A typical sandwich from home includes bread – one thick slice of whole wheat, one or two favorite condiments, lunch meat, lettuce, tomato, and pickles. Packing a homemade lunch to work or school is one of the easiest ways to lose and maintain weight. Making a sandwich means the ingredients, calories, and nutrition can be controlled. However, a healthy sandwich can easily exceed calories if not careful. Bread choices and condiments like mayonnaise, dressings, and cheese can change a sandwich’s nutrition and increase calories, fat, and sodium. Calories can be cut with smart nutrition information and a few recommendations.
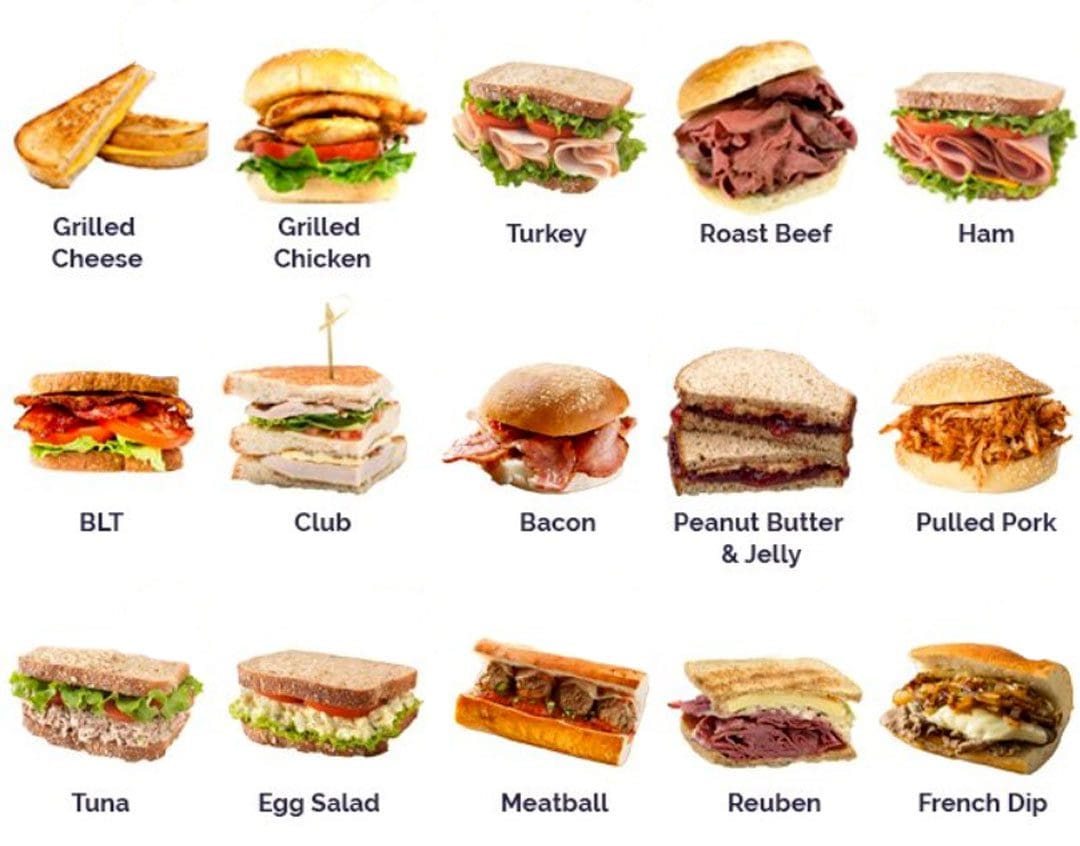
Table of Contents
Sandwich Nutrition Facts and Health Benefits
Sandwich Calories and Nutrition
USDA nutrition information for one sandwich with ham, cheese, and mayonnaise equals 155 grams.
- Total Calories 361
- Fat 16.7 grams
- Sodium 1320 milligrams
- Carbohydrates 32.5 grams
- Fiber 2.3 grams
- Sugars 5.1 grams
- Protein 19.3 grams
Favorites
The calories can vary based on the bread, fillings, and spread used to make it and whether vegetables are added.
