For individuals dealing with musculoskeletal pain, can incorporating acupuncture and dry needling therapy improve functionality?
Table of Contents
Introduction
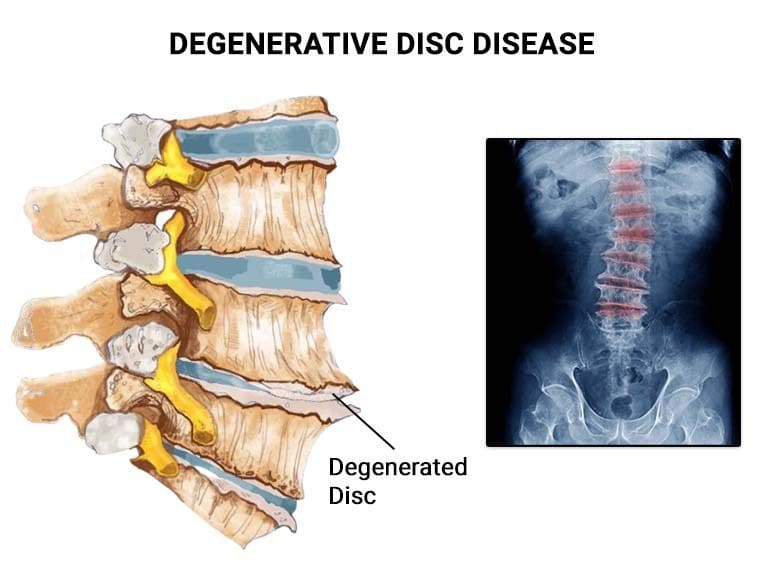
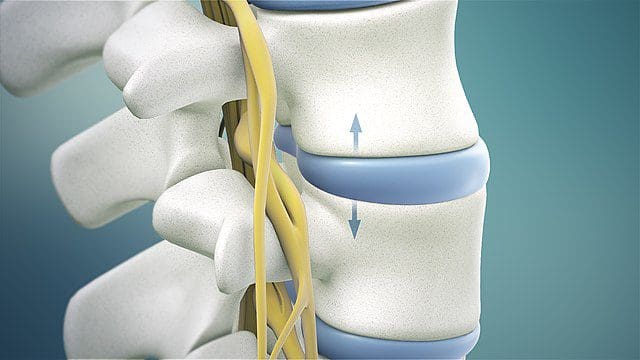
All around the world, many individuals have experienced musculoskeletal pain at one point in their lives. Musculoskeletal pain can range from acute to chronic, depending on how severe the affected muscles are in pain. Sometimes, when a person is dealing with pain in one location and feels it in a different body location, that is known as referred pain, and it can lead to overlapping risk profiles. Additionally, many individuals dealing with musculoskeletal pain are often associated with various environmental factors that contribute to its development or have traumatic injuries that causes the spine to be out of alignment with the body. When it comes to treating musculoskeletal pain, many individuals will do home remedies that can provide temporary relief until the pain flares up again. When that happens, many will seek treatment to reduce the pain-like effects and find the relief they are looking for. Today’s article examines two treatments, their benefits, and how they can reduce musculoskeletal pain. We talk with certified medical providers who consolidate our patients’ information to provide numerous treatments to minimize musculoskeletal pain affecting their bodies. We also inform and guide patients on how various treatments can be beneficial to their health and wellness as they can help reduce musculoskeletal pain. We encourage our patients to ask their associated medical providers intricated and important questions about the referred pain-like symptoms they are experiencing from musculoskeletal pain that is causing them pain and discomfort. Dr. Jimenez, D.C., incorporates this information as an academic service. Disclaimer.
What Is Acupuncture?
Do you wake up in the morning feeling general aches and pains in various muscle locations? Do you feel muscle stiffness in your neck, shoulders, or back after a long, hard workday? Or have you experienced pain-like symptoms like numbness or radiating burning sensations in your upper or lower body extremities? In these pain-like scenarios, many individuals are experiencing musculoskeletal pain once in their lives. This usually happens when environmental factors or traumatic injuries occur in the musculoskeletal system, causing the surrounding muscles, ligaments, and tissue to be overstretched, tight, or weakened, depending on the severity. When a person is dealing with musculoskeletal pain, they will seek treatments to reduce the musculoskeletal pain and be affordable and customizable to the individual’s pain, hence why non-surgical therapies can benefit the person dealing with musculoskeletal pain.

