Understand the complexities of developmental disorders and learning disabilities and how they affect individuals uniquely.
Introduction To Developmental Disorders
When talking about disabilities, whether from health conditions or diseases, many healthcare professionals have to think about two languages crucial to the individual they are assessing. One is person-first language, and the other is identity language. In person-first language, it pertains to how a person places more importance on the individual and their uniqueness. This involves individuals young and old with ADHD or Down syndrome. This is compared to the identity-first language, which often highlights the disorder or disease more than the individual (e.g., autistic child). The goal that many healthcare professionals aim for when treating individuals with disabilities or developmental disorders is to use respectful terminology to reduce social stigma, prejudice, and discrimination.
Many young individuals have their cognitive and social skills evaluated when entering and progressing through school. These evaluations sometimes indicate that a young individual or children might need special assistance with either language or learning to interact with others. Evaluation and diagnosis are the first steps in providing many people with the tools and resources needed to function. However, there are also significant social implications regarding diagnosis and labeling. Many healthcare providers must consider that anyone, young or old, can be misdiagnosed. Once the person receives the diagnosis label, the individual and whoever is in the person’s life have to interpret the person’s actions through that label. For instance, if a child has been misdiagnosed as having a learning disability, it can influence the child’s self-concept. It may be due to difficulties in school that cause children to have trouble at their academic level. This self-fulfilling prophecy causes them to act this way, causing people to predict what will happen come true. Healthcare professionals must pay attention to the power of labels and apply them accurately when assessing patients.
It is also important to consider that people’s difficulties can change over time. An example would be a child who has problems in school that may improve later or grow up to be an adult where these problems are no longer relevant. That person, however, will still have a label for having a learning disability. Even though it is fairly common for children and young individuals to have abnormal behaviors, healthcare providers should recognize that the distinction between abnormal/atypical and normal/typical behavior is not always clear. When evaluating learning disabilities, misdiagnosis may be more of a concern.
When it comes to the diagnosis of developmental disabilities, it is required that a pediatrician, psychologist, psychiatrist, or other accredited professional should assess a child for a developmental disability, as there are many factors to consider. Many common behaviors in children, like temper tantrums, being overly active, being shy, etc., might be misinterpreted as a behavioral disorder like ADHD (attention-deficit/hyperactivity disorder). Therefore, trained professionals use multiple assessments or questionnaires completed by the parent(s) and teacher(s) in conjunction with in-person observations and case history before diagnosing.
Autism Spectrum Disorders
As a common developmental disorder, autism spectrum disorder (ASD) can affect various areas of development, such as communication and behavior, in many individuals. The spectrum is wide and varies from person to person. In the United States, it is estimated that about 1 out of every 36 children or individuals has been diagnosed with autism, covering a wide variety of abilities and symptom expression between high and low functioning. ASD is characterized by age-inappropriate, impaired social communication and may have a complex interaction between genetics, epigenetic, and environmental factors associated with cerebral dysfunction. (Mukherjee, 2017) When it comes to social skills and communication, ASD can impact a person’s language skills as it can become difficult. A person within the autism spectrum may respond to a question by repeating the question, may not respond appropriately, or may not communicate in response at all. Some symptoms for an individual within the autism spectrum may be sensitivity to touch, sound, or visual stimulation. Individuals with autism often view the world differently and learn in unique ways while preferring routines and can become upset when routines are altered. For example, moving furniture or changing the daily schedule can be very upsetting.
There is no single known cause of autism, though research has indicated a possible genetic link. This could be due to the intricate neurobiological mechanisms that correlate with the immune system and neuroinflammation, causing atypical functional connectivity and neurotransmitter alterations. (Rajabi et al., 2024) Luckily, there are holistic approaches to reducing autism symptoms to help improve a person’s quality of life within the spectrum.
Holistic Treatments For Individuals Within The Autism Spectrum
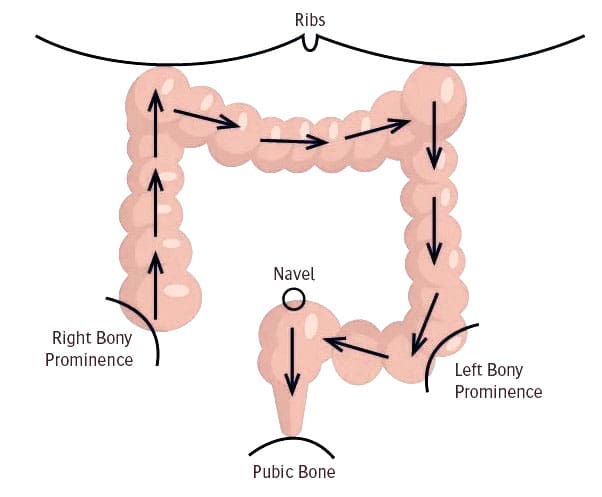
When it comes to holistic treatment approaches for individuals with autism, they can vary for the individual while not affecting their sensory issues. Physical activities and motor skill training can help their mobility and improve movement performance. (Shahane et al., 2024) Additionally, individuals within the autism spectrum could be dealing with abnormal sensitivity and gastrointestinal difficulties that can cause numerous pain-like symptoms in the body. Incorporating and allowing autistic individuals to try out anti-inflammatory foods and prebiotics can help improve the symptoms associated with ASD while reducing the inflammatory effects on their bodies. (Sivamaruthi et al., 2020)
What Are Learning Disabilities?