Peanut Butter
- Calories 200 – 300.
- Peanut butter on white bread.
- A single serving of peanut butter is two tablespoons.
Peanut Butter and Jelly
- Calories 350 – 500.
- Depending on how much peanut butter is used and the type of jelly or jam.
Nutella
- Calories 300 – 500.
- A 2-tablespoon serving is 200 calories.
Turkey Sandwich
- Calories 160 – 500.
- Depending on the amount of meat added and condiment choices.
Ham
- Calories less than 200.
- This is without the cheese.
- With butter on French bread, it can be 400 calories or more.
Chicken Salad
- Calories 400 – 600 or more.
Egg Salad
- Calories 350 for the mayonnaise filling, plus around 150 for the bread.
Egg and Cheese
- Calories 250 -400 or more.
- If made on a biscuit or croissant.
Subway
- 230 to nearly 1000 calories.
Cut Calories
With a few adjustments and healthy swaps, a nutritious and healthy sandwich that is lower in calories but full of flavor can be made.
Low-Calorie Bread
- Thick, crusty bread, bagels, baguettes, croissants, and hearty rolls can contain fat and calories.
- Instead, choose a whole grain or bread alternative with additional nutrient benefits like healthy fats or fiber.
- Consider an open-faced sandwich for heartier bread and keeping the portion to one slice.
- Make a sandwich without bread and wrap the filling in lettuce or other bread substitutes.
Leaner Fillings
Once a healthy bread is chosen, build the sandwich around a meat or meat-free filling. Get creative and try different choices to find new flavors. Read labels of meat or fish spreads that sound healthy. Many brands may contain protein and beneficial nutrients, but the filling is often combined with other ingredients high in calories. Try for:
- Deli ham sliced thin.
- Deli turkey sliced thin.
- Deli roast beef sliced thin.
- Deli-style rotisserie chicken breast sliced thin.
- Look for low-sodium meats.
- Grilled eggplant.
- Grilled portobello mushroom.
Nutrient-Rich Vegetables
Pack the sandwich with natural toppings like vegetables. Make a goal to have at least two vegetable servings per sandwich. Nutrient-rich vegetables add flavor and crunch to the sandwich.
- Iceberg lettuce, spinach, romaine lettuce, or greens.
- Shredded cabbage.
- Tomato.
- Sun-dried tomatoes.
- Cucumber.
- Jalapeno peppers.
- Banana peppers.
- Green peppers.
- Plain or grilled onions.
- Basil leaves.
- Bean sprouts.
Low-Calorie Condiments
The spread takes up the least space on a sandwich but can contain the most fat. Condiments should be used moderately.
- Olive oil
- Butter
- Aioli
- Tahini
- Pesto
- Salad dressing
- Jelly
- Avocado
- Guacamole
- Olive tapenade
- Barbecue sauce
- Relish
- Ketchup
- Dijon mustard
- Yellow mustard
When first starting, cutting sandwich calories might seem complicated and unfamiliar. Fill the refrigerator with as many healthy choices as possible, get creative, and see what you come up with, as crafting a delicious meal is fun once you get the hang of it.
Body In Balance, Fitness, and Nutrition
References
An, R et al.” Sandwich consumption concerning daily dietary intake and diet quality among U.S. adults, 2003-2012″ Public Health vol. 140 (2016): 206-212. doi:10.1016/j.puhe.2016.06.008
Sebastian, Rhonda S., et al.” Sandwich Consumption by Adults in the U.S. What We Eat In America, NHANES 2009-2012″ FSRG Dietary Data Briefs, United States Department of Agriculture (USDA), December 2015.
U.S. Department of Agriculture, Agricultural Research Service. FoodData Central. [Historical Record]: Ham and Cheese.
U.S. Department of Agriculture, Agricultural Research Service. FoodData Central [Historical Record]. Whole Wheat Bread.
Zhao Z, Feng Q, Yin Z, et al. Red and processed meat consumption and colorectal cancer risk: a systematic review and meta-analysis. Oncotarget. 2017;8(47):83306-83314. doi:10.18632/oncotarget.20667