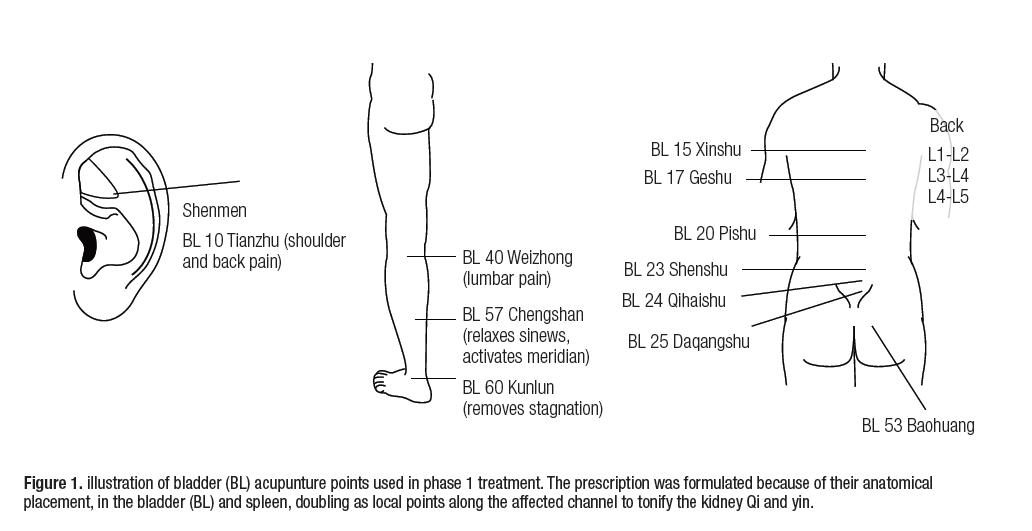
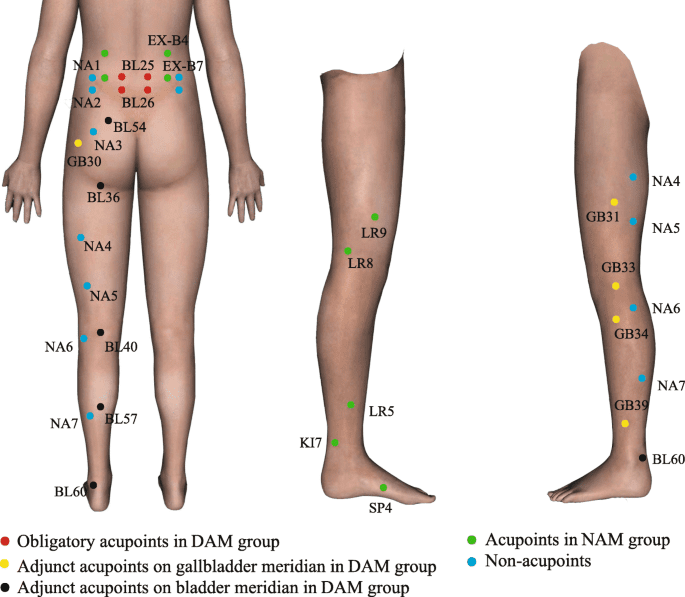
One of the oldest forms of non-surgical treatment is acupuncture, which can help reduce musculoskeletal pain. Acupuncture has been practiced in China for over two thousand years by modulating the body’s physiology by stimulating specific body regions or acupoints. (Wang et al., 2023) Acupuncture incorporates thin, solid needles used by highly trained medical professionals to restore the balance of qi or energy flowing through the body while positively affecting the central and peripheral nervous system. To that point, by changing pain perception, acupuncture can help reduce the inflammatory cytokines associated with musculoskeletal pain. (Kelly & Willis, 2019)
Acupuncture Benefits
Some of the benefits that acupuncture can help a person dealing with musculoskeletal pain include:
- Release tight muscles.