When a person, both young and old, has an intellectual disability or an intellectual development disability, they could have significant impairment in intellectual and adaptive functioning. This, in turn, generally results in an IQ (intelligence quotient) under 70, which is two standards below the median. This causes deficits within two or more adaptive behaviors that affect everyday general living, causing them to learn slowly in all areas of learning. This is known as learning disabilities.
A learning disability (LD) is a specific impairment of academic learning that interferes with a particular aspect of schoolwork and significantly reduces a person’s educational performance. It can be shown as a major discrepancy between a person’s ability and some achievement features, causing them to be delayed in various academic areas. Many people often confuse the difference between a learning problem and a learning disability, as a learning problem stems from physical, sensory, or motor handicaps or generalized intellectual impairment.
Dyslexia
One of the most prevalent learning disorders, dyslexia is characterized by difficulties reading; fundamentally, many dyslexics struggle to learn how to spell and interpret words and become proficient in phonological representation. (Snowling & colleagues, 2020) The reason for this is because a number of anatomical alterations in the brain impair the brain’s capacity to integrate data from various RSNs (resting state networks), which lessens the neuroplasticity of the brain. In 2020, Munzer et al. There are reading experts in several therapies to aid with the troublesome regions of the patient.
Dysgraphia
Writing disabilities like dysgraphia are often linked to dyslexia. It is sometimes used as a general term for all impairments of written language. Different forms of dysgraphia include orthographic dysgraphia and phonological dysgraphia. When a person has phonological dysgraphia, they are unable to write words using their phonemes. On the other hand, people with orthographic dysgraphia are able to spell words that are spelled consistently but not erratically. When using a pen or pencil, some people with dysgraphia may have issues making letters and with motor control.
Dyscalculia
The inability to absorb arithmetic concepts (such number, place value, and time), retain math information, and comprehend how problems are structured on paper are all symptoms of dyscalculia, a kind of math-related impairment. As a result, many students end up having bad school experiences and consistently failing at arithmetic assignments, which breeds failure anxiety and lowers self-esteem. Harris and Schulte-Korne (2019) People who deal with numbers suffer from working memory problems as a result. Atypical patterns of mathematical cognitive performance may be reflected in this, since the parietal lobes may be smaller and less active. Downer (2024)
Optimizing Your Wellness-Video
Attention-Deficit/Hyperactivity Disorder (ADHD)
A neurodevelopmental disease known as attention-deficit/hyperactivity disorder (ADHD) causes problems with cognitive and motor function. This is because certain brain regions are smaller than others, which may lead to patterns of impulsive, hyperactive, and inattentive behavior. These patterns can also alter the neurotransmitters in the brain, which can disrupt regular functioning. In 2017, ADHD & The Brain
Among the symptoms of inattention are:
Task difficulty and avoiding them
Disregarding directions
Lack of organization
Ignoring details and becoming easily sidetracked
Forgetting.
Excessive movements, which are indicative of hyperactivity in ADHD, include:
Being restless
Finding it difficult to remain still
Inappropriate running and climbing on objects
Responses that are blurred out
Waiting is hard.
obstructing and disturbing other people.
Whether they are adults or toddlers, energetic people often come off as noisy. This leads to social and intellectual difficulties throughout their lives. People with ADHD often get worse grades, perform poorly on standardized tests, have greater expulsion rates, and are more likely to drop out of school during the academic year than their peers without ADHD.
Causes of ADHD
Genetics is a major factor in the development of ADHD, according to several twin and family studies. Gender, exposure to environmental variables, and the diagnosis of an ADHD subtype have all been suggested as possible modifiers of ADHD development in several studies. The Gizer group (2009) It is believed that a particular gene that regulates the neurotransmitter dopamine is implicated in ADHD. According to certain brain imaging studies, people with ADHD have anomalies in the frontal lobes, which are a region of the brain with a lot of dopamine. Individuals with ADHD will have reduced frontal brain activity during mental activities since the frontal lobe regulates behavior. Therefore, anomalies in this area might be a major factor in explaining part of the hyperactive, uncontrollable behavior associated with ADHD.
