one of the most effective treatments for spinal stenosis and spinal canal issues like:
- Tumors
- Certain types of infections and abscesses
- Spinal issues involving bowel/bladder dysfunction
- The primary reason for laminectomy is spinal stenosis, most common in individuals over the age of 60.
Other considerations and conditions include:
- Non-invasive treatments that don’t improve the condition that includes medication, massage, and physical therapy
- Fusion surgery failure
- Injection treatment failure
- The presence of tumors in or around the spine
- An infection like an epidural abscess
- Neurologic issues
- Bowel or bladder dysfunction
- Cauda equina syndrome
Ask questions about the procedure to ensure you are comfortable with the operation. Here are some questions:
- What are the risks associated?
- Will the surgery relieve all symptoms?
- Not having the surgery risks?
- What is recovery like?

Recovery
- Open or micro, recovery does take time. Following the doctor’s instructions carefully are essential to make a full, healthy recovery.
- Individuals should be careful for about a month following the surgery. But does not mean laying down or being sedentary. Movement is crucial to recovery.
- The patient should not stay in bed or lie on the sofa.
- Wait a week or two before beginning physical therapy if necessary.
- Most will have a weak core, poor posture, and poor body mechanics, the goal is to help develop and strengthen these areas.
Things to help with recovery include:
- Ice/cold packs will help reduce swelling and pain.
- Try not to sit for too long, as sitting is the least comfortable position after back surgery.
- Body mechanic awareness means avoiding too much bending or lifting and using the right body mechanics when bending or lifting.
- Post-operative body movement after surgery is vital and helps prevent post-surgery issues.
Things to do before surgery:
Quitting smoking
- Especially before surgery. Quitting entirely or at least for at least six weeks before surgery will make recovery easier and healthier.
Losing weight
- Speak with a doctor about weight. Just 5 pounds can make a significant difference during recovery.
Blood sugar
- For individuals with diabetes, having an A1C under eight before surgery is ideal.
Every patient’s recovery is different. Recovery time depends on:
- The complexity of the surgery
- Personal medical history
- Health issues
Recovery typically takes about two to four weeks after the surgery. However, it depends on the reason/s for the surgery.
Questions
Post-laminectomy syndrome
- Post-laminectomy syndrome PLS also known as failed back surgery syndrome is a condition where an individual continues to have pain after surgery. Individuals still having symptoms after should speak with their doctor to determine the next phase of treatment.
How long before exercise?
- Returning to the gym or getting into an exercise routine will take some time. It is important to follow the doctor’s recommendations and complete the full course of physical therapy before regular exercise activity can resume. Discuss workout plans with the doctor to determine the best timeline for the spine.
Full recovery?
- Returning to some activity is possible around four weeks after surgery. Full recovery takes longer as each patient’s recovery is unique. Depending on the complexity of the surgery, most return to all activities within 6 to 9 months.
Body Composition Spotlight
Dr. Alex Jimenez’s Blog Post Disclaimer
The scope of our information is limited to chiropractic, musculoskeletal, physical medicines, wellness, and sensitive health issues and/or functional medicine articles, topics, and discussions. We use functional health & wellness protocols to treat and support care for injuries or disorders of the musculoskeletal system. Our posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate and support directly or indirectly our clinical scope of practice.*
Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We also make copies of supporting research studies available to the board and or the public upon request. We understand that we cover matters that require an additional explanation as to how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. The provider(s) Licensed in Texas& New Mexico*
References
American Association of Neurological Surgeons. “Minimally Invasive Spine Surgery.” (n.d.) https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Minimally-Invasive-Spine-Surgery
Foraminotomy. MedlinePlus. https://medlineplus.gov/ency/article/007390.htm. Reviewed November 27, 2016. Page last updated December 21, 2017. Accessed January 18, 2018.
Laminectomy. https://medlineplus.gov/ency/article/007389.htm. MedlinePlus. Reviewed November 27, 2016. Page last updated December 21, 2017. Accessed January 18, 2018.
Mayo Clinic. “Laminectomy.” (n.d.) https://www.mayoclinic.org/tests-procedures/laminectomy/about/pac-20394533
Mayo Clinic. “Laminotomy.” (n.d) https://www.mayoclinic.org/diseases-conditions/spinal-stenosis/multimedia/img-20149227
Professional Scope of Practice *
The information herein on "Spinal Decompression Surgery: Laminotomy and Laminectomy" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card