- Inflammation reduction
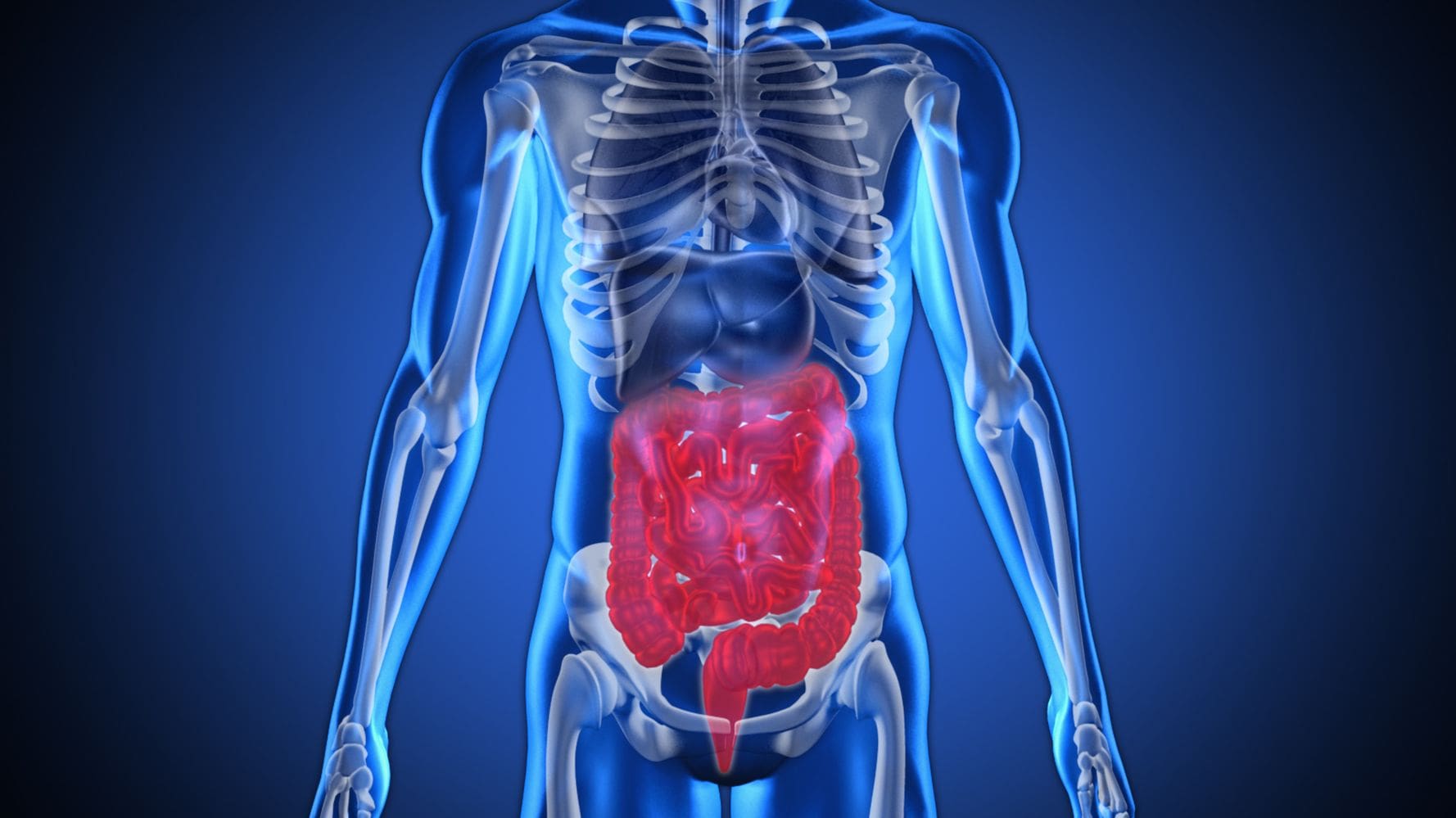
- Regulate gut activity associated with musculoskeletal pain.
- Improve pain and disability.
Since pain is a common indication for acupuncture, acupuncture for individuals experiencing musculoskeletal pain can help enhance the descending inhibitory effects while modulating the feelings of pain, which, to this point, modify central sensitization. (Zhu et al., 2021) This, in turn, helps many individuals experience positive effects from musculoskeletal pain reduction in their bodies.
What Is Dry Needling?