It has been believed that some environmental elements, such as sugar and artificial colors, increase an individual’s hyperactivity. In order to alleviate the symptoms of ADHD, many individuals choose to cut them down. However, there have been a lot of research comparing the effects of cigarette smoke exposure on the development of severe ADHD symptoms in the fetus. (Linnet & colleagues, 2003)
ADHD Treatment
The most widely used treatments for ADHD include stimulant medication, non-surgical therapies, and lifestyle modifications that may help lessen the symptoms of the disorder. Many people believe that using stimulant medicine is paradoxical, however it may help individuals with ADHD concentrate by activating the undeveloped areas of the brain, notably the frontal and prefrontal lobes. This in turn aids in managing ADHD’s detrimental consequences.
Both non-pharmaceutical therapies and physical exercise may enhance cognitive and motor abilities. In 2015, Ziereis and Jansen However, cognitive behavioral therapy is a popular non-surgical treatment that may help patients become more conscious of their thoughts and change them from negative to positive. A lot of medical practitioners may use both CBT and medicine in their patients’ treatment regimen. It is especially advantageous since the drug facilitates behavior change more rapidly, which speeds up the learning process for long-term behavioral changes via cognitive behavioral therapy. on order to enhance their quality of life on their path toward health and wellness, people with developmental disorders and learning impairments may have a personalized treatment plan by implementing minor adjustments and using a variety of therapy choices.
Injury Medical & Functional Medicine Clinic
We associate with certified medical providers who understand the importance of the various effects of developmental disorders and learning disabilities affecting the body. While asking important questions to our associated medical providers, we advise patients to implement small changes to their daily routine to reduce the symptoms affecting their bodies. Dr. Alex Jimenez, D.C., envisions this information as an academic service. Disclaimer.
References
ADHD & The Brain. (2017). American Academy of Child & Adolescent Psychiatry. https://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/ADHD_and_the_Brain-121.aspx
Dowker, A. (2024). Developmental Dyscalculia in Relation to Individual Differences in Mathematical Abilities. Children (Basel), 11(6). https://doi.org/10.3390/children11060623
Gizer, I. R., Ficks, C., & Waldman, I. D. (2009). Candidate gene studies of ADHD: a meta-analytic review. Hum Genet, 126(1), 51-90. https://doi.org/10.1007/s00439-009-0694-x
Haberstroh, S., & Schulte-Korne, G. (2019). The Diagnosis and Treatment of Dyscalculia. Dtsch Arztebl Int, 116(7), 107-114. https://doi.org/10.3238/arztebl.2019.0107
Linnet, K. M., Dalsgaard, S., Obel, C., Wisborg, K., Henriksen, T. B., Rodriguez, A., Kotimaa, A., Moilanen, I., Thomsen, P. H., Olsen, J., & Jarvelin, M. R. (2003). Maternal lifestyle factors in pregnancy risk of attention deficit hyperactivity disorder and associated behaviors: review of the current evidence. Am J Psychiatry, 160(6), 1028-1040. https://doi.org/10.1176/appi.ajp.160.6.1028
Mukherjee, S. B. (2017). Autism Spectrum Disorders – Diagnosis and Management. Indian J Pediatr, 84(4), 307-314. https://doi.org/10.1007/s12098-016-2272-2
Munzer, T., Hussain, K., & Soares, N. (2020). Dyslexia: neurobiology, clinical features, evaluation and management. Transl Pediatr, 9(Suppl 1), S36-S45. https://doi.org/10.21037/tp.2019.09.07
Rajabi, P., Noori, A. S., & Sargolzaei, J. (2024). Autism spectrum disorder and various mechanisms behind it. Pharmacol Biochem Behav, 245, 173887. https://doi.org/10.1016/j.pbb.2024.173887
Shahane, V., Kilyk, A., & Srinivasan, S. M. (2024). Effects of physical activity and exercise-based interventions in young adults with autism spectrum disorder: A systematic review. Autism, 28(2), 276-300. https://doi.org/10.1177/13623613231169058
Sivamaruthi, B. S., Suganthy, N., Kesika, P., & Chaiyasut, C. (2020). The Role of Microbiome, Dietary Supplements, and Probiotics in Autism Spectrum Disorder. Int J Environ Res Public Health, 17(8). https://doi.org/10.3390/ijerph17082647
Snowling, M. J., Hulme, C., & Nation, K. (2020). Defining and understanding dyslexia: past, present and future. Oxf Rev Educ, 46(4), 501-513. https://doi.org/10.1080/03054985.2020.1765756
Ziereis, S., & Jansen, P. (2015). Effects of physical activity on executive function and motor performance in children with ADHD. Res Dev Disabil, 38, 181-191. https://doi.org/10.1016/j.ridd.2014.12.005
Disclaimer




 Digital Pulleys
Digital Pulleys










 Causes
Causes