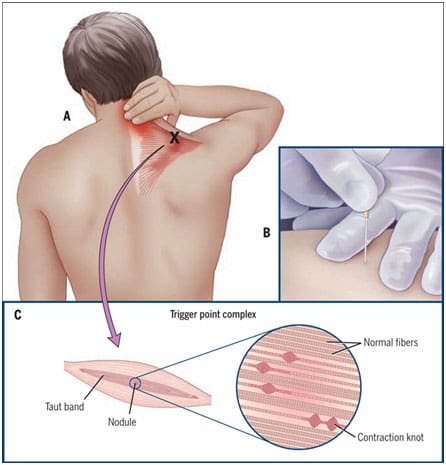
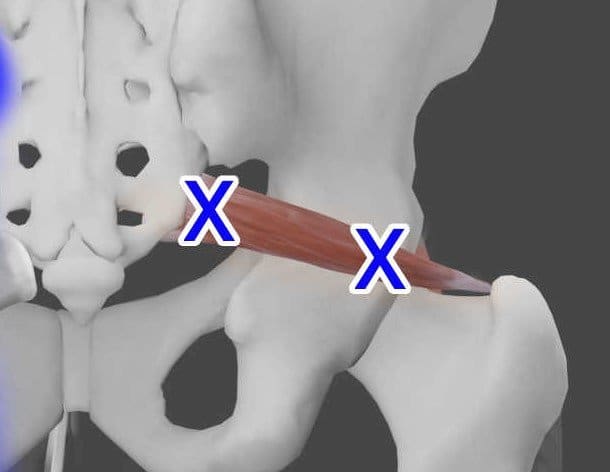
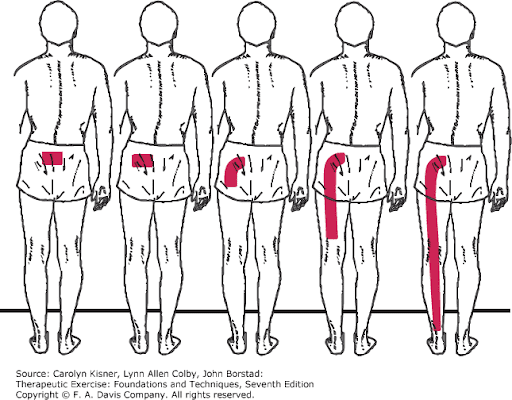
Dry needling is a different form of acupuncture that combines TCM (traditional Chinese medicine) and structural manipulation of the affected muscles experiencing pain. Dry needling is safe and, like acupuncture, cost-effective. It reduces pain and improves fascial and scar tissue mobility back to the muscle. (Munoz et al., 2022) At the same time, dry needling is used by highly trained professionals to treat soft tissues and neurovascular bundles correlated with numerous neuromusculoskeletal pain syndromes by inserting fine monofilament needles and stimulating specific reactions in the targeted tissue. (Lara-Palomo et al., 2022)
Dry Needling Benefits
Dry needling can help reduce musculoskeletal pain symptoms associated with myofascial pain syndrome by mechanically disrupting the trigger points to elicit a local twitch response. (Lew et al., 2021) Some of the benefits that dry needling provides include:
- Decrease muscle tightness.
- Pain reduction
- Joint and muscle mobility
- Increase blood flow.
How Acupuncture & Dry Needling Help With Pain?
Depending on how severe the individual’s pain is affecting their daily life, they can choose either acupuncture or dry needling and combine them with other non-surgical therapies to reduce the chances of musculoskeletal pain from causing overlapping risk profiles that can make a person’s life miserable. Both non-surgical techniques can be effective with patients dealing with musculoskeletal pain, improve stiffness and fatigue, and enhance quality of life. (Valera-Calero et al., 2022) Incorporating these non-surgical treatments to reduce musculoskeletal pain with healthy habits can give helpful results to the individual by making small changes in their everyday lives and being mindful of their bodies. This allows them to reduce the chances of musculoskeletal pain and its associated factors from recurring again in the future.
Revolutionizing Healthcare- Video

References
Kelly, R. B., & Willis, J. (2019). Acupuncture for Pain. American Family Physician, 100(2), 89-96. https://www.ncbi.nlm.nih.gov/pubmed/31305037
https://www.aafp.org/pubs/afp/issues/2019/0715/p89.pdf
Lara-Palomo, I. C., Gil-Martinez, E., Antequera-Soler, E., Castro-Sanchez, A. M., Fernandez-Sanchez, M., & Garcia-Lopez, H. (2022). Electrical dry needling versus conventional physiotherapy in the treatment of active and latent myofascial trigger points in patients with nonspecific chronic low back pain. Trials, 23(1), 238. https://doi.org/10.1186/s13063-022-06179-y
Lew, J., Kim, J., & Nair, P. (2021). Comparison of dry needling and trigger point manual therapy in patients with neck and upper back myofascial pain syndrome: a systematic review and meta-analysis. J Man Manip Ther, 29(3), 136-146. https://doi.org/10.1080/10669817.2020.1822618
Munoz, M., Dommerholt, J., Perez-Palomares, S., Herrero, P., & Calvo, S. (2022). Dry Needling and Antithrombotic Drugs. Pain Res Manag, 2022, 1363477. https://doi.org/10.1155/2022/1363477
Valera-Calero, J. A., Fernandez-de-Las-Penas, C., Navarro-Santana, M. J., & Plaza-Manzano, G. (2022). Efficacy of Dry Needling and Acupuncture in Patients with Fibromyalgia: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health, 19(16). https://doi.org/10.3390/ijerph19169904
Wang, M., Liu, W., Ge, J., & Liu, S. (2023). The immunomodulatory mechanisms for acupuncture practice. Front Immunol, 14, 1147718. https://doi.org/10.3389/fimmu.2023.1147718
Zhu, J., Li, J., Yang, L., & Liu, S. (2021). Acupuncture, from the ancient to the current. Anat Rec (Hoboken), 304(11), 2365-2371. https://doi.org/10.1002/ar.